L5-S1 Non-surgical Disc Treatment
L5-S1 non-surgical disc treatment has radically changed in these past few decades. What used to be a sure thing surgery, morphed into injected steroids and now has morphed again into Orthobiologics. Let’s explore one patient’s result to learn.
What Is a Herniated or Bulging Disc?
Axel_Kock/Shutterstock
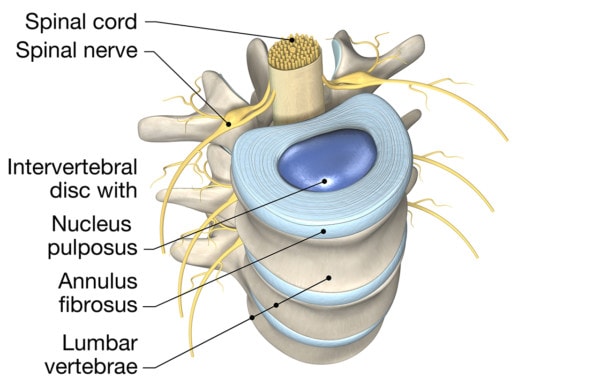
Your discs are the shock absorbers that live between your back bones (vertebrae). On the inside, they have a gel-like substance called the nucleus pulposis, and on the outside, a tough layered structure called the annulus fibrosis.
Designua/Shutterstock
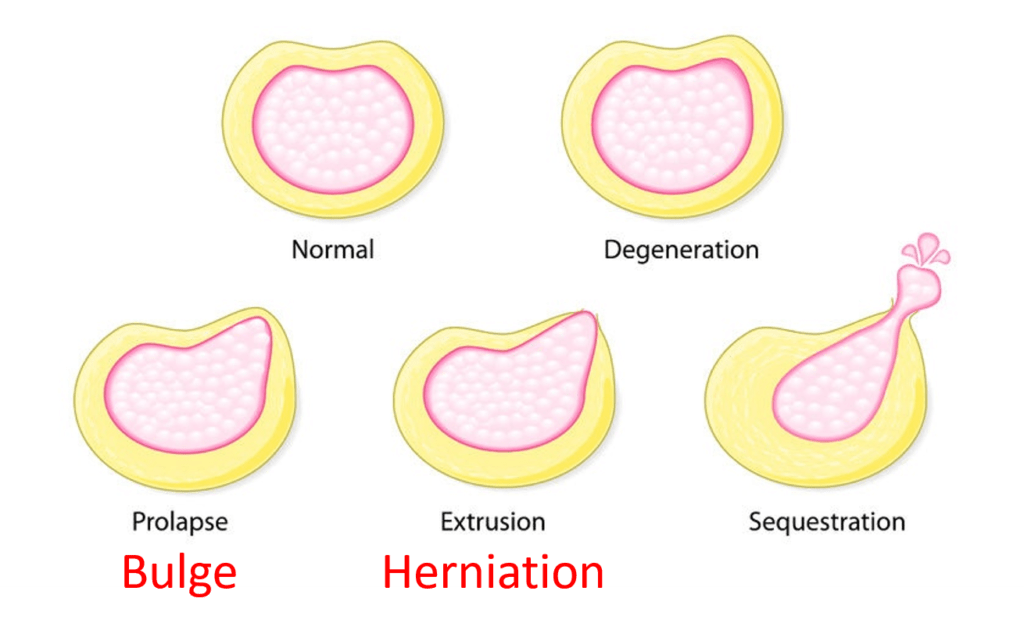
When the inner gel squirts outside of the tough outer covering due to a complete tear in the annulus, that’s called a Herniated or extruded disc. If the outer covering is only partially torn, the inner gel only pouches out the outer covering while remaining contained. This is called a Bulging or protruded disc (1).
Both of these can irritate the exiting nerve. That can cause back pain as well as numbness, tingling, burning, or pressure down one or both legs.
L5-S1 is the bottom-most disc in the low back. Now let’s get into L5-S1 non-surgical disc treatment.
Is There a Better Way?
Old school L5-S1 non-surgical disc treatment is injecting high-dose steroids (2). The problem? Those steroids, while potent anti-inflammatories, can hurt local tissue and reduce the disc’s ability to heal itself.
Our clinic was the first on planet earth to inject stem cells into a disc in 2005/6. Since that time, we’ve learned quite a bit about what works and doesn’t work for L5-S1 non-surgical disc treatment. In particular, for herniated and bulging discs in young and active people, platelet lysate injected outside of the disc (epidural), which contains the growth factors from the patient’s own platelets, can often help get rid of the issue. Othertimes, specially cultured stem cells are needed to get rid of the disc bulge. To learn more about different orthobiologics, see my video below:
I’ve been helping patients with L5-S1 non-surgical disc treatment for almost two decades now using these procedures. There are several more before and after MRI’s of patients we’ve helped in the video below:
This is a research paper we published on the treatment I will review today (3).
Adam’s Story
Adam first saw us as a new patient in 2017 with low back pain since the prior summer. He was gradually getting worse. He desperately wanted L5-S1 non-surgical disc treatment but had so far had poor results from other clinics trying to use orthobiologics on his low back.
He had a prior ultrasound-guided epidural with exosomes by another clinic which initially helped, but then he quickly regressed. Acupuncture was helping for about a day, but deep tissue massage did not help. The patient has also had tried chiropractic adjustments with no relief and was taking Tylenol every other day. Another physician had also injected PRP into piriformis and gluts with amniotic fluid with no relief.
When he was seen, he reported discomfort when standing from a seated position and also pain with bending or reaching. He could only sit for about 30 minutes before he started feeling cramping and shooting pain in the hamstring.
Why did his Orthobiologics treatment to date fail? Frankly, he was getting substandard care. What I mean is that not only was there no need to inject the patient with exosomes and amniotic fluid, but the providers who were offering that care didn’t have the skill level needed to get the Orthobiologic in the right spot. In this case, between his disc and the irritated nerve. That can’t be done under ultrasound, but only using x-ray guidance.
So what did we do differently to achieve L5-S1 non-surgical disc treatment? I injected him twice, once transforaminal using x-ray guidance and a second-time infra-neural, getting even closer to the nerve disc interface. Both of these are techniques that are not possible to do well with ultrasound. I also injected the growth factors from his own platelets and injected other structures as well.
What was the final result? His before and after MRIs are above. The one on the left shows a significant pooch out the back of the lowest L5-S1 disc (protrusion) and the one on the right, shows that this bulge has resolved. He is now 90% better for the long run and came in for a touch-up treatment as he’s extremely active and wants to do more.
The upshot? Adam found an L5-S1 non-surgical disc treatment and got better because of our almost 2 decades of expertise in using Orthobiologics in the low back. That means that where and how you inject the Orthobiologic is as critical as what’s injected.
___________________________________
References:
(1) Appel B. Nomenclature and classification of lumbar disc pathology. Neuroradiology. 2001 Dec;43(12):1124-5. https://www.spine.org/Portals/0/Assets/Downloads/ResearchClinicalCare/Nomenclature.pdf
(2) Pena E, Moroz L, Singh D. Lumbar Epidural Steroid Injections. JBJS Essent Surg Tech. 2016;6(3):e25. Published 2016 Jul 13. doi: 10.2106/JBJS.ST.O.00058
(3) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. Published 2017 Nov 25. doi: 10.1186/s40634-017-0113-5

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.