CCJ Instability: Rectus Capitis Posterior Minor and the Myodural Bridge
One of the more amazing things experienced during my medical career has been that smart physicians and scientists keep finding out brand new things about the body we didn’t know. One of those discoveries that have happened in the last 15 years is that a tiny muscle that lives at the base of the skull is actually connected to the covering of the brain and involved in headaches. So what is this muscle, and how might having loose ligaments holding your head on (CCJ instability) cause headaches by messing with the muscle? Let’s take a look.
What Is CCJ Instability?
Your head is held on by strong ligaments in the high upper neck. Regrettably, 99.9% of physicians when asked wouldn’t know the names of these ligaments, so it’s not surprising that when they get damaged or become loose, physician specialists scratch their heads as to what’s wrong. CCJ means “cranio-cervical,” and CCJ instability means that the ligaments that hold the head on are lax and the upper neck joints are moving around too much. To learn more about CCJ instability and what can be done for it short of surgery, watch my most recent video on the subject below:
Our Complex Upper Neck Muscles
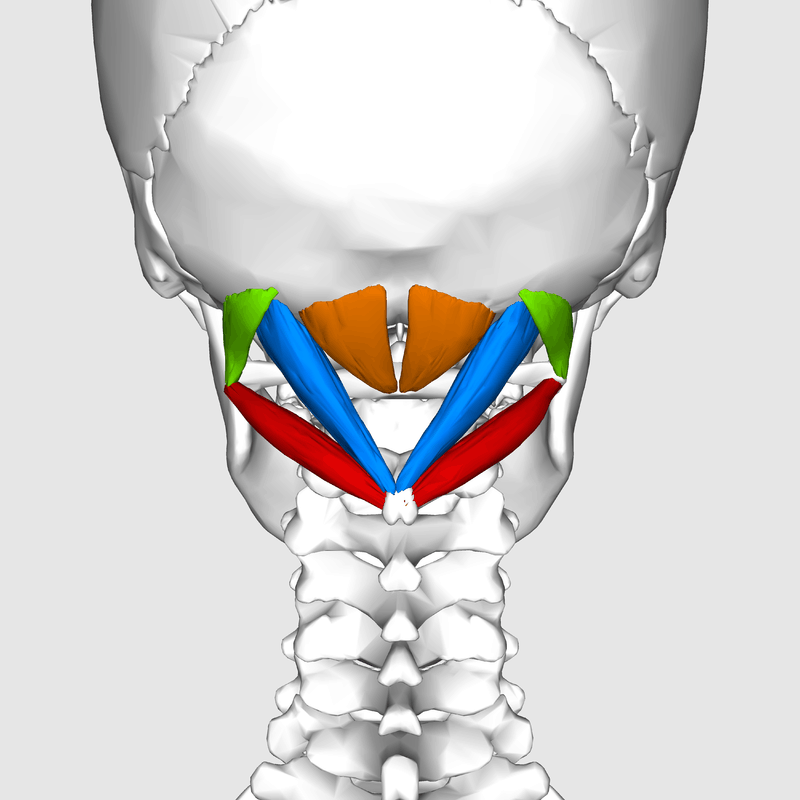
The upper neck muscles at the back of the head are very complex. Just take a look below:
It’s not hard to see how these muscles are designed to help move your head around the neck in lots of different directions. In fact, they can help you look up and down, bend your head to the right or left, turn your head, or any combination of those movements. In addition, they have many position sensors to give the brain information about where the head is located. For example, whether it’s 2 degrees side bent to the right and 5 degrees in flexion or 3 degrees of side bend. All of that data has to be coordinated with the information coming from your eyes and inner ear. What happens if it’s not? You get dizzy or off balance.
The Myodural Bridge
Back in the early 2000s, some smart neurosurgeons noted that when they cut through the midline of the back of the skull to access the brain, patients would note that their headaches went away. When they searched anatomy textbooks, they couldn’t explain why this would happen, so they did some cadaver dissections of their own. What they found shocked the medical world. Turns out that one of those tiny muscles in the upper neck called rectus capitus posterior minor was actually connected to the covering of the brain! Think about that for a second, and let it swirl around your noggin. A muscle used to position the head is connected to the brain? They published this finding in a medical journal, and it made big news.
Now that the neurosurgeons had found this new connection, which they called the myodural bridge (the dura is the covering of the brain), they had an explanation for what they saw with headaches and surgery. When they cut this muscle to access the brain, the constant tugging on the covering of the brain that had been causing headaches went away. This caused the headaches to vanish.
How CCJ Instability Might Impact All of These Small Muscles
If your head isn’t firmly affixed to your neck because the ligaments have been damaged, these small upper neck muscles must now go into overdrive to try to stabilize the head. The problem, of course, is that these muscles weren’t designed to stabilize the 10- to 15-pound bowling ball called your head. In addition, one of them is hooked into the covering of the brain, so when it goes into spasm because it’s had enough, the headaches kick in. In addition, it can be damaged through wear and tear, like any other muscle and tendon, and get inflamed and beat up, causing more problems for the myodural bridge.
Now, we could cut this muscle, but that only weakens the stabilization system just at a time when it’s needed the most. So that could be like throwing gasoline on a campfire. Meaning there are other structures in the upper neck that will then be fried by excessive motion that can also cause headaches (the nerves and facet joints). Hence, cutting this muscle tendon and the myodural bridge connection may solve one problem and cause others.
Injection the Rectus Capitis Posterior Minor Isn’t Easy
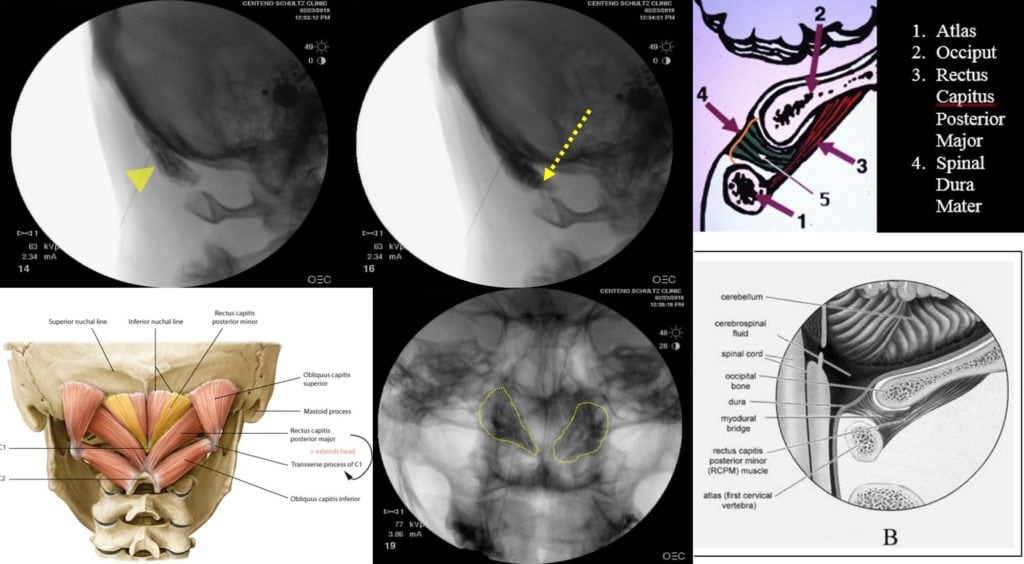
One of the things we can do to help this pain is obviously to treat the ligaments that hold the head on, as described in the above video. However, yet another is to inject the RCPM with platelet rich plasma just like we would do with any muscle and tendon that’s been beaten up by excessive wear and tear. The problem is that there are no textbooks that detail how this muscle is to be injected. While it can be injected using ultrasound imaging, the hair is often in the way and you don’t get a sense of whether the injection has also traveled into the myodural bridge. Injecting the muscle with radiographic contrast and using fluoroscopy can accomplish both things as this technology isn’t disrupted by hair the same way that ultrasound signals are, and the contrast can be easily seen connecting the muscle to the dura. Here’s an RCPM injection from yesterday:
The X-ray (fluoroscopy) images from the side of the skull view (two images up top) clearly show the muscle being injected, and the contrast even extends into the myodural bridge (yellow arrowhead points at the RCPM muscle and the dashed arrow points at the contrast in the myodural bridge). I’ve included a view of the injection through the skull that also shows the muscles (I have gotten more of the lateral portion of the muscle and tendon, which I have outlined in yellow on the muscle diagram in the lower left corner of this montage). The muscles are outlined by the dashed yellow line on the skull X-ray. The two images off on the right at the top and bottom are illustrations of how the muscle, the myodural bridge, and the dura interconnect. In the bottom illustration, #5 is the myodural bridge.
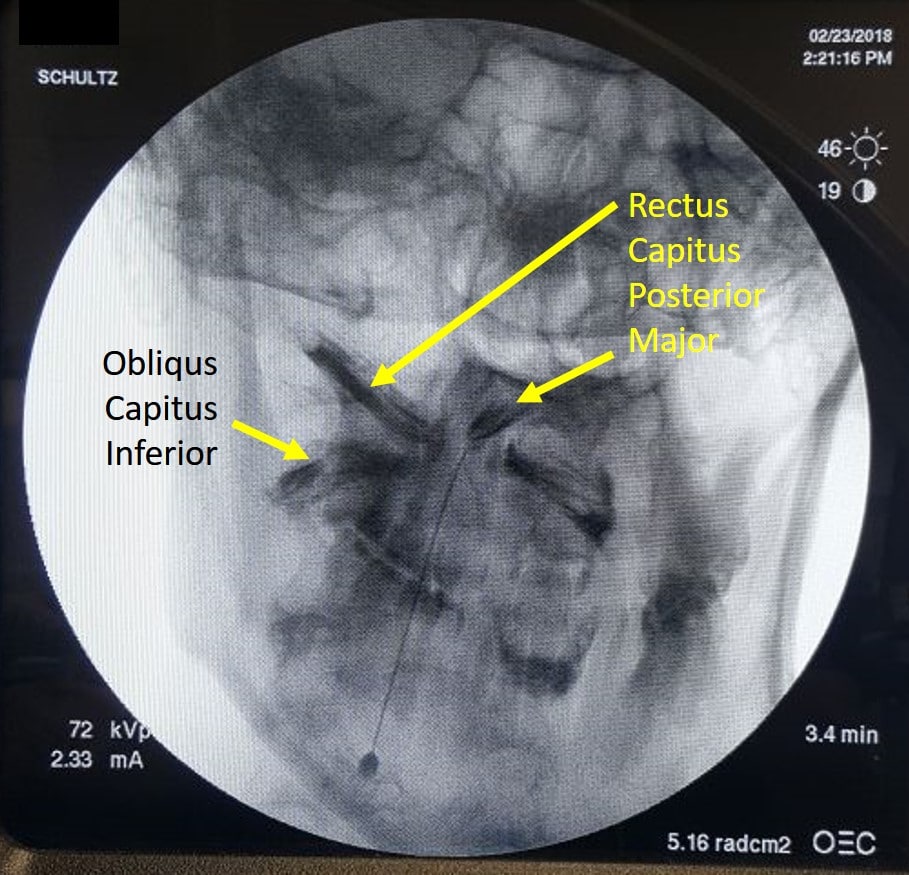
Can you inject the rest of these complex muscles? Yep, see an injection from Dr. Schultz, also from yesterday, outlining these muscles with contrast:
The upshot? We can treat these complex upper neck muscles. While there are no textbooks for how this should be done, we at Regenexx HQ in Colorado pride ourselves in writing the texts, not following them. For this patient above, we will treat her upper neck ligaments and CCJ instability, but in the meantime, if we can help her headaches by calming down the inflammation and tendinopathy in the RCPM muscles, that’s a net positive!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.