Learning About the Stages of Healing: The Curious Case of My Wife’s Fracture and PRP
Months ago, my wife tripped over our dog and fractured her fibula. After 6 weeks in a cast, she had only a partially healed bone and continued epic swelling in the leg. Hence I decided to inject PRP and all of the swelling in the leg vanished within 12 hours. What can that teach us about PRP and your healing?
A Fibular Fracture
As a couple, my wife and I are caring for her disabled mother at home and her mostly blind and deaf cattle dog named Annie. It’s probably tough being a dog that was bred to herd cattle and only have your sense of smell, and she frequently gets underfoot. A few months ago, my wife suddenly got up from her computer desk and Annie got caught underfoot. My wife fell to avoid crunching this little dog and heard a snap and had severe pain. The next day this was identified as a distal fibular fracture.
Problems?
The good news was that the fracture wasn’t displaced. The bad news was that the mid-level in the ER put on a temporary splint that was far too tight. She then went to one orthopedic surgeon who wanted to operate and place a plate. She never went back. She then went to someone I picked who was more honest with her. She could either go into a cast for 6 weeks and then into a boot or she could get a plate and maybe return to activity a few weeks faster. Given that she’s not much for surgery, she chose the cast.
When she came out of the cast at 6 weeks, the x-ray showed partial healing of the fracture and she was told to take it easy, but she could walk as tolerated, but then needed to rest and elevate. However, I was alarmed at how swollen the leg and ankle still were (50% bigger than the other side). She was also told that she would be back to full activity at 8 weeks.
We went to California for spring break and all during that trip the swelling in the leg was still epic. My initial thought was that her distal leg and ankle swelling would resolve with a little walking. If anything, that made it worse. In addition, I could tell that she was getting discomfort. She never told me it was pain, but rather a vague pressure.
The Bright Shiny Object Syndrome
I’ve talked about this issue many times. Basically, in situations of trauma where fractures are involved, the medical care system focuses all of its attention on the fracture and ignores the rest of the injuries. Knowing that it’s tough to break your fibula bone without lots of collateral damage to the main ankle joint and surrounding ligaments, at 7 weeks, when she was still limping around with severe leg and ankle swelling, it was time to dig deeper. My first concern was a DVT or blood clot in the leg. When the ultrasound came back negative and she was still the same, at 8 weeks I got an MRI.
The ankle MRI did still show a partially healed fracture and trashed inside and outside ankle ligaments. It also showed a cartilage lesion in the main ankle joint and severe swelling in that joint. Basically, the fracture was the least of her worries and our medical care system had totally missed far bigger long-term issues.
A PRP Miracle?
At that point, she went back to see the orthopedic surgeon and he wanted her back in a walking boot for two weeks. If the symptoms, swelling, and fracture didn’t improve in two weeks, he wanted to operate by adding the plate and performing arthroscopy on her ankle. That would in all likelihood include ligament procedures where they removed her damaged ligaments and drilled holes and strung tendons (Brostrom procedure).
That plan wasn’t going to work for my wife, or me. Hence, she came into the office last Friday and her ankle joint swelling was drained and high dose PRP was injected. Her damaged ankle ligaments and her fracture line and surrounding soft tissues were also injected.
What was amazing was that this severe swelling that had dogged her for months was gone by the next morning. Like a balloon where the air had been let out, her leg and ankle were now skinny and looked like they had been in a cast, atrophied calf and all. How could this have happened so quickly?
Superficial Thrombophlebitis
When we were ruling out a blood clot, the diagnosis that came back from radiology was superficial thrombophlebitis (ST) without an observed blood clot. Basically, that the veins were inflamed. I thought this was a complication of the cast. Is there anything published on PRP and ST? Nope.
What happened? My best, educated guess is that there was chronic inflammation in the leg because of the non-healed fracture. This was probably a neurologic/inflammatory response. Basically, her body was trying to heal the area, but being unable to get the job done, the inflammation just continued. The PRP caused both an acute inflammatory response and kicked her chronic bad inflammation into 2nd gear, moving it towards the resolution phase. Let me explain.
Understanding the Stages of Healing
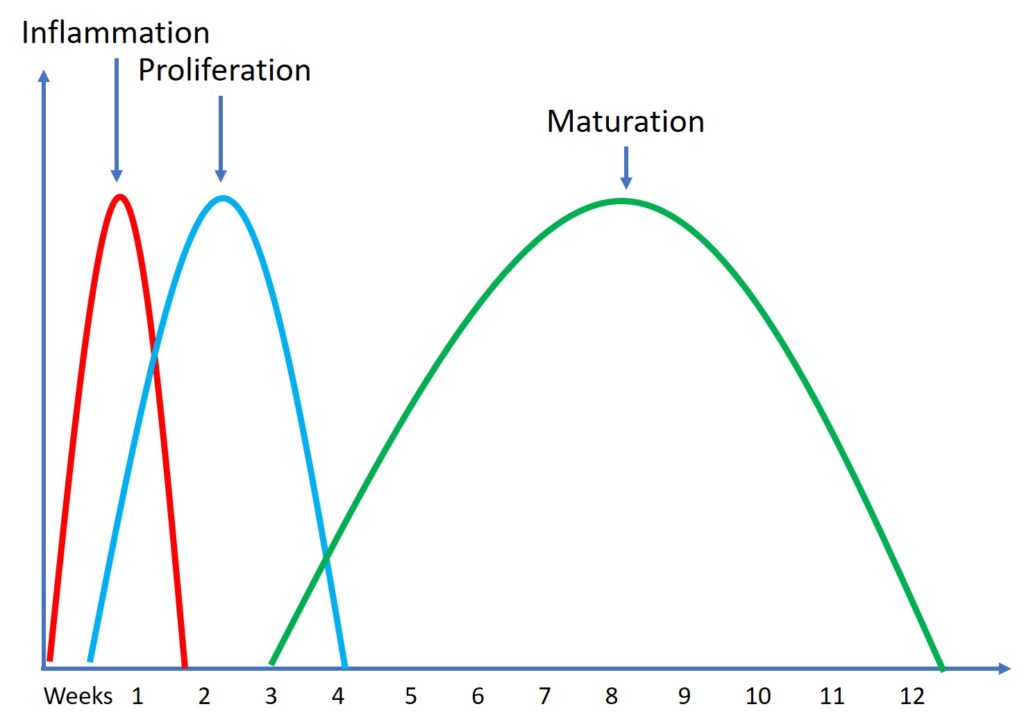
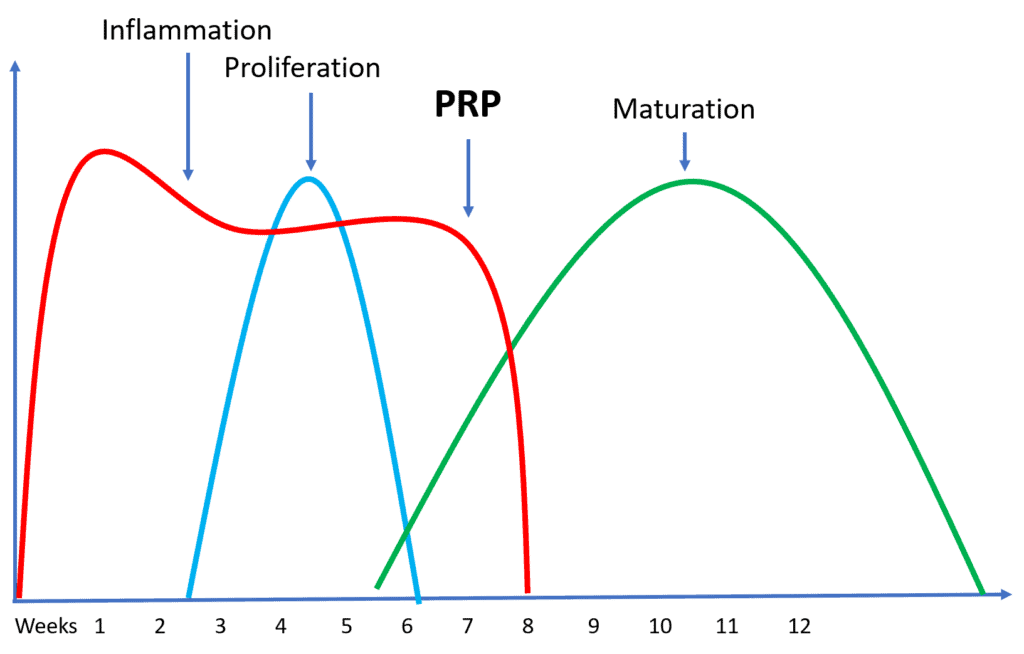
Normally, tissue healing happens in the above stages:
- There’s inflammation for a few days. This is the swelling we observe. This is when the body brings in cells to clear the damaged tissue and begin the healing process.
- Then, about day 3, the local repair cells begin to proliferate. For a fracture, this would be osteoblasts in the bone and local mesenchymal stem cells. This lasts through the first month.
- Finally, this new tissue that gets laid down in the proliferation phase has to mature. This is where the body tells the tissue the demands and loads it must carry and then remodels it to be able to tolerate those forces. This lasts through the first few months. In older people, this can even take longer than 3 months.
So what happened to my wife?
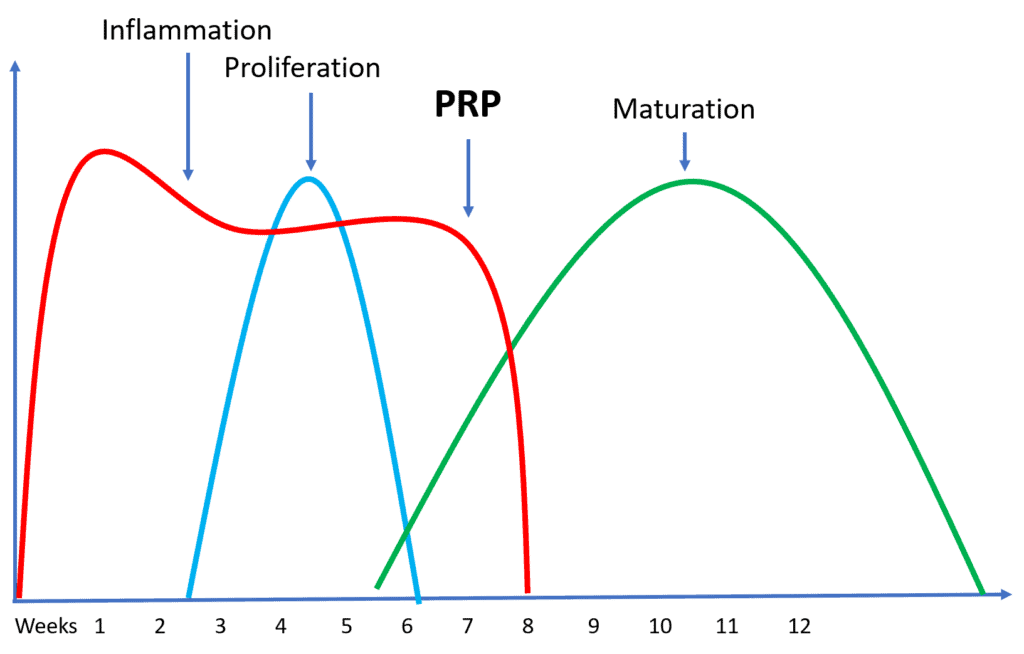
Her body got stuck in the inflammation phase, which delayed her healing. This is a form of the chronic inflammation that we all have been told is bad, although it was only in her leg. The PRP ended that phase and allowed her fracture and other areas to kick into the next phase of healing.
A Case for a Different Treatment Algorithm?
The case with the usual fracture is that it’s casted or plated and then immobilized to heal. The patient then is sent to physical therapy if they have residual problems. While this usually works well, what happens in cases where there is damage to the joint or surrounding ligaments? Or when the body is stuck in that chronic inflammation phase?
The problem is that it takes 3-6 months (longer in socialized healthcare systems) to get to the point where an MRI is taken and the problems are recognized. By that time, the damage has been done. Joints are fried and ligaments are further damaged. Big surgeries are required and significant and lifelong disability ensues. Thankfully all of this was caught early in my wife’s case, but my practice is filled with patients who fell into this hole in our care system and now need orthobiologics for big problems that could have been small issues if caught early.
The upshot? I will update you as we find out more at the end of this week when another x-ray and ultrasound will be taken. In the meantime, she is grateful that she can now walk with a boot and doesn’t have all of that inflammation and pressure pain. I am still amazed that PRP could so dramatically and quickly alter her course of care.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.