The Academic Low Dose PRP Knee OA Problem Is Alive and Well-The Lewis Et al JBJS Paper

Credit: Shutterstock
Academics are hopelessly behind the modern practice of orthobiologics. While there are all sorts of reasons for this, the problem is that it continuously shows up in the literature. This morning we’ll cover a new knee arthritis “PRP” study and review an older one that both made the mistake of not actually using PRP. Let’s dig in.
Academics and Orthobiologics
While there are a few notable exceptions, most academic physicians are way behind the learning curve in orthobiologics. Since our practice runs a fellowship program in this area I see this with our fellows who get jobs in academic centers. In that situation, they are basically unable to use all of the skills they acquired in fellowship because the academic medical center just doesn’t have a box for orthobiologics.
Why? One issue is billing. We would all like to believe that academic medical centers are places of science first and money second. However, it’s actually the opposite. These are healthcare businesses that teach and perform research. Hence, the ability to bill care to insurance companies is the main engine that keeps the financial furnace stoked. Given that orthobiologic therapies like PRP can’t yet be easily billed to insurance carriers, Medicare, or Medicaid, using these products in academia is VERY limited. For example, our private clinic with 6 physicians does more PRP injections in a month than the local university medical center does in a year. This lack of direct experience causes real problems. In essence, academics are less likely to know which end is up based on training and experience in this area. This can often lead to problems that make their way into research studies.
What is PRP?
Platelet-rich plasma is made by taking whole blood and concentrating the healing platelets in plasma. Its first definition for PRP back in 1998 was that the platelets would be at least 2X concentrated (1). The modern definition now used by physicians working with PRP all day is to get that concentration as high as feasible. That’s based on a few studies and lots of clinical experience. For example, the average physician expert in orthobiologics wants to see their PRP concentration at least 3-5X and often 7X or higher. The problem is that few bedside machines used by doctors to make the PRP can attain these higher concentration levels. As an example, at Regenexx, we routinely use concentrations from 7-20X, but that requires a specialized lab platform rather than a simple bedside machine. Most bedside machines require a non-FDA cleared double spin to get above 3-5X.
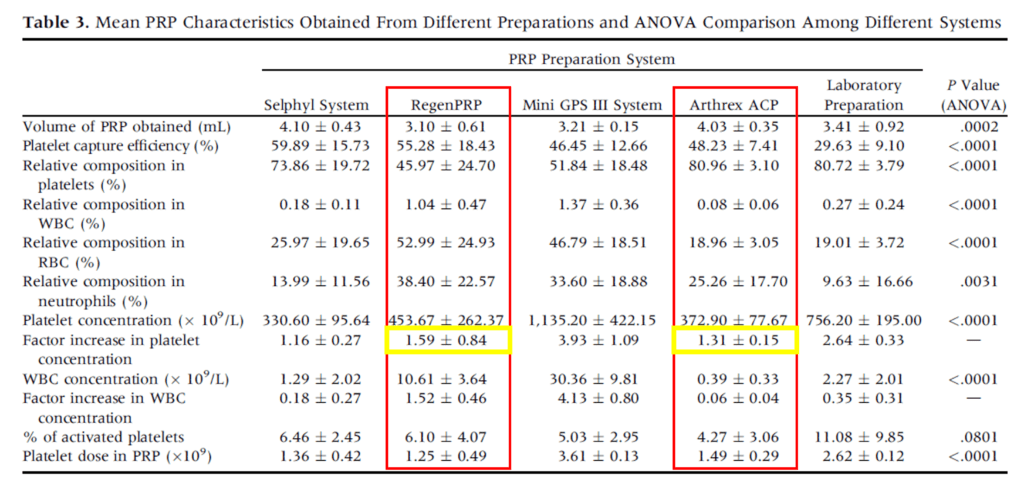
Before we get into these two academic research papers on PRP, let’s dive into the concentration of platelets that the two machines used in these studies produced. Above is a table from Magalon et al who researched the concentration various bedside machines were capable of producing (2). The two we’re focusing on today are in red boxes (RegenLab and Arthrex ACP). In the yellow boxes, you see the concentration attained. RegenLab (here RegenPRP) produces a mean 1.59X concentration. Arthrex ACP manages even less at 1.31X. Hence, the blood products these machines produce don’t meet the minimal definition of PRP as defined by Marx.
Why would otherwise smart academic researchers use these machines? The Magalon paper above was published well before these two new studies were conceived. Why didn’t they get the memo? See the discussion above. Anybody with any experience using PRP would have long since been to conferences where Jeremy Magalon has presented this data and would have known to steer clear of these two devices. I would posit that none of the authors on these two papers had enough experience with using PRP to know about these problems. Meaning they didn’t know what they didn’t know.
The New “PRP” Study
The new study, like the slightly older study, is from Australia. As you’ll see as we dissect this research, there is definitely something going on “down under”. Let’s dive in.
This new research studied 102 patients with knee arthritis and was published in The Journal of Bone and Joint Surgery (3). They randomized mild to moderate knee arthritis patients into three groups: saline alone, PRP alone, and then PRP for the first injection and saline for two more injections. This is the first place where the study gets a bit bizarre. Since three weekly injections of PRP are the least common type of treatment for this type of knee arthritis, this design makes little common sense. For example, if you wanted to compare a single PRP shot to a placebo that would be a comparison to a single saline injection. If you wanted to compare three PRP shots to a placebo, you would obviously compare that to three saline injections. However, it’s a mystery why you would ever combine PRP and saline in the same treatment arm.
In the end, the authors found no differences between the groups. That’s in contradiction to almost two dozen positive RCTs published on the use of PRP to treat knee osteoarthritis (5-23). However, given that this study used the Arthrex ACP device characterized by Magalon et al which produces a pitiful 1.3 X concentration, this study never used PRP (2).
Hence, the original title of this paper was:
- The effectiveness of leucocyte-poor platelet-rich plasma injections on symptomatic early osteoarthritis of the knee: the PEAK randomized controlled trial
But should have been:
- The effectiveness of leucocyte-poor
platelet-richplasma injections on symptomatic early osteoarthritis of the knee: the PEAK randomized controlled trial
The fact that leukocyte-poor plasma doesn’t work better than saline injections for knee arthritis IS NOT SURPRISING.
Why Would a Respected Orthopedic Journal Miss This?
Right now, with orthobiologics not being taught in academic medical centers due to the lack of exposure I described above, what the average orthopedic surgeon who may review for The Journal of Bone and Joint surgery knows about PRP could fit on the back of a postcard in big block letters. Hence, it’s unsurprising that the reviewers for this paper never looked to check third-party studies to see if the Arthrex machine actually produced PRP.
Another Fake PRP Study from the Recent Past
I’ve already blogged on the Bennell et al knee arthritis RCT also from Australia that used the other fake PRP kit that was characterized in the Magalon study, the RegenLab system at a paltry 1.6X! (2,4) Hence, its title gets changed from:
- Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis-The RESTORE Randomized Clinical Trial
To this:
- Effect of Intra-articular
Platelet-RichPlasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis-The RESTORE Randomized Clinical Trial
This is a Real Problem
The vast majority of doctors who will read these studies will only ever read the abstract. Meaning they will assume that both studies used legit PRP rather than just plasma. That has the potential to set the field back.
What Can You Do?
Share the snot out of any post or blog (like this one) that points out this very obvious flaw with these studies (here’s another one to share from my colleague Don Buford, MD). Talk to as many colleagues as you can about these papers. Add the Magalon et al table to your next talk in front of doctors. Just get the word out that these are NOT PRP studies. Finally, talk with your academic colleagues and educate them. Ask them to reach out to you if they’re designing any new studies.
The upshot? Fake PRP studies continue to be produced. These are expensive and resource-intensive studies being done by academics who don’t know which end is up. We all need to call that out.
_________________________________________________________________
References:
(1) Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004 Apr;62(4):489-96. doi: 10.1016/j.joms.2003.12.003. PMID: 15085519.
(2) Magalon J, Bausset O, Serratrice N, Giraudo L, Aboudou H, Veran J, Magalon G, Dignat-Georges F, Sabatier F. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthroscopy. 2014 May;30(5):629-38. doi: 10.1016/j.arthro.2014.02.020. PMID: 24725317.
(3) Lewis E, Merghani K, Robertson I, Mulford J, Prentice B, Mathew R, Van Winden P, Ogden K. The effectiveness of leucocyte-poor platelet-rich plasma injections on symptomatic early osteoarthritis of the knee: the PEAK randomized controlled trial. Bone Joint J. 2022 Jun;104-B(6):663-671. doi: 10.1302/0301-620X.104B6.BJJ-2021-1109.R2. PMID: 35638203.
(4) Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. JAMA. 2021;326(20):2021–2030. doi:10.1001/jama.2021.19415
(5) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
(6) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(7) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
(8) Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
(9) Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
(10) Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
(11) Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
(12) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(13) Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
(14) Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
(15) Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
(16) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
(17) Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
(18) Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
(19) Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
(20) Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
(21) Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
(22) Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-Term Outcomes of Percutaneous Trephination with a Platelet Rich Plasma Intrameniscal Injection for the Repair of Degenerative Meniscal Lesions. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Int J Mol Sci. 2019 Feb 16;20(4):856. doi: 10.3390/ijms20040856. PMID: 30781461; PMCID: PMC6412887.
(23) Chu J, Duan W, Yu Z, Tao T, Xu J, Ma Q, Zhao L, Guo JJ. Intra-articular injections of platelet-rich plasma decrease pain and improve functional outcomes than sham saline in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2022 Feb 6. doi: 10.1007/s00167-022-06887-7. Epub ahead of print. PMID: 35124707.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
