Another New Study Says PRP Dose Is Critical: Why We Have ALWAYS Used High Dose PRP
Physicians who read the orthobiologics literature and follow the latest and greatest have caught onto a message I’ve been delivering for almost two decades. The most critical aspect of PRP is the dose and concentration of platelets delivered to the patient. A new study published last week adds more fuel to that fire. Let’s dig in.
PRP Dose
Since I did my impromptu analysis of PRP study failure related to low doses, a supporting study has been published (2). Before that, a few authors (including us) shouted from the hilltops that dose is critical if you want a good patient outcome (3-5). Despite this, the academics who have pulled the trigger on many well-designed “PRP” studies didn’t seem to get the memo. Instead, millions of dollars were wasted by using platelet preparations that were so low dose that they couldn’t meet even a minimal standard to be called PRP.
How Did I Know This About PRP Back in 2005-2007?
I’ve relayed a few times that way back in 2005, when we were culture-expanding mesenchymal stem cells, we settled on a culture technique that didn’t use fetal bovine serum. That was because, at the time, there was a big issue with cattle prion disease. That caused us to use autologous platelet lysate. That’s made from the patient’s blood. First, PRP is made, and then the platelets are lysed to release their growth factors. Those growth factors stimulate growth in the bone marrow mesenchymal stem cells in culture.
When we cultured these cells, we noticed something. The cells from young patients could easily be cultured with very low concentrations of PL. If you upped the concentration, it didn’t help their cells grow faster. However, for older patients, you could endlessly increase the concentration of PL and get more proliferation of their cells. You could do that up to the practical limits of how much blood you could take to create the PL.
We also wanted to see if this high-dose platelet growth factor phenomenon was the same for other cells, so we replicated it in tenocytes and published that work (4). The message was clear: In middle-aged or older patients, high-dose PRP can goose clinical results.
The New Study
The new research into PRP was a systematic review of those PRP studies that included product characterization. This whittled down the more than 100 RCTs published on PRP to just 29. Here’s the “money shot” or the one factoid that tells the story (the graph is mine):
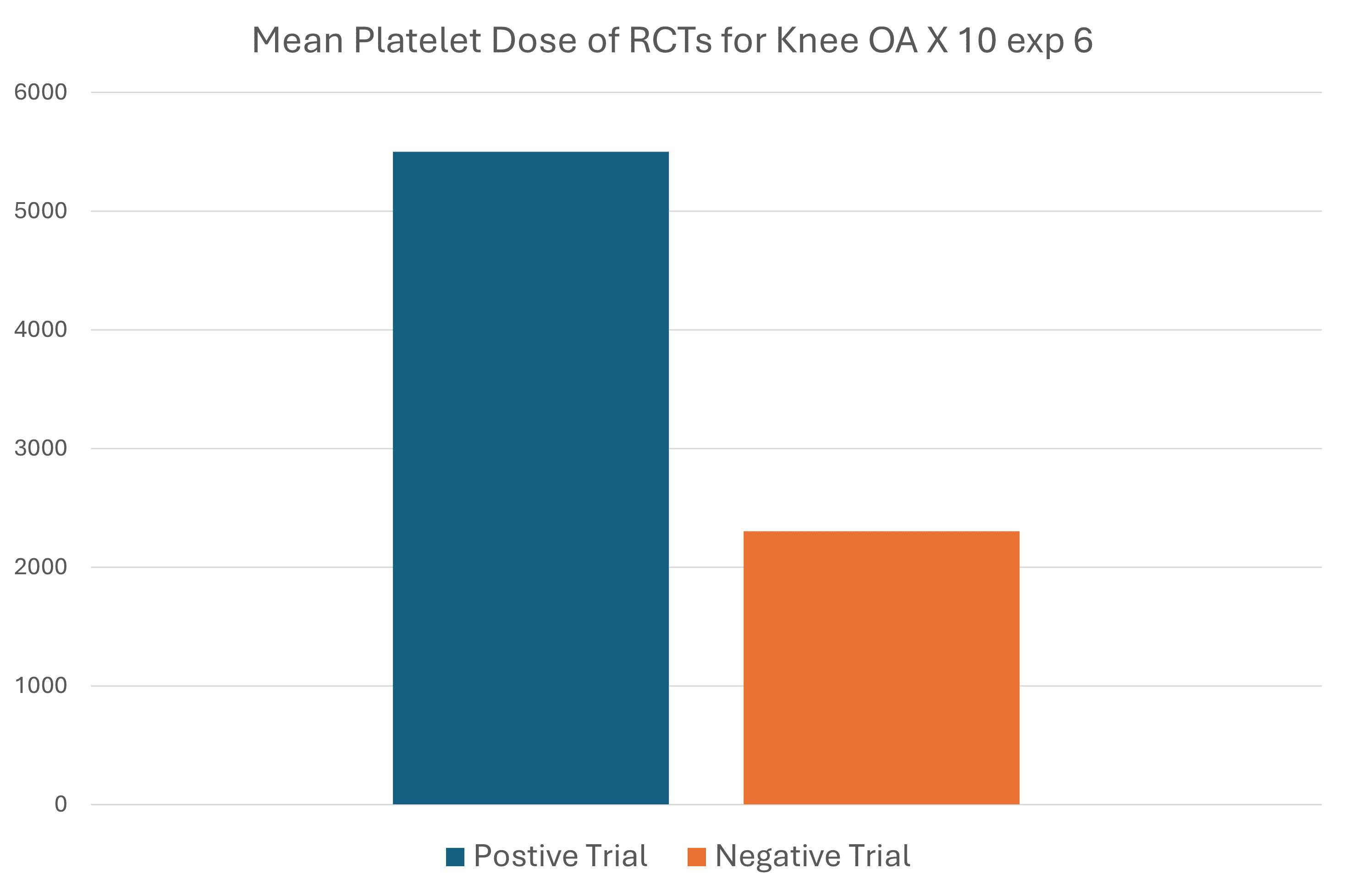
The mean total platelets delivered into knees in a successful RCT was 5500 +/- 474 versus 2302 +/- 437 (10 exp 6 for both)—so 5.5 billion for successful trials and 2.3 billion for unsuccessful ones.
Of the studies they reviewed, 31 treatment arms were reviewed at six months, with only two being negative. At one year, 16/18 treatment arms showed efficacy.
Take Home Message for Physicians and Patients
As I have said, the more platelets you deliver in middle-aged and older patients, the better the results. Based on the published literature, cheap gel tube systems like Regen Lab will likely produce orthobiologic treatment failures. On the other hand, more expensive kits that allow the physician to take more blood and achieve higher concentrations are likely to produce better results.
For patients, it’s all about the amount of blood the clinic takes. For example, any clinic trying to treat knee arthritis that takes only 1-2 tubes of blood is not practicing at a high level. Treating your knees would require 50-100 ml of blood, which is 7-12 tubes.
The upshot? More and more clinical research continues to support theses we created a long time ago. For middle-aged and older patients, high-dose PRP is the only type of PRP that your doctor should use and that you, as a patient, should seek out. In addition, it’s time for us to ask why an academic spending millions of dollars on a clinical trial of PRP uses a kit that can only produce very low concentrations of platelets. On that front, it’s time for academics worldwide to get the memo.
______________________________________
References:
1. Berrigan WA, Bailowitz Z, Park A, Reddy A, Liu R, Lansdown D. A Higher Platelet Dose May Yield Better Clinical Outcomes for PRP in the Treatment of Knee Osteoarthritis: A Systematic Review. Arthroscopy. 2024 Mar 19:S0749-8063(24)00206-8. doi: 10.1016/j.arthro.2024.03.018. Epub ahead of print. PMID: 38513880.
(2) Patel S, Gahlaut S, Thami T, Chouhan DK, Jain A, Dhillon MS. Comparison of Conventional Dose Versus Superdose Platelet-Rich Plasma for Knee Osteoarthritis: A Prospective, Triple-Blind, Randomized Clinical Trial. Orthop J Sports Med. 2024 Feb 26;12(2):23259671241227863. doi: 10.1177/23259671241227863. PMID: 38410168; PMCID: PMC10896053.
(3) Bansal, H., Leon, J., Pont, J.L. et al. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: Correct dose critical for long term clinical efficacy. Sci Rep 11, 3971 (2021). https://doi.org/10.1038/s41598-021-83025-2
(4) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.
(5) Anitua E, Sánchez M, Zalduendo MM, de la Fuente M, Prado R, Orive G, Andía I. Fibroblastic response to treatment with different preparations rich in growth factors. Cell Prolif. 2009 Apr;42(2):162-70. doi: 10.1111/j.1365-2184.2009.00583.x. Epub 2009 Feb 24. PMID: 19250293; PMCID: PMC6496288.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.