Can You Dodge ACL Surgery Arthritis? Brooke’s Story…
We’ve now officially saved many kids from ACL surgery. Why do I say “saved”? After all, isn’t ACL surgery a rite of passage for teenagers these days? They break the ligament and they get it replaced, just like inserting a new spare part? Nope. ACL surgery in a teenager is nasty business, a decision that will likely lead to arthritis by age 30. In fact, let’s coin the term now so that every parent out there can conceptualize ACL surgery appropriately; we’ll call this phenomenon “ACL surgery arthritis.”
What Is the ACL and Is Surgery in a Teen a Good Idea?
Most patients and parents believe that an ACL surgery is just a rite of passage for an athletic kid. The part breaks and you surgically insert a brand-new one, but regrettably this is fiction. Let me explain.
The canary in the ACL surgery coal mine began singing based on a study that was published a few years back that showed that 2/3rds of teens who get the surgery will have arthritis by age 30! Let that soak in for a moment. We’re putting kids through invasive surgery in hopes of avoiding later arthritis, and the majority are getting ACL surgery arthritis anyway? Why are we drilling holes in their bone and inserting a fake ligament? To make them feel like an NFL player trying to get a contract extension?
Why a Surgically Implanted ACL Will Never Be like the Original Equipment
There are a slew of differences between the tendon that’s fashioned into a ligament and drilled into the knee and the original ACL that was torn:
- The artificial ACL goes into the knee at a much steeper angle than the original ligament. This means that in order to have a similar function, it must be placed in very tight, adding compression forces to the cartilage that likely worsens wear and tear.
- The natural ACL has two bundles that help control excessive rotation of the tibia; 90% of surgically replaced ACLs have only one bundle, which leaves the knee rotationally unstable.
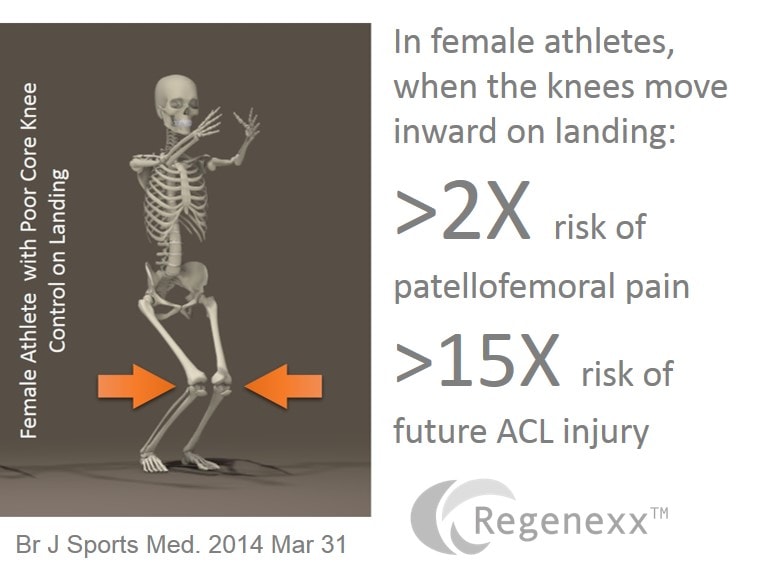
- The ACL reconstruction has no proprioception (position sense), leading to poor control of the knee on landing.
- The hamstring muscle from which the ACL graft is often harvested will be left permanently weaker than the other side.
Wouldn’t It Be a Better Idea to Heal and Keep Your Own ACL?
With all of the problems that come with ACL reconstruction, like ACL surgery arthritis, why not just try to heal the ligament in situ (i.e., in the knee)? This had been thought impossible until we began showing before and after MRI evidence after a highly precise stem cell injection using C-arm fluoroscopy to guide the placement of cells. This culminated in a research paper on using computerized imaging analysis of stem-cell-treated ACLs with before and after MRI images that was published in 2014. We’re now putting together a larger case series for publication and have an ongoing randomized controlled trial further scientifically vetting the technique.
Brooke’s ACL Journey…
Brooke is a 17-year-old high-school dancer who in November of last year heard a pop in her knee after an awkward landing and was diagnosed with a complete ACL tear. Note the image on the left (at the top of this post) and the yellow triangles. The ACL course is outlined, and the ligament is big, blown out, and ghost like in appearance—denoting a complete ACL tear. Brooke was a surgical candidate, but given that most kids who get surgery will end up with ACL surgery arthritis, there had to be another way. So Dr. Schultz at our Colorado clinic carefully and meticulously injected her own specially processed stem cells into both bundles of her blown out ACL using C-arm fluoroscopic guidance (i.e. no surgery). The four month after image is on the right, where the yellow triangles now define the course of a ligament that’s darker and more formed like a normal ACL than the blown-out ghost like appearance of the prior study. Based on these MRI images, Brooke’s ACL is on its way toward healing without surgery!
Can the Guy Down the Street Who Took a Weekend Course in Stem Cells Do This?
Regenexx is advanced interventional orthopedics, which is a separate and distinct medical specialty that takes years of training to master. The orthopedic surgeon, physical medicine, or family practice sports doctor down the street who took a weekend course and knows how to use ultrasound to perform a simple joint injection in the knee doesn’t have the advanced training to be able to get your stem cells anywhere near your ACL ligament.
The upshot? We’ve now saved many teens from invasive procedures and hopefully ACL surgery arthritis, simply by perfecting the precise placement of their own stem cells into their ACL ligament using our advanced Regenexx-SD procedure. I consider it a personal victory of how medicine advances from more-invasive to less-invasive procedures for every kid and adult who gets to keep their own ACL because of this groundbreaking procedure!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.