My Story of Living With Cervical Spinal Stenosis
On this page:
- What is cervical spinal stenosis?
- My story of living with cervical spinal stenosis
- Neck fusion vs. living with cervical spinal stenosis
- Diagnosing the symptoms of cervical spinal stenosis
- My tips for living with cervical spinal stenosis
I still remember the first day I knew there was something seriously wrong with my neck. I had just finished working out with a personal trainer when I wrenched something and went to lay down on the couch and couldn’t move my neck. In fact, the only way I could get up from the couch was to hold my teeth with one hand to support the weight of my head while using the other to push up.
Thankfully, this was gone by the morning, but it began an odyssey that ended with a diagnosis of cervical stenosis made via MRI and a recognition that I would have to adapt around this problem. Thankfully I knew what to do to manage the problem, and my life today living with neck stenosis, outside of a few adaptions, doesn’t look all that different from the life of most 50-somethings without stenosis.
However, having just gotten off the phone with a patient who is now where I was at my low point, I understand that most patients with this problem are trapped between a rock and hard place and have no idea how to climb out of that deep and dark hole. Hence, this unusually long blog.
What Is Cervical Spinal Stenosis?
Cervical stenosis means that the hole in the middle of the spinal cord (central canal) is too tight and doesn’t have enough room. Since this is the place that all of the wiring must pass through from your brain to your muscles or from your fingers and toes to your brain, pressure on the spinal cord here can cause all sorts of havoc. What causes the central canal in the neck to get too small? Neck-joint (facet) arthritis, disc bulges, loose ligaments, and being born with a small canal.
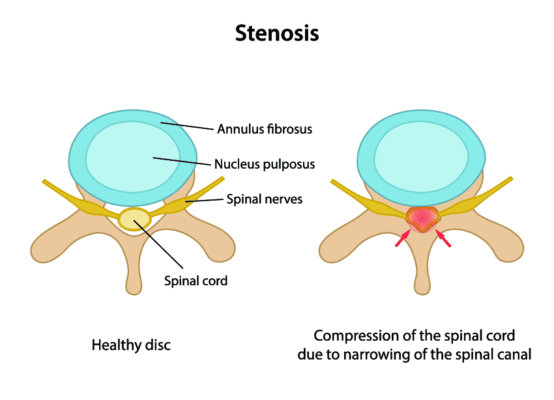
Photo credit: Shutterstock
My Story of Living With Cervical Spinal Stenosis
That day on the couch, I knew something was really wrong. I didn’t just have a stiff neck; I couldn’t move my head and neck! I wasn’t paralyzed anywhere else except my neck muscles. I should have gotten an MRI then as this was really messed up, but I didn’t, perhaps afraid of what I would find and because I was just too busy. My neck finally gave out a few years later, but not after any specific event—it just came out of the blue.
Before this major event, I had long noticed times where I had pain in my shoulder blade. I would ignore these and they would go away, but then about 3–4 years ago, that pain began to amp up. In fact, I remember pressure on my shoulder blade that felt like an invisible hand was shoving my head forward. I also remember that a few weeks before that, my thumb would go numb when playing football with my son.
That shoulder blade pain continued to rise until it became a 9/10. Given that I didn’t have much neck pain, I told the physicians at our clinic to inject my shoulder, which did nothing. Hence, I quickly became a connoisseur of carefully arranged sleeping pillows.
In fact, I could only sleep at a 45-degree angle, which meant broken rest at best. I then changed up the treatment plan and had my partner inject my neck with an epidural (around the nerves) using my own platelet growth factors (platelet lysate). For the first time in about a week, I went home without much shoulder blade pain! We had found the source, which was in my neck.
I also still remember staring at my MRI, disbelieving that it looked as awful as some of my patients’ MRIs! There were multiple areas where the spinal cord had barely enough room and a few where the exiting nerves had no room.
We had a friend of ours diagnosed at the same time with a similar condition who went for immediate surgery. I didn’t go that route; instead, I worked with our doctors to perform several injections. I also began to make changes to what I did and worked on getting my neck “opened up” by performing physical therapy at home. How all of that worked is below.
Neck Fusion vs. Living With Cervical Spinal Stenosis
We live in a society where we are erroneously taught that every problem we have can be “fixed’ with a surgery. As a physician who gets to see the strings in the surgical puppet show, I know that this isn’t remotely true. In fact, the most common surgery to “fix” cervical stenosis, a neck fusion, is often worse than the disease in my experience (1).
Basically, you solve one problem and introduce two others. In addition, a January 2015 study echoed that observation, showing that while stenosis patients do better for a time after surgery, by 3 to 4 years out, they’re right back where they started, but now with all new issues (2).
One of the things patients need to get over is the “hard sell” that surgeons will use to try and convince the patient to undergo surgery. Usually, scare tactics like, “If you take a bad fall or get in a car accident, you’ll be paralyzed.” Is this true?
While it’s theoretically possible and is seen from time to time in large university medical centers, it’s so rare that it’s hard to find any statistics on (believe me I’ve tried). Hence, near as I can tell, the likelihood of this happening is about the same as dying in a fatal car crash. It can happen, but it’s a very rare event.
Diagnosing the Symptoms of Cervical Spinal Stenosis
As I spoke to a patient the other day about whether we could help his stenosis, I realized that one of his problems is that nobody had ever told him that living with neck stenosis was possible, and that you could not just live, but live well.
I thought back to what my life would have been like had I not learned how to make minor adaptions and if I didn’t have the advanced injection care of my colleagues, placing platelet growth factor shots in all the right places. I would have had a surgical fusion by now, and we would be chasing the new pains caused by the surgery, or I would be like my patient on the phone, disabled and unable to do much.
Before I can go into how to live and function with cervical stenosis, you have to understand a few rules of the road. First, you need to understand how to recognize symptoms of what I call “ramp up.” This means that the nerves in your neck are getting irritated and it’s time to back off. What does this look like for a patient with stenosis? Here’s what happens to me:
- Tightness or soreness in the muscles of my forearm or arm. Most people and many physicians don’t understand that irritated neck nerves can cause tightness in the upper back, shoulder, biceps, triceps, forearm, or hand. At times this will feel like pressure, and other times this will feel like the muscle is sore for no reason. Sometimes it will show up as a small cramp.
- Numbness or tingling can happen, but for me it’s not as prevalent, other than at night. When that occurs during the day, it’s usually in my thumb, and it means I’ve really pissed off my neck. At night, either one of my whole hands can go numb. This happens if I have my head in the wrong position or if my shoulder is too far forward, placing pressure on the brachial plexus nerves.
- Neck tightness and decreased range of motion are common. This tends to happen when I overdo it, usually with lifting weights. This happens because the nerves that supply the small stabilizer muscles close to the spine get irritated because I have brought too much of my neck into the lift (rather than just my torso and arms). Hence, the small stabilizers get knocked offline and the big muscles like my upper traps, levator scap, and scalenes take over to stabilize my neck, causing tightness. This is because these muscles aren’t designed to be neck stabilizers.
- Crepitus is a medical term that means popping and cracking in a joint with motion. This can happen to my neck when the stabilizer muscles are offline (see above).
- Low-back pain? While I have a separate low-back issue, when I sleep with my neck in the wrong position, I can wake up with back pain. Why? The nerves in my spinal cord that go to that area can get irritated.
- Fasciculations, or muscle jumping, is common. This just means that the nerve supply to that muscle is offline.
- Weak or heavy legs or arms is not uncommon. This comes from irritated nerves that supply these muscles. If it happens in my shoulders, I take this as a serious sign that I need to get the nerves calmed down.
My Tips for Living With Cervical Spinal Stenosis
- You may have heard the phrase “location, location, location” for buying real estate. The analogous phrase for cervical stenosis is “head position, head position, head position.” Meaning that when your head and neck get bent in funny ways, this puts pressure on the nerves and spinal cord. As an example, I limit or, at least, control the amount of time I spend looking down at my phone or anything else. Or another example, lying in bed with my head propped up to read a book or an iPad will begin to set things off. The workarounds? Hold your phone higher to keep your head and neck straighter and lie on your side with your head correctly positioned to read a book.
- Sleeping can be interesting and a time when your head and neck can get in weird positions and begin a cycle of being “ramped up.” When my neck was really bad, I would sleep with a loose cervical collar at night. In fact, I became a connoisseur of cervical collars, looking for just the right one with the right fit or making small modifications to them by cutting out this piece of plastic or that. I also experimented with how loose or tight they should be. When I was deep in the hole, this really helped me climb out. While I no longer use these, I always make sure one is handy if my neck gets really aggravated.
- Pillows are a big deal. I need to use a specific one to keep my head in straight alignment with my body. If the pillow is too big (e.g., in a hotel), I can wake up with symptoms that can take the better part of the day to go away. So making sure that you have a pillow that can compress is key. I also only sleep on my side and avoid sleeping on my stomach with my head turned. Sleeping on your back is fine.
- Weightlifting or just lifting and carrying heavy things. As you read above, this is what got me in trouble the first time my problem exploded. However, I’ve learned that all of this is fine as long as I can control my core. This means that I am intensely focused on lifting less weight for more reps, and for every arm workout, there’s either a core component (like benching less weight on a Swiss ball) or many exercises exclusively focused on my core (like slow and careful body rotations with a pulley). So the rule is that I can only lift heavier once my core gets stronger. How do I know I’m pushing it too hard? If my neck kicks in substantially during the exercise. I now know that this is not a good sign and I’ll pay for it. None of this means that I’m not able to stay in shape; it just means that I need to listen to what my body is telling me.
- Overhead work is a killer. When you have cervical stenosis, your neck stabilizers can easily go offline. When this happens, you become “trap dependent,” meaning your trapezius muscles are responsible for stabilizing your neck. When you do overhead work or have one arm up and resting on something, that takes the trap out of commission as a stabilizer, so you’re relying on neck stabilizers that don’t work so well. This can be a recipe for tweaking your neck.
- Bad seats are a hazard. The absolute worst is either an airline economy seat or some of the newer movie seats that have a forward head support and bend your neck slightly forward. Both can be helped by placing a rolled up jacket behind the curve in your low back, to create some natural curvature of the neck and to push your body forward of the headpiece. The same holds true for other chairs. In addition, turning your head frequently left and right can be an issue, so never position yourself at dinner in a seat where you need to have your head turned to talk to someone!
- Stretching is key. You can’t let yourself develop an old man or woman forward head! Or at least it’s your day job to fight against gravity. Why? A forward head puts more pressure on the spinal cord! Hence, I’m constantly using my “Old Man Stretch.”
- Stability is key. To this end, injections into the loose spine ligaments that come with stenosis to help tighten them and reduce sloppy motion is a key part of reducing symptoms and increasing function. Why? Sloppy spine motion means more nerves being banged into and more symptoms and less function.
- Putting the fire out when it happens is also key. Despite how carefully you move or position your head, there will be times when things get ramped up and out of control. For me, when that happens, I take an occasional Tylenol, which will help reset things, as it can be a potent nerve drug. If Tylenol won’t touch your symptoms, then you need to start where I started, having high-dose platelet growth factors injected around the neck nerves (epidural or into the facet joint using X-ray guidance). I still do this once or twice a year when I feel things getting ramped up and I can’t bring them back down by myself. My last injection was about a year ago. I stay away from steroid shots in my neck, as while these can help reduce swelling, they also inhibit healing, damage cartilage, often have diminishing effects, and have systemic side effects (3,4).
While I have other things I could teach, it’s critical to understand that living with neck stenosis is possible. My life is very active. On the weekends I hike about 2,000 vertical feet and eight miles. I lift weights twice a week. I do some sort of leg workout or cardio on other days. Meaning, nobody looking in at my life (outside of my wife) would know that I have this problem.
Are there types of stenosis you can’t live with and that require surgery? Yes, but at this time, we can manage about 70 to 80% of all patients that get this diagnosis and who are told that they need surgery. Hence, you have a good shot at avoiding the surgery bullet.
The upshot? A diagnosis of cervical stenosis in most cases doesn’t mean a fusion is automatically needed. Living with neck stenosis is possible and not hard to do, but you need to learn the tricks and how to manage the problem.
I’m several years into this and 98% of the patients in my shoes would have long since had a cervical fusion. My goal with this long blog this morning is to make sure that people with this problem know that surgery is not your only option and that you can live well with this disease!
—————————————————
References
(1) Maruenda JI, Barrios C, Garibo F, Maruenda B. Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J. 2016;25(5):1550-1557. doi:10.1007/s00586-016-4469-5
(2) Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63-76. doi:10.1097/BRS.0000000000000731
(3) Chon JY, Moon HS. Salivary cortisol concentration changes after epidural steroid injection. Pain Physician. 2012;15(6):461-466. https://pubmed.ncbi.nlm.nih.gov/23159961/
(4) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017;317(19):1967-1975. doi:10.1001/jama.2017.5283
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.