Could a New Hydrogel Help DDD?
Credit: Shutterstock
Degenerative disc disease or DDD is a common problem. While lots of therapies have been discussed, there is still no reliable way to grow people a new disc. A recent small study on an injectable hydrogel was recently hyped in the media as maybe solving this issue? Let’s review that new data.
What is DDD?
Credit: Shutterstock
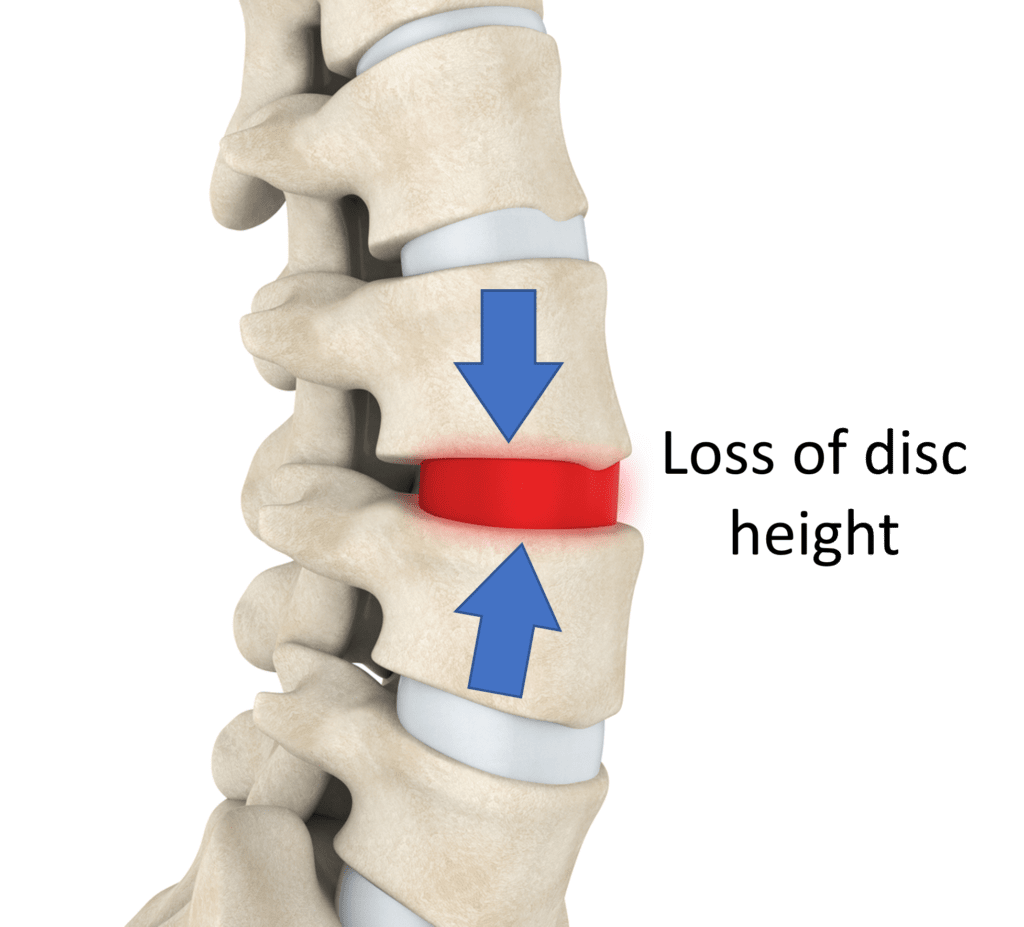
Degenerative disc disease is when the disc between the vertebrae loses its ability to hold onto water. It can then begin to dry out and lose height, which then puts more stress and weight on the facet joints, leading to arthritis in those joints. During this time, the whole functional spinal unit gets sloppy and begins to move around too much both due to ligament laxity and atrophied stabilizer muscles.
The disc maintains its height with living cells in the nuclear pulposis that produce the chemical that holds onto water. This chemical is called a GAG (glycosaminoglycan).
DDD Treatment Approaches
PRP or platelet-rich plasma has been shown to be able to treat DDD when the pain is caused by a tear in the disc (1). Bone marrow concentrate has also been used to help this kind of disc pain (2). We have published on the use of culture-expanded mesenchymal stem cells used to treat disc bulges (3,4). However, none of these technologies can regrow you a new disc.
An alternative approach to treat DDD that we’ve used for years and are now conducting a randomized placebo-controlled trial on is treating the facets, irritated spinal nerves, atrophied muscles, and lax ligaments with platelet-based products. In our clinical experience, this works well and avoids the potential complication of discitis by skipping the injection of the disc. Discitis is when the bacterial microbiome of the disc is upset and one bacteria (usually p acnes) overgrows. This can need IV antibiotic treatment and often a surgical clean-out. This happens in about 1 in 200 injected discs.
The most common way painful DDD is treated when the patient fails conservative care is ablative or surgical. One approach is to perform radiofrequency ablation of the nerves that transmit pain signals from the facet joints. The problem is that this kills the nerves that supply the stabilizing muscles and in our experience makes the patient worse in the long run. Alternatively, low back fusion surgery is used to lock the vertebrae in place using hardware. This is very invasive and can cause adjacent segment disease (ASD). That’s when the levels above and below begin to wear out due to the extra stresses.
Injectable Hydrogels 101
A hydrogel is a gel that holds onto water. The body’s original injectable self-assembling hydrogel is blood. You can inject it and through the magic of the clotting cascade, it will become a solid clot with the consistency of Jello. There are many others that have been floated in the world of animal and basic science research.
A self-assembling hydrogel is usually one that can be injected and through some intervention, it becomes the consistency of a blood clot or denser. This can happen with a change in temperature or something like adding UV light.
The New Research
A small study was recently published of 19 patients aged 22-69 years of age with DDD who had failed conservative care and who still had 0-10 pain scores of 4 or more (5). These patients had low back pain that had been confirmed as caused by the intervertebral disc. This means that the patient had a positive discogram where the doctor injected dye into the disc and this caused their usual pain.
The procedure involved injecting a product called Hydrafil which is a self-assembling gel that when heated is a liquid and at body temperature “sets up”. The procedure involves using a very large 17 gauge needle to place the gel into the disc. The patients were followed for 6 months and preliminary results showed a reduction in back pain 0-10 scores 7.1 to 2.0 (p < 0.001) and Oswestry Disability Index scores from 48 to 6 at 6 months.
The Good News
This is a small case series without any randomization that shows that injecting discs with an injectable hydrogel may help back pain in DDD patients with discography confirmed discogenic pain. The pain reductions were solid, but this is a tiny study with no long-term follow-up, so what the results look like in a bigger patient sample or for a longer time period is unknown.
Problems
We currently have higher-level RCT data on PRP when injected into discs in the same patient population. This can be injected via a much smaller 22 gauge needle that’s half the size of a 17 gauge needle. This is a big deal because placing a bigger hole in the disc to inject this stuff is not trivial. For example, we know that tears in discs can begin the degenerative cascade, so a bigger needle may cause a bigger long-term issue.
GAGs are produced by the cells in the nuclear pulposis. That system allows GAGs to be constantly produced and refreshed. So injecting a hydrogel will only allow a disc to hold onto water for some period of time. This is why I’m very curious as to why the MRI data wasn’t presented here. Also absent is an analysis of changes or improvements in disc height. The abstract states that the images were performed. The idea behind this treatment was that the injectable hydrogel could help the disc hold onto water long term, so the absence of that data is curious.
The upshot? While the new study is promising, it’s a small low-level case series and not a randomized controlled trial comparing this treatment to something else. We also have no MRI data and we know that other injectable orthobiologics in current use work well in this patient population. We’ll see how all of this develops.
_________________________________________________________
(1) Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R. 2016 Jan;8(1):1-10; quiz 10. doi: 10.1016/j.pmrj.2015.08.010. Epub 2015 Aug 24. PMID: 26314234.
(2) Pettine KA, Suzuki RK, Sand TT, Murphy MB. Autologous bone marrow concentrate intradiscal injection for the treatment of degenerative disc disease with three-year follow-up. Int Orthop. 2017 Oct;41(10):2097-2103. doi: 10.1007/s00264-017-3560-9. Epub 2017 Jul 26. PMID: 28748380.
(3) Centeno C, Markle J, Dodson E, Stemper I, Williams CJ, Hyzy M, Ichim T, Freeman M. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017 Sep 22;15(1):197. doi: 10.1186/s12967-017-1300-y. PMID: 28938891; PMCID: PMC5610473.
(4) Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016 Sep 1;14(1):253. doi: 10.1186/s12967-016-1015-5. PMID: 27585696; PMCID: PMC5009698.
(5) Abstract 45: Treatment of Painful Lumbar Degenerative Disc Disease: A Feasibility Study. D. Beall, K. Amirdelfan, P. Nunley, T. Phillips, I. Navarro, A. Spath. Annual Scientific Meeting, June 11–16, 2022. This abstract can be found at sirmeeting.org after the embargo time.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.