Is True Needle Arthroscopy on the Way?
We have been both excited and then disappointed by the state of the art in small arthroscopes. Now a new technology could one-day produce a true “needle scope”. Let’s dig in.
The Promise of Needle Arthroscopy vs. The Reality
I first heard the term “needle arthroscopy” about a decade ago. The idea, at least as I had envisioned it, would be that you were performing your normal guided injection of orthobiologics either using fluoroscopy or ultrasound and that you could additionally “see” through the end of the needle. However, what was actually possible and what was real didn’t jive.
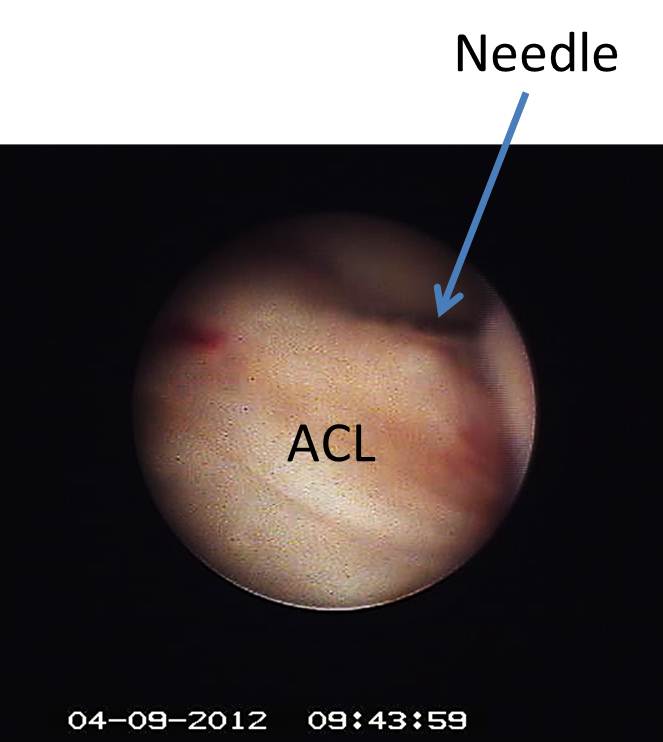
We tried our first small arthroscopes in 2011/12 and the problem was that they weren’t all that small, they were invasive to use, and they had poor imaging. First, the size was nothing close to the 22 or 25 gauge needles we commonly used. In fact, the systems were often 4-5 times as big. In addition, because of their size and lack of flexibility, they were difficult to use and much more likely to damage tissue than a guided injection. Finally, the imaging was poor. It was grainy and had a very limited field of view (meaning that you could only see what was right in front of you). To the left is the first injection we did using the small arthroscope into a damaged ACL in 2012.
Better Small Scopes?
In the past decade or so, the good news is that the scopes have gotten a bit smaller and the resolution has gotten better. However, we’re still not anywhere near the reality of needle arthroscopy. Let’s take a specific example, our Perc-ACLR procedure.
The Perc-ACLR procedure was originated by the Colorado HQ site of Regenexx back in 2011. We were the first physicians on earth to reliably use bone marrow concentrate (which is rich in stem cells) to inject a damaged ACL using imaging guidance. Since then we’ve published several studies demonstrating that healing the ACL is possible and that these patients generally avoid surgery and return to sports much more quickly than a surgical ACL reconstruction (1,2). In addition, we have an almost completed RCT study. To see what the procedure looks like, see my video below:
The Perc-ACLR is performed with a 25 gauge needle using real-time x-ray guidance (fluoroscopy). We’ve tried this using ultrasound, but the problem is that you can only see the part of the damaged ACL in the front of the knee and you also can’t get a handle on where the bone marrow is going. For comparison, one of the systems on the market, called the MyEye is more than 4 times as large in diameter as my 25 gauge needle. More diameter and stiffness means more potential for damaging tissues while taking a look. Hence, we have a unit and we don’t use it.
A True Needle Arthroscope?
Engineers from Johns Hopkins have defied the give-and-take principles of the optics to invent a lens-free endoscope (or arthroscope) only a few human hairs in width—more ultra-miniaturized than ever—that produces higher quality images than its bulkier predecessors.
Endoscopes or arthroscopes traditionally range from roughly a half-millimeter to a few millimeters in diameter, with smaller endoscopes being less destructive to tissue—but creating weaker images than larger endoscopes that risk damaging the tissue. But the new scope seems to have overcome the balance paradigm between size and resolution by going lens-free without the use of fiber optics. (Fiber optics, until now, were the only mechanism for lensless microendoscopy, but they frequently lost quality due to ‘bending’ when moved.)
The ‘ace in the hole’ ended up being coded aperture—a process that collects large amounts of data in an initial, messy image, which is later computationally reconstructed into higher resolution. The coded aperture is a flat grid that blocks light at random to create a projection similar to poking holes in aluminum foil. Though the initial image is unclear, the computer can sift though, make sense of, and clarify the graphic—with precision. Though the study’s ‘subjects’ were beads arranged on a slide, their results show that, moving forward, high quality images can be obtained in this very small size range.
Another boon for this lensless endoscope is that it need not be moved around to focus on objects at different depths; three-dimensional computational refocusing calculates the light’s origin to determine shape and structure, this feature further protecting technology and tissue alike.
So how small could this system be? Looks like they should be able to get it to fit into the very small 25 gauge needle we use for the Perc-ACLR procedure. That means far less tissue damage than using one of the existing scopes on the market.
The upshot? At the end of the day, the concept of needle arthroscopy is a solid one. The idea that I could one day use our thin and flexible needles to be able to image what the needle sees would be a breakthrough. Less tissue damage, but good image quality would be awesome. Hopefully, we’ll get this new scope in our hands soon!
________________________________________
References:
(1) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447.
(2) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246.
(3) Jaewook Shin, Dung N. Tran, Jasper R. Stroud, Sang Chin, Trac D. Tran, Mark A. Foster. A minimally invasive lens-free computational microendoscope. Science Advances, 2019; 5 (12): eaaw5595 DOI: 10.1126/sciadv.aaw5595

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.