Scoliosis Treatment in Adults – Is It Possible to Avoid Scoliosis Surgery?
©Regeneex
Scoliosis, or a side bending of the spine, is one of those diseases that kind of sneaks up on patients. So let’s take a look at what we know about this disease, scoliosis treatment in adults, what we know works, and whether patients can realistically avoid scoliosis surgery.
What is Scoliosis? What Causes it?
Pikovit/Shutterstock
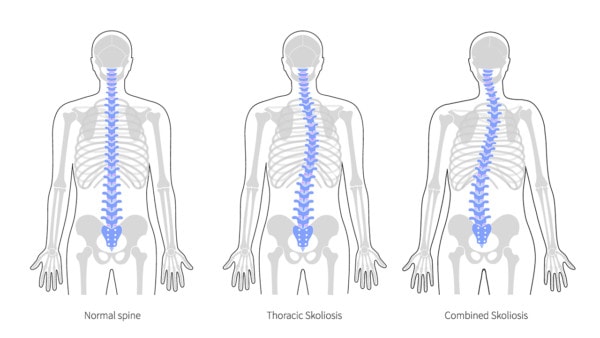
Scoliosis is a side bending of the spine. We all take for granted that our bodies were built to be symmetrical with the left being like the right. The normal spine mirrors that in providing a symmetrical base of support. However, sometimes the spine can bend sideways, which is known as scoliosis. Many people acquire mild degenerative scoliosis as they age, but a few get more severe side bending at an early age. When this happens, it’s called adolescent idiopathic scoliosis (AIS) (1).
So what do we know about this problem? About 80% of the causes of AIS are never identified (2). We also know that there is only a small percentage of adolescents with a more significant curve of over 10 degrees (3). Women tend to have larger scoliotic curves than men (4). The larger the curve and the earlier it’s found, the higher the likelihood for progression or worsening of that curve over time (5). For the vast majority of AIS patients, there are no severe health consequences involving the lungs or heart (6). In addition, long-term studies have found that most AIS patients function well as they age (7).
Older people can develop scoliosis as they age or patients with AIS obviously age over time. The former is called degenerative scoliosis and about 1/3 of the elderly population have this problem (8). This normally occurs due to the discs that separate the vertebra collapsing more on one side than the other or imbalances in the body.
Measuring Scoliosis Severity: The Cobb Angle
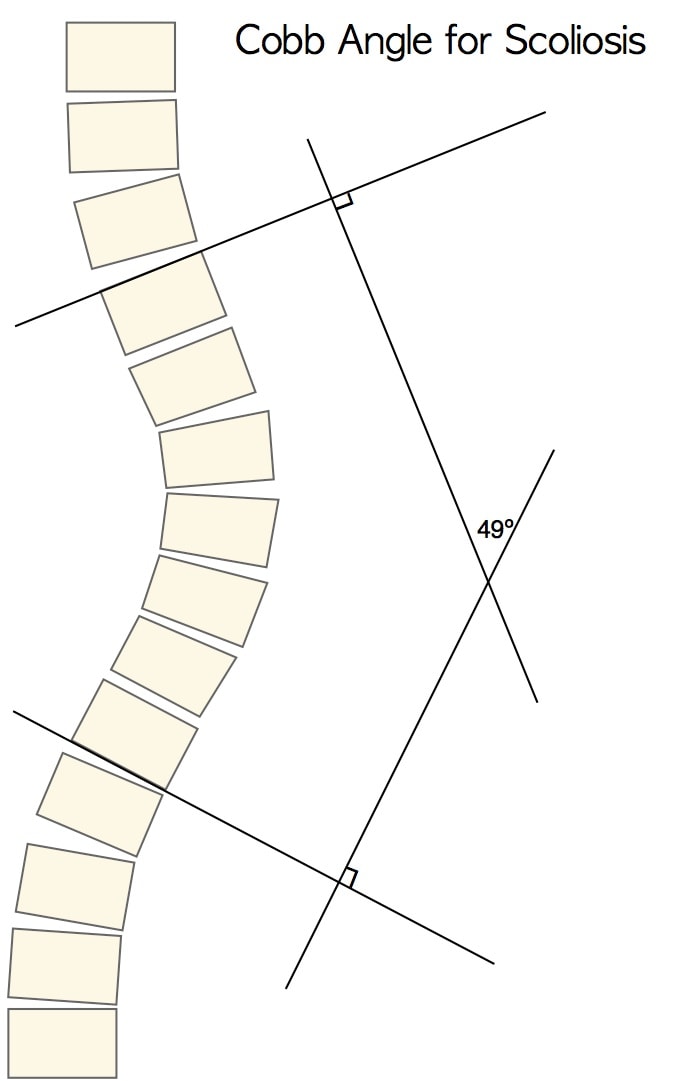
- Scoliosis-specific exercises (15 – 25° Cobb)
- Bracing (20 – 40° Cobb)
- Spinal fusion surgery (> 40 – 50° Cobb)
Hence, for smaller curves, exercise therapy is often prescribed. For medium curves, bracing is used. Finally, for severe curves, surgery is often utilized. However, can you avoid scoliosis surgery? As I’ll explain later, we have noted that a newer treatment option involving interventional orthobiologics may make surgery less common.
Do Exercises Help? Does Surgery Help?
Exercises are one valid scoliosis treatment in adults. The most popular physical therapy type to avoid scoliosis surgery is the Schroth method which was founded in the 1920s. This involves pelvic corrections, right angular breathing, and stretching/strengthening to stabilize and correct the spine (9). High-quality studies have shown that this can be effective long-term in reducing the cobb angle (10). In addition, long-term follow-up studies have shown that AIS patients treated with either bracing or surgery had little differences in quality of life (11,12). Even in severe scoliosis patients (cobb >40 degrees) who avoided scoliosis surgery when compared to those who had the procedure, no differences were observed 8 years later (13).
If there isn’t a big difference in function between patients treated with exercises, braces, or nothing and who avoided scoliosis surgery and those who had the surgery, why are we performing these aggressive procedures? Scoliosis surgery involves taking a rod and screwing this into multiple spine bones to straighten the spine and usually to fuse the bones together. The procedure has a high rate of complications (14). These commonly include the spine bones not fusing, infection, nerve damage, and misplaced screws. Is there a better way to help patients avoid scoliosis surgery?
Percutaneous Scolioplasty
While steroid injections around nerves (epidural) and into arthritic joints (facet injections) are sometimes performed in scoliosis patients who have pain, the problem with this approach is that it isn’t functional and it likely causes tissue damage. Meaning, the goal is to identify a few spots that hurt and to inject those areas with high-dose steroids which we know can harm tissue like cartilage and bones (15).
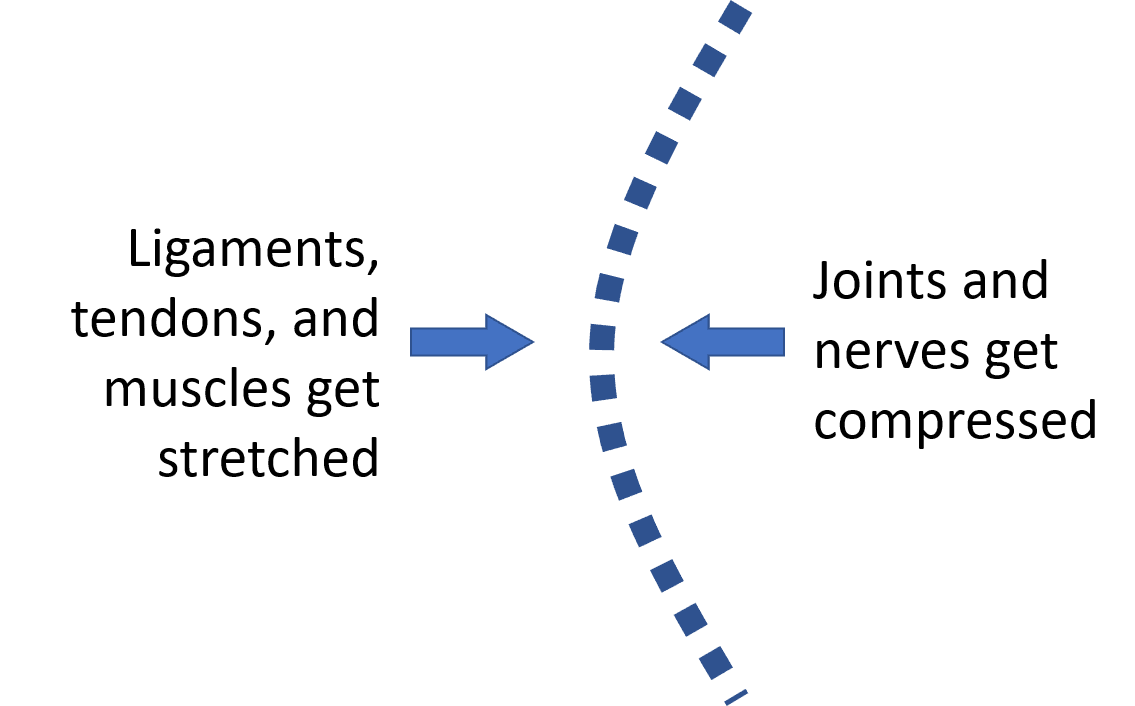
- Painful and swollen nerves and joints in areas of excessive compression
- Stretched ligaments, tendons, and muscles in areas of excessive stretch
I call this procedure, Percutaneous (perc) Scolioplasty, which is first the precise diagnosis of the areas that need help and then the precise injection using both x-ray and ultrasound guidance, of orthobiologics. While one the goal of this procedure is to reduce pain and increase function, another is to provide resistance to further sideways collapse of the spine by tightening ligaments on the convex side of the curve and stretch those due to the rotation of the vertebrae. Does it work?
My first experience with this approach was with one of our long-time dedicated employees who has AIS and never had surgery. She wanted to avoid scoliosis surgery as she got older, but by her 30s her pain was getting severe. At first, I tried spot treatments in this area like epidurals or fact injections. That approach helped some, but she continued to decline over time. So I came up with a new plan, why not target specific ligaments, tendons, muscles, nerves, and facet joints? Hence the Perc-Scolioplasty procedure was born. Our employee did much better with this approach and I began more widely applying it in my patients who were either older AIS patients to who had degenerative scoliosis.
Freyda’s Story
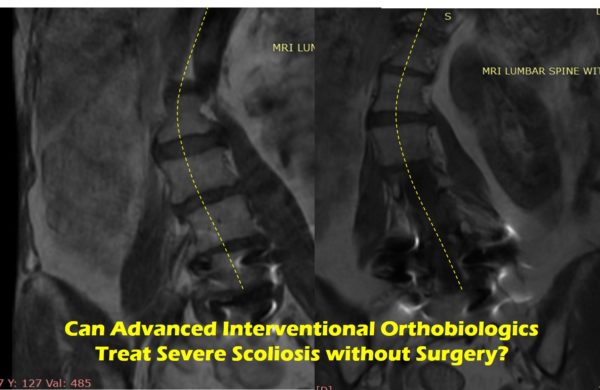
Freyda’s MRIs are above and they show a Cobb angle of more than 40 degrees, so she has severe degenerative scoliosis. She first saw me in 2017 and at that time she had just gotten L4 through her sacrum fused a year and a half earlier. Prior to that surgery, her Cobb angle was in the 30-degree range, but things got worse after the procedure. Her problems progressed to the point where she couldn’t walk long distances, sit in a restaurant without pillows, or do much in the way of any activity. Why? This is a problem called ASD which means adjacent segment disease. To learn more, see my video below:
I have treated Freyda several times with the Perc-Scolioplasty procedure using her own blood platelets in a few different forms (high dose platelet-rich plasma, platelet lysate, and platelet poor plasma). How did she do? As of yesterday, she says she’s planning a trip to Europe with her husband which wouldn’t have been possible before we began, Now she can walk about two miles, no longer takes pillows with her to go to restaurants, and finds that when things do get flared, they recover much more quickly. In essence, she avoided a long scoliosis type fusion.
The upshot? Why are we operating on so many scoliosis patients? There are excellent options for scoliosis treatment in adults like Schroth, bracing, and now Perc-Scoliolioplasty. Hence, there are many ways to avoid scoliosis surgery!
References:
- Bettany-Saltikov J, Turnbull D, Ng SY, Webb R. Management of Spinal Deformities and Evidence of Treatment Effectiveness. Open Orthop J. 2017;11:1521–1547. Published 2017 Dec 29. doi:10.2174/1874325001711011521
- Roaf R. “Historical Survey” in Spinal Deformities. 2nd ed. Pitman Medical; 1980. pp. 1–5.
- Willner S., Udén A. A prospective prevalence study of scoliosis in Southern Sweden. Acta Orthop. Scand. 1982;53(2):233–237. doi: 10.3109/17453678208992208.
- Rogala E.J., Drummond D.S., Gurr J. Scoliosis: incidence and natural history. A prospective epidemiological study. J. Bone Joint Surg. Am. 1978;60(2):173–176. doi: 10.2106/00004623-197860020-00005.
- Lonstein J.E., Carlson J.M. The prediction of curve progression in untreated idiopathic scoliosis during growth. J. Bone Joint Surg. Am. 1984;66(7):1061–1071. doi: 10.2106/00004623-198466070-00013.
- Branthwaite M.A. Cardiorespiratory consequences of unfused idiopathic scoliosis. Br. J. Dis. Chest. 1986;80(4):360–369. doi: 10.1016/0007-0971(86)90089-6.
- Weinstein S.L., Dolan L.A., Spratt K.F., Peterson K.K., Spoonamore M.J., Ponseti I.V. Health and function of patients with untreated idiopathic scoliosis: A 50-year natural history study. JAMA. 2003;289(5):559–567. doi: 10.1001/jama.289.5.559.
- Hong J.Y., Suh S.W., Modi H.N., Hur C.Y., Song H.R., Park J.H. The prevalence and radiological findings in 1347 elderly patients with scoliosis. J. Bone Joint Surg. Br. 2010;92(7):980–983. doi: 10.1302/0301-620X.92B7.23331.
- Lehnert-Schroth C. The Schroth scoliosis three-dimensional treatment; A physiotherapy method for scoliosis, Scheuermann’s, kyphosis and other related deformities of the spine. Maynard press. 1st ed. Part A; 2007. pp. 9–25.
- Schreiber S., Parent E.C., Khodayari Moez E., Hedden D.M., Hill D.L., Moreau M., Lou E., Watkins E.M., Southon S.C. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis – an assessor and statistician blinded randomized controlled trial. PLoS One. 2016;11(12):e0168746. doi: 10.1371/journal.pone.0168746.
- Andersen M.O., Christensen S.B., Thomsen K. Outcome at 10 years after treatment for adolescent idiopathic scoliosis. Spine. 2006;31(3):350–354. doi: 10.1097/01.brs.0000197649.29712.
- Danielsson A.J., Wiklund I., Pehrsson K., Nachemson A.L. Health-related quality of life in patients with adolescent idiopathic scoliosis: A matched follow-up at least 20 years after treatment with brace or surgery. Eur. Spine J. 2001;10(4):278–288. doi: 10.1007/s005860100309.
- Ward W.T., Friel N.A., Kenkre T.S., Brooks M.M., Londino J.A., Roach J.W. SRS-22r Scores in non-operated adolescent idiopathic scoliosis patients with curves greater than forty degrees. Spine. 2016. https://www.ncbi.nlm.nih.gov/pubmed/28796720
- Weiss HR, Goodall D. Rate of complications in scoliosis surgery – a systematic review of the Pub Med literature. Scoliosis. 2008;3:9. Published 2008 Aug 5. doi:10.1186/1748-7161-3-9
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi:10.1001/jama.2017.5283

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.