A Research Update on PRP to Treat Knee Arthritis
It’s been more than a year since I published my infographic on the use of platelet-rich plasma for knee arthritis. Since that time, the pace of PRP research on knee arthritis treatment has quickened. Hence, today, let’s go over what we know now.
What is PRP?
PRP is when the doctor takes blood from the patient and concentrates the platelets in a centrifuge. The product that’s created is called platelet-rich plasma (PRP). All of those platelets release growth factors and other things like exosomes that can help healing. To learn more about PRP (as well as platelet lysate), see my video below:
What is an RCT?
RCT stands for Randomized Controlled Trial. This is the “gold standard” for quality research. Basically, patients are randomized to either receive treatment A or B, and then their response is measured. You can make the RCT better by making it placebo-controlled. That means that A is the treatment you want to evaluate and B is a fake treatment.
The Research on PRP Used to Treat Knee Arthritis
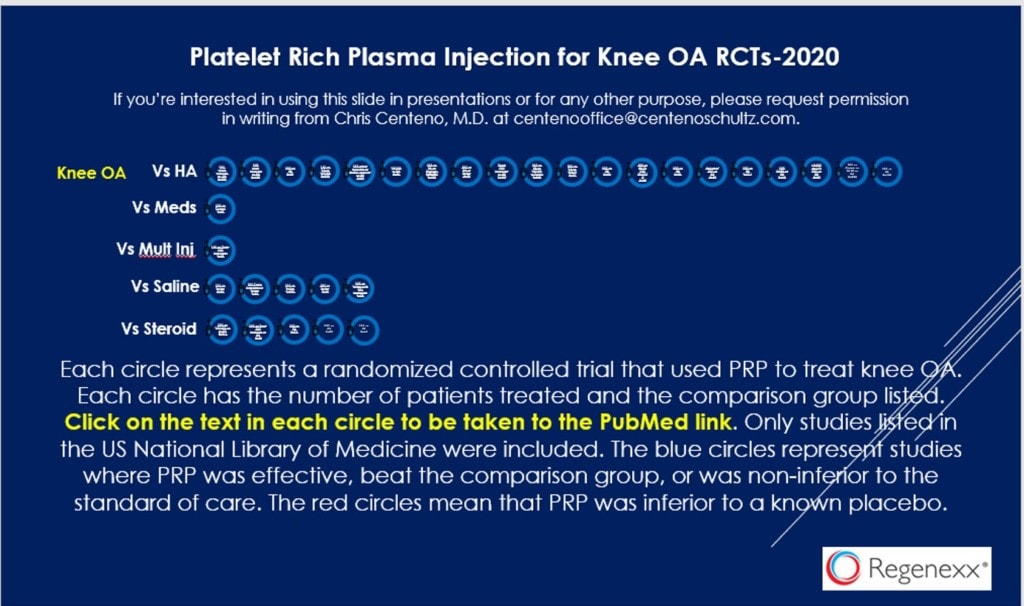
In the infographic above, you see 30 circles. Each describes something about a PRP RCT. Each has a hyperlink to the US National Library of Medicine where that study can be found. The PDF can be found by clicking on the image above or here.
We now have 30 randomized controlled trials on the use of platelet-rich plasma to treat knee arthritis. That’s pretty amazing since most of these are of higher quality than the single RCT that we currently have on knee replacement. Let’s dive into all of that for a few minutes.
We have 20 RCTs that compare PRP to common knee gel shots (Hyaluronic Acid or HA). In most of these studies, the PRP was better than the HA and in the minority, it was just as good. Bizarrely, HA is covered by most major insurance companies and PRP is not.
We have five RCTs where PRP is compared to saline control and in all 5, PRP beats saline. There are three RCTs where PRP is compared to the very common knee steroid injection, and in all three PRP beats steroid. Steroid injections for knee arthritis are covered by every major insurance carrier, PRP is not.
Now let’s get back to knee replacement. We have only a single RCT on knee replacement whose results were poor in my opinion. In addition, that study didn’t compare knee replacement to placebo surgery. Instead, it compared it to physical therapy. Hence, this study was of lower quality than many of those PRP studies above with a higher risk of a false result due to the tremendous placebo effect of big surgeries. To learn more about that study, see my video below:
How about other orthopedic surgeries to treat knees?. Do any of them from ACL reconstruction to meniscectomy to cartilage repair have 30 RCTs supporting their use? Nope? Do any of them have 5 RCTs comparing the surgery against a placebo surgery and showing efficacy? Nope.
The PRP Pushback
While the research supporting PRP use is far better than that supporting most of the common orthopedic surgeries in existence today, that hasn’t stopped certain groups from not liking this disruptive treatment. This largely takes the form of flack from some orthopedic surgeons and some bench scientists.
The Orthopedic Response
For some orthopedic surgeons, PRP has been adopted into their practices. This movement is gaining steam as the obvious high-quality research continues to be published. For others, PRP is a problem. Why? Let’s explore this a bit.
PRP is a problem for some orthopedic surgeons because it disrupts the status quo. For example, if you’re a joint replacement surgeon, PRP may have a real immediate impact on delaying those surgeries. If you’re focused on the health of your patients, that’s great news. If however, you’re focused on device payments to you from knee replacement device manufacturers, surgery center schedules being filled, or other financial, non-patient care concerns, PRP can mess with your bottom line.
The Bench Scientist Response
Just like PRP disrupts the orthopedic surgery status quo, it also disrupts the economics of university discoveries and patients in the world of stem cell drugs to treat orthopedic conditions. How? Let’s dive in.
Some in the bench scientist crowd have been actively campaigning against PRP. These are university professors who focus on the financial health of the commercial stem cell therapy drug market. Why would they care about a lowly blood product that could help knee arthritis patients avoid the need for surgery? Economics 101. Let me explain.
The bench scientist crowd who are financially conflicted all want to push expensive cellular drugs as treatments for common musculoskeletal problems like knee arthritis. These cell drugs, because they require FDA approval and extensive clinical trials, will all be very, very expensive. If PRP has become popular and covered by insurance as a cheap knee arthritis therapy by the time these cell drugs hit the market, there will be no market. Meaning, if their products can’t significantly beat PRP for efficacy, then the major health insurers won’t extend coverage for the more expensive cell drugs and the investments of universities who developed these cell drugs will be ruined. It’s simply that simple.
The upshot? PRP is here to stay. We have more RCTs supporting its use for knee arthritis than we have for most FDA approved drugs. There’s also substantially more research supporting its use than for any orthopedic surgical procedure in existence that’s used to treat knees. This makes PRP a major healthcare disruptor. For physicians focused on trying to find the best available treatment for their patients, this is all fantastic news. For some surgeons who want to maximize their income from joint replacement surgeries, this is not good news. Also, if you’re developing a competitive cell drug, you may not like all of the PRP research, as it could mess with your investment.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.