Marx, Platelet Concentration, and Fake PRP
Image created with ChatGPT 4.
An astute physician colleague this week pointed out that one of the references in my past blog about fake PRP impacts the results of clinical trials needed updating. Hence, in researching that issue this week, I thought this topic would make a great blog. So, how do we define the minimum concentration for PRP? Where does that definition come from? Let’s dive in.
Fake PRP
If you read this blog, you know I’m critical of fake PRP, which I have defined as under 2X in concentration. This means that the device used to make the PRP is so inefficient that it can’t achieve at least double the baseline platelet concentration in whole blood. I referenced Marx (not Groucho or Karl but Robert, a dentist, and early PRP adopter) for that baseline definition.
Where did this 2X minimum come from? How did Marx’s own opinions on the minimum platelet concentration change over the years? How does all of that impact what I have written about fake PRP and an analysis that we are doing on clinical trial failures?
Marx on PRP
Robert Marx is a dentist and early PRP pioneer with many publications in this space. In his first 1998 publication on the use of PRP in dental bone grafts, he used a PRP with a mean platelet count of 595,000/µl with a starting mean count of 232,000/µl in whole blood or 2.25X (1). However, that minimum changes by the time of his next indexed publication in 2001 (2). In this paper, he states:
“Because the scientific proof of bone and soft tissue healing enhancement has been shown using PRP with 1,000,000 platelets/lJ.l, it is this concentration of platelets in a 5-ml volume of plasma which is the working definition of PRP today. Lesser concentrations cannot be relied upon to enhance wound healing, and greater concentrations have not yet been shown to further enhance wound healing (Fig. I).”
This change takes the 2X PRP he used in the 1990s and updates it to essentially 5X on average (assuming a mean normal platelet count of 200,000/µl in whole blood). In this paper, he bases that new definition on this table:

Regrettably, this table doesn’t do much to support this conclusion for 5X, as PDGF (Platelet Derived Growth Factor) is plentiful in platelets and would be expected to increase with a higher platelet count. It’s also not a major growth factor in musculoskeletal tissue repair like TGF-b, b-FGF, or VEGF.
By 2004, Marx provided additional data to support his claim that 5X was better than 2X (3). In that paper, we see this graph:

Here, we see an experiment that seems only to have been presented at a conference and not published in the peer-reviewed literature. Here, we see the platelet fold concentration on the X-axis and mesenchymal stem cell proliferation on the Y-axis. This shows much better proliferation at 5X and 10X than 2.5X. Given that we have done this same experiment often in vitro in our own lab, this data agrees with our internal observations that higher platelet concentrations cause more proliferation in MSCs. However, there’s a catch not discussed by Marx.
The Catch
Everything in life has a catch, and the PRP concentration story concerning helping cells grow and repair is no different. The catch here is that this direct dose response only works (more is better) when the cells are older but falls apart when the cells are younger. After observing this for many years in MSC culture, we did a formally published experiment with young versus old tenocytes. Here, we exposed these tendon cells to various platelet growth factor concentrations made from PRP and then looked at how young versus old cells fared (4):
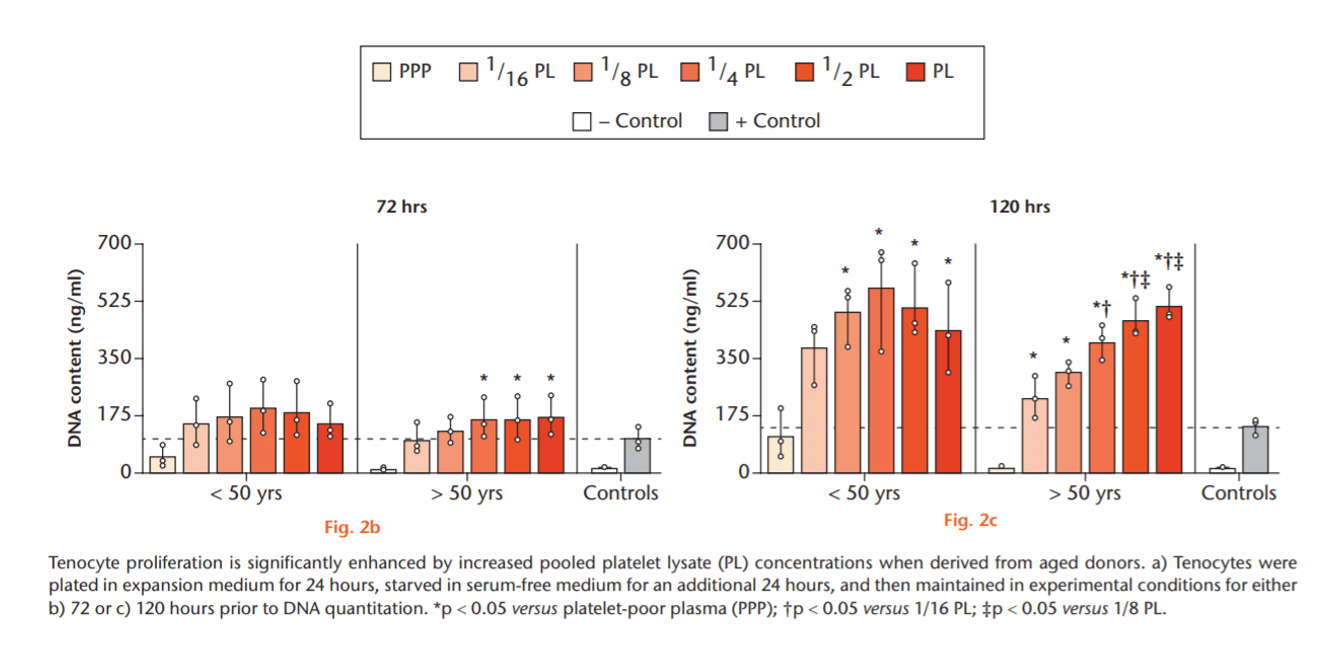
In the young cells to the left, the higher platelet doses quickly max tenocyte proliferation out at low concentrations. In the older cells to the right, the tenocytes show better and better proliferation as the cells are exposed to higher and higher platelet concentrations.

The above graph combines what we found in our 2019 paper and what we have observed. If you expose young cells to PRP, more isn’t better. In fact, for the really young, 2X will do just fine. As the person ages, more is MUCH better. I have discussed why this likely happens in a separate blog.
Hence, Marx was right and wrong with his 2X PRP use and later redefinition to 5X as a minimum. What is “real” PRP for young people is a lower concentration than for older people.
How Can We Use This Data to Define Fake versus Real PRP?
So, where should we set the minimum definition of fake versus real PRP? I have previously stated that Marx felt that line was at 2X, but that’s only partially true. So should it be 2X or 5X? How does that line impact my prior PRP trial failure analysis?
To review, I analyzed all 101 PRP Randomized Controlled Trials using PRP for orthopedic conditions. When I used a threshold of 2X to define “real PRP,” 60% of trial failures occurred in studies that used “PRP” systems that produced a PRP product below this threshold. On the other hand, only 5% of trial failures occurred in trials that used systems capable of producing PRP greater than 2X.
One More Reason
Why use 2X as a cutoff between fake and real PRP? In two words, “clueless academics.” There are two widely used fake PRP systems out there: Arthex ACP and RegenLab. Both systems were used in sophisticated clinical trials by clueless academics. Why would an academic not understand that the devices they used in the study couldn’t get past the 1990s Marx definition of PRP, let alone his new 5X definition? None of these academics had actually used PRP in their daily clinical practices, so this was the blind leading the blind.
What Do We Do?
All of the above is a research analysis. In daily clinical practice, since 90% of our patients are middle-aged and older, we routinely use PRP that is well above 5X. In fact, the lowest concentration we will use in that age group is 7X, and more frequently, 10-20X. Hence, we have been imbibing the higher dose mantra for PRP ever since our early 2007/8 experiments showed that higher doses in older patients caused more mesenchymal stem cell growth.
The upshot? I thank the colleague who pointed out some of the newer Marx publications. Anytime someone enters a new concept into the mix, I try to take a deep dive into the literature and work through the new information relative to what we know. So, while all of this 2X or 5X stuff may be a bit dry, it’s a great way for me to review the literature again to ensure I know which end is up.
____________________________________________________
(1) Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638-46. doi: 10.1016/s1079-2104(98)90029-4. PMID: 9638695.
(2) Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001;10(4):225-8. doi: 10.1097/00008505-200110000-00002. PMID: 11813662.
(3) Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004 Apr;62(4):489-96. doi: 10.1016/j.joms.2003.12.003. PMID: 15085519.
(4) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.