Orthopedics 2.0 Version 3 Sneak Peek! Take this New Stability Test to See Where You Need Work
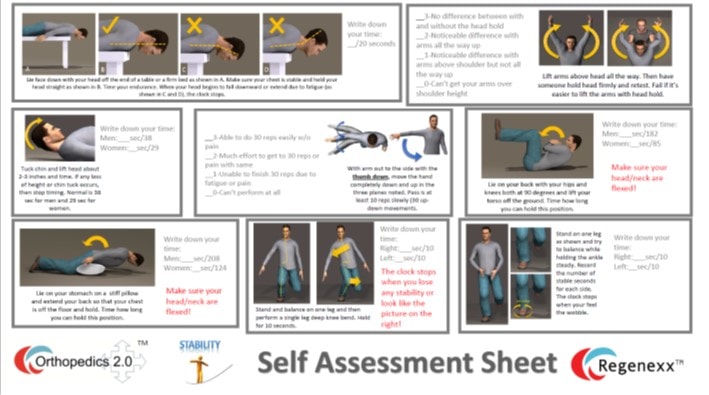
Sorry I’ve been off from blogging for a few days. I needed a little break and then I began working on the third version of our practice’s e-book, Orthopedics 2.0. I should have this done over the holidays so that version 3 comes out early next year. The new book will continue the trend of inter-activity with the reader and add in scoring and updated tests in each major area like stability and symmetry. It will also have our latest registry data and many more updates. The book will also begin to synchronize with the patient experience at our Colorado clinic and then at various network sites. The Stability worksheet is above and here’s the new portion of that chapter leading up to the test. So if you’ve had enough turkey sandwiches to last a lifetime and you want a little challenge, click on the thumbnail above and print out the worksheet. Grade yourself and see where you have issues!
[For this chapter’s illustrations, see the worksheet above.]
Regenexx Simple Muscular Stability Tests
When you get evaluated using the SANS system, these are the quick and simple physical exam tests that will determine if you have good or poor stability. There are also other things that will be evaluated, like the status of your spinal stabilizing muscles on MRI. If you have pain with any of these movements, make sure that you pay attention to the rest of these chapters.
We expect our patients to be participants in their own recovery, so we want them to take this test on a monthly basis when being treated. If you’re a Regenexx patient, before your first evaluation, please take the test, print out the worksheet, and bring it to your first evaluation. If you were given a physical book, you can find the worksheet at the back of this chapter. If you’re not a patient, you can do the same thing by taking the test and filling out the work-sheet to record where you are at any given time (click here for the link to the worksheet)
Caution!These tests may cause injury or exacerbate the conditions of patients who have a more fragile stability system or who are lower level in their stability. Please do not attempt these if you get injured easily. If you do decide to perform this assessment, if you get significant pain during any given test, stop immediately.
Getting Ready: For some of these tests you’ll need an assistant. You’ll also need a timer or clock/watch with a second hand (there are good stopwatch programs on most Smartphones).
Neck: The first test is simple, just lift your arms out to your sides and all the way above your head. Is this easy or hard? Can you easily get your arms up all the way? Now have someone stand behind you and hold your head very firmly. Your head shouldn’t move at all as you perform the same hands over head maneuver. Was it easier to lift your arms with your head stabilized by someone? If you found it hard to lift your arms over your head without someone stabilizing your head, then you may have upper cervical instability. This means that the muscles or ligaments stabilizing your upper neck may not be strong enough. If you experience significant pain with this maneuver, stop!
Scoring: If you feel no difference between with and without the head hold, then give yourself a 3 here. If you feel a noticeable difference and can get your arms all the way up you score a 2, if you feel a difference and get your arms over your shoulders but not all the way up-you score a 1, if you can’t get your arms over shoulder height give yourself a 0.
The second neck test was developed by an Australian researcher and is a bit more challenging. Lie on a flat and firm surface like the floor and have someone time and monitor you. First tuck your chin fully and then lift your head 2-3 inches. Have your monitor start the timer. The clock stops when you lose any of the chin tuck or your head is unable to maintain the same height. Normal for men is 38 seconds and for women is 29 seconds. If you can’t do this, your deep neck flexors are weak and you fail this part of the test. These are important muscles that stabilize the front of your neck. When these muscles are weak, patients often report headaches. If you experience significant pain with this maneuver, stop!
Scoring: Just write down your timed score.
The third neck test was developed by a U.S. physical therapist and tests the endurance of the deep and superficial neck muscles that hold your head up. You first lie face down on a table or firm bed, making sure your chest is stable (you may want to have someone hold you by placing downward pressure on your upper back). You then hold your head perfectly straight, with the face parallel to the floor. You hold this position and time yourself. You should be able to get to 20 seconds without your neck and head bending (as shown in C) or extending (as shown in D). If you went into position C as you fatigued, your superficial neck extensors are weak. These help to hold your head up. If you went into position D, your deep neck extensors are weak and the superficial extensors are taking over. In both of these instances, patients with weak neck extensor muscles tend to report a heavy head or fatigued neck by the end of the day. If you experience significant pain with this maneuver, stop!
Scoring: Just write down your timed score.
Shoulder: The test for the shoulder focuses on rotator cuff muscle endurance. The arm is held out to the side with the thumb facing down and pointing toward the floor. The arm is then moved down toward the side and back up to shoulder height. You perform this movement in the three planes shown (behind the body, at the body, and in front of the body). Do this slowly. If you experience significant pain with this maneuver, stop! You should be able to do this ten times in each position (30 reps total). You may be fatigued. If you can’t get that far without stopping, you need to strengthen the rotator cuff. These muscles help to stabilize the ball of the shoulder joint in its socket.
Scoring: If you can get through 30 reps (10 in each plane) without pain (although you may be mildly to moderately fatigued), then give yourself a 3 here. If you can do this barely with much fatigue and effort or have pain with this test, then you score a 2, if you can’t get through all of this due to fatigue or pain you score a 1, if you can’t do this at all give yourself a 0.
Low Back: There are two stability tests for the lower back, both pioneered by a Japanese researcher. The first is a simple sit-up maneuver where you begin by lying face up and bringing your hips and knees to a 90 degree position as shown. Make sure you keep your neck flexed. Set a timer and hold this position. The normal time for men is 182 seconds (3 minutes) and for women 85 seconds (1 and a half minutes). If you experience significant pain with this maneuver, stop!
Scoring: Just write down your timed score.
The next test starts with lying face down on the floor and placing a firm pillow under your stomach with your hands at your side. The pillow should be firm enough or doubled up so that you can extend your back and lift your chest off the floor as shown. Your neck should remain flexed. Set a timer and hold this position. For men, the normal hold is 208 seconds and for women it’s 124 seconds. If you experience significant pain with this maneuver, stop!
Scoring: Just write down your timed score.
Hip/Knee: There is a single test for hip and knee stability, as both of these are linked. Here you stand and then balance on one foot (the side you want to test). You then perform a single leg squat while trying to keep your body as straight as possible. If you’re able to balance so that you’re straight for about a ½ deep knee bend and for the return back up, then you pass the test on that side. If you must tilt your body over to that side and/or your knee drives inward, you have poor hip and knee stability and fail the test. If you can’t perform the half squat, you fail as well.
Scoring: Write down your timed score for each side as the number of seconds you can hold that side so that you look the picture to the left above versus the right.
Ankle: You can test the ankle from the same standing on one leg position. Count to ten while balancing on one leg and watch your ankle. With your body straight (which is again measuring your hip stability) and hands to your sides, does the ankle roll or have to move back and forth over that ten seconds? If so, you have an unstable ankle. If not and the ankle remains rock solid for the 10 seconds, you pass this test. If you have a tough time with this, you may have an ankle stability issue. This can impact things all the way up to the knee and can even in some patients cause a knee cap issue.
Scoring: Write down your timed score for each side as the number of seconds you can hold that side so that the ankle is stable.
What if I failed some of these tests? This means you have poor stability in these areas. This could be due to pain shutting down muscles, weak muscles, or irritated nerves that make the muscles weaker or misfire. If it’s pain, then you have to find and fix the source of that problem. If it’s weak muscles, then they may just need strengthening. Finally, if its irritated nerves, no amount of getting the muscles stronger will help, you need to reduce the nerve irritation. These things will all be covered later in the book.
As you get treated, use this Regenexx Stability Test as your monthly spot check to gage your progress. You want to increase your scores in each problem area.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.