This Is a VERY Important Mesenchymal Stem Cell Study
How do mesenchymal stem cells work? We know some things, but not close to everything. In particular, how do they suppress bad inflammation? Turns out these cells have a big trick up their sleeve that few saw coming. Let’s dig in.
Mesenchymal Stem Cells
At Regenexx, we began using MSCs to heal and help manage orthopedic injuries way back in 2005. Mesenchymal stem cells (MSC), are a type of stem cell derived from bone marrow, fat, and other tissues. We’ve used them because of their ability to self-renew, repair, heal, and transform into other cells. Though their role in controlling inflammation is clear, how that works is less clear.
Someone Else’s MSC
Using someone else’s MSCs has a built-in problem. Why? On the one hand, we know that they are immunoevasive, which means that they can evade the host’s immune system and become invisible to the main immune response. On the other, eventually, they get taken out by the killer T response from the host’s immune system. This is different than your own MSCs which stick around.
So if someone else’s MSCs implanted into your body get taken out, do they only suppress inflammation for a short time? If they work longer, beyond the time they get destroyed by the immune system, how does that work?
New Research
A November 2020 study published in Stem Cells looked at mesenchymal stem cells and how they’re able to continue to suppress the inflammatory response even after the body has cleared them all out (1). The researchers injected human umbilical cord tissue-derived MSCs (hCT-MSCs) into mice with induced lung inflammation, but within 24 hours, all the MSCs had been removed by monocytes and macrophages (the foreign cell clean-up system).
It’s worth taking a minute to go over how macrophages and the cellular clean up system works. These cells get rid of foreign cells literally by eating them. They then “digest” them and spit out pieces that show up on their surfaces which are then “read” by other cells.
However, in a strange twist, the researchers also noticed that the cells that had engulfed and eliminated the MSCs underwent reprogramming by the MSCs. These clean-up cells could now suppress inflammation like the MSCs. How did that work?
The MSCs contained cytoplasmic processing bodies (p-bodies). These p-bodies contained RNA that was capable of creating proteins that suppress the activation of helper T cells.
P-Bodies
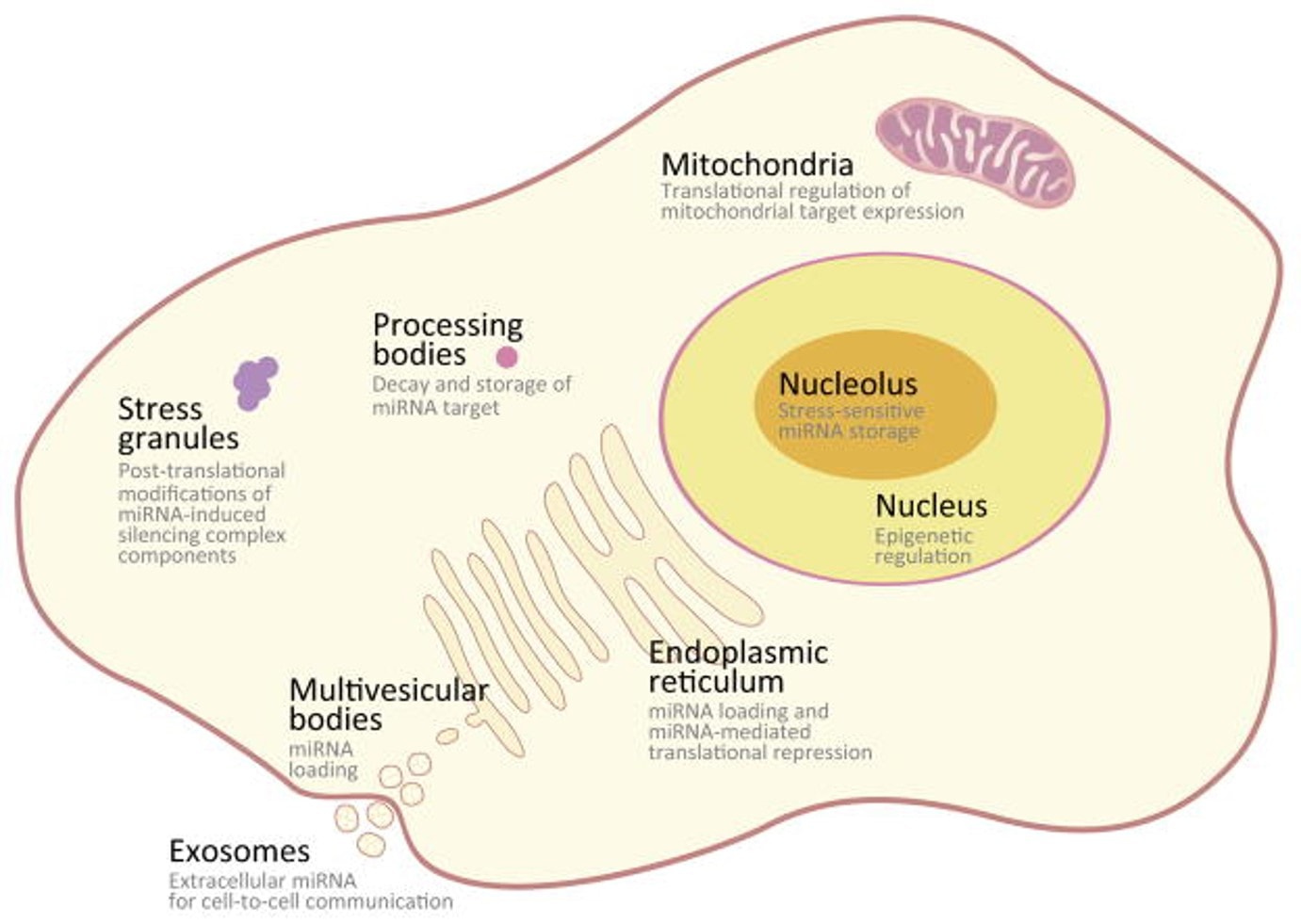
What interesting here is that while it’s known that these P-bodies may be important in regulating cells, they’re also thought to represent the decay products of RNA. While they were first described in 1997, so far, nothing monumental like this has been associated with them. Hence, my sense is that going forward, accessing whether stem cells have P-bodies that can suppress inflammation in this way may become a key assay in determining their potency.
The Ways We Know MSCs Work
So we know that MSCs work through differentiating or turning into other cells. We also know that they work by secreting lots of things including specialized chemicals and exosomes that can orchestrate how other cells work. In addition, we know that they can give their good batteries (mitochondria) to dying cells. Now they can also directly reprogram cells that eat them!
The upshot? This is a pretty cool discovery. The fact that MSCs were being taken out by the host’s immune system was a problem, but if they can reprogram other cells by getting themselves eaten as part of the immune response against them, that’s a page out of the Night of the Living Dead!
___________________________________
References
- Min H, Xu L, Parrott R, Overall CC, Lillich M, Rabjohns EM, Rampersad RR, Tarrant TK, Meadows N, Fernandez-Castaneda A, Gaultier A, Kurtzberg J, Filiano AJ. Mesenchymal stromal cells reprogram monocytes and macrophages with processing bodies. Stem Cells. 2020 Nov 9. doi: 10.1002/stem.3292. Epub ahead of print. PMID: 33166420.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.