Setting an Ethical Framework for Preventative Orthobiologics
Anyone practicing legit high-level Interventional Oorthobiologics (IO) has had the experience of a patient asking to have an area or body part treated just because that patient has some degenerative changes on imaging but no symptoms. As a field, I would argue that we are the first physicians in history to begin addressing this dilemma for degenerative musculoskeletal conditions. So, what makes sense, and what’s possible malpractice? Let’s dive into this issue.
The Issue
A young patient walked into my Cayman clinic this week with multiple disc bulges on his MRI but very few symptoms. What should I do?
A 40-something has right knee OA, which is symptomatic, but the left knee has very mild chondromalcia but is NOT symptomatic. What should you do?
Both patients want to get treated and will be unhappy if we deny access to treatment. Where should we draw this ethical line?
The Disc Conundrum
Injecting a spinal intervertebral disc can cause a mess of a clinical situation. First, there is discitis, which upsets the bacterial balance of the disc, usually causing P. acnes to overgrow. That leads to IV antibiotics and, usually, surgery to lavage the disc. Next up is damaging the disc by placing a hole in it. Finally, there’s a controversy about whether the contrast we inject into discs can injure the cells inside the structure (3,4).
Obviously, a disc causing pain and disability (discogenic pain) would be a reasonable injection target as long as the patient understands the risks weighed against the possible benefits. Even here, I would argue for expanded informed consent, meaning an actual conversation with the patient.
Estimates of the incidence of discitis vary from 0.44% to 0.15 (2). This equates to a 1 in 227 to a 1 in 667 risk. I tell my patients there is a 1 in 300 chance of this happening (2). If it does occur, there will likely be severe, unrelenting pain, the need for IV antibiotics, and likely surgery. It’s amazing how many patients don’t want the procedure after that discussion.
Much less clear is what to do with degenerative discs that are probably asymptomatic. My patient this week had relatively mild axial low back pain symptoms. One physician had already injected the T10-T11, T11-T12, L1-L2, L2-L3, L3-L4, L4-L5, and L5-S1 discs with fibrin glue, which didn’t help. Looking at his MRI, performing an exam, and taking a careful history, you could make an argument that maybe 3 of these discs were possibly symptomatic and degenerative. Given that we were using hypoxic-conditioned MSCs and that we observed that this cell type, when properly injected, can reduce the size of disc bulges, I opted to treat L3-S1 and leave the others (5,6). My patient was a bit upset as he felt that the other discs were abnormal based on his MRI and should be injected as well. I didn’t bite on that argument. More on that calculus below.
The Mild OA Knee, Which Is Asymptomatic or Minimally Symptomatic
Now, let’s change up the risk calculus a bit. Let’s say the procedure is a simple intra-articular injection in the knee joint. What’s the risk of an ultrasound-guided PRP injection? For infection, the risk for various types of injections from a review are (1):
“Iatrogenic septic arthritis (SA) has been reported in patients following hyaluronic acid, steroids injections and even ozone (8-10). The risk of iatrogenic SA has been estimated at 0.005% and 0.0002% for joint injections (9).”
This equates to 1 in 20,000 to 1 in 500,000. Hence, it’s much less risky to inject a knee joint than a disc. If the knee were to be infected, it would be the same clinical mess, often requiring IV antibiotics and usually surgical lavage.
Disease Modifying or Not?
The whole reason for using orthobiologics in preventative situations is to reduce the need for future care. Hence, if the orthobiologic injection is used this way, there should be good evidence that it can modify the disease. Take the disc example above. Do we have solid evidence that injecting PRP, BMC, or even hypoxic culture-expanded MSCs into a disc can improve the progression of degenerative disc disease? While we and a few others have reported cases where that seems to occur, we have no good randomized controlled trial showing a deceleration of the degenerative cascade occurs in most patients.
On the other hand, take the knee OA example with PRP. Several studies using higher doses, 2X and above, show that PRP can modify or improve the progression of knee osteoarthritis.
A Framework for Preventative Care
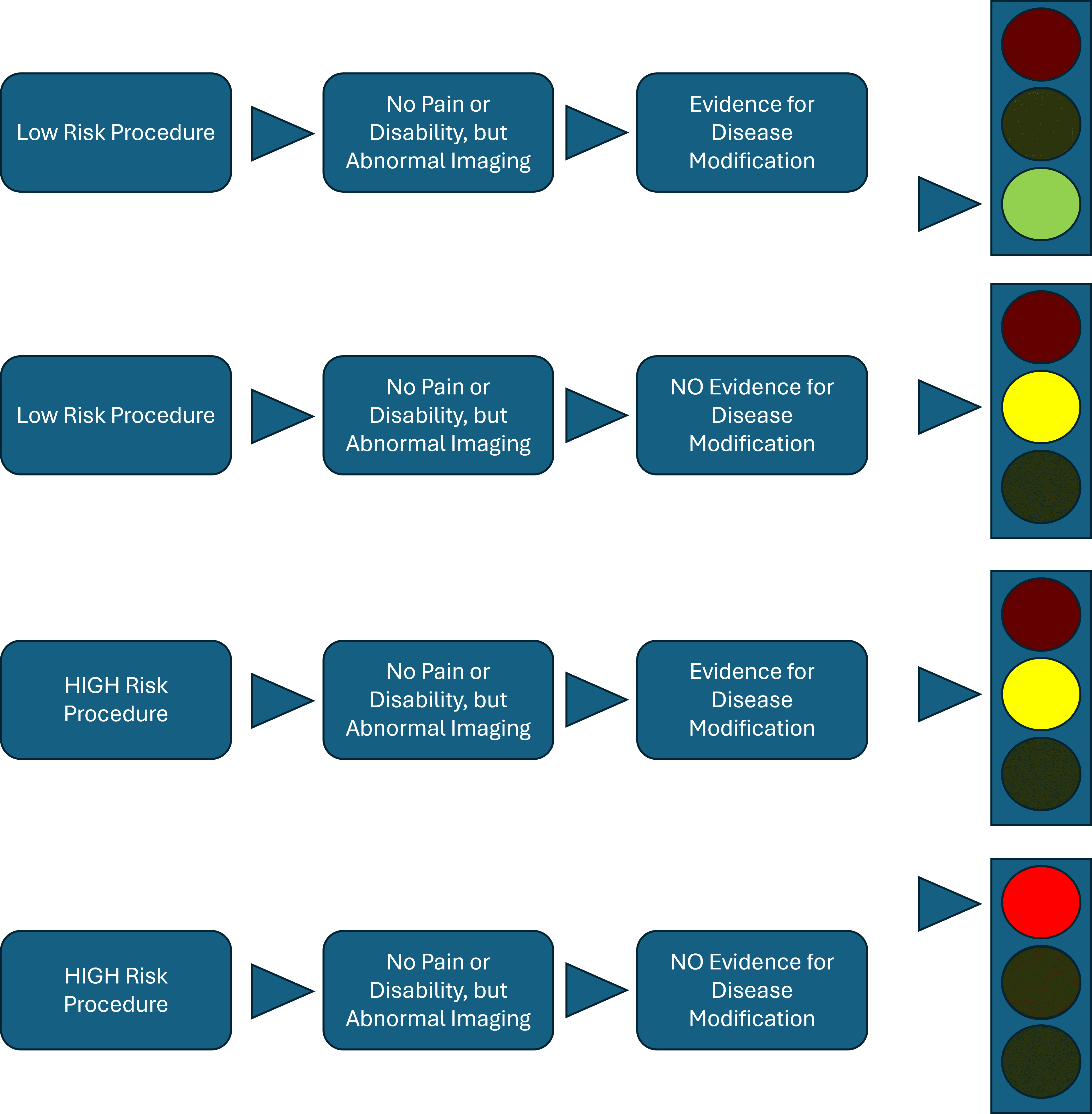
This framework assumes that the patient has no pain or disability but has abnormal imaging findings. As you can see in the topmost row, preventative care makes sense in low-risk procedures like our knee OA case, given that we have evidence that PRP is a DMOAD. Other interventions may or may not, depending on whether there is evidence of that biologic reducing the progression of OA. Hence, the green light.
In the middle row, I have a yellow caution light in cases where the evidence of disease modification is unclear. After expanded informed consent, this decision would have to be made between the patient and the physician. The same would hold for a high-risk procedure with clear evidence of disease modification, which would be left up to the doctor and patient after careful discussion.
In the lowest row, for high-risk procedures like a disc injection, this isn’t justified when there is no evidence of disease modification. That scenario gets a red light. So, for example, the fibrin glue injections in asymptomatic but radiographically abnormal discs have no evidence of disease modification and would violate this ethical framework.
Thoughts on Ethics in Interventional Orthobiologics
Ethical conundrums abound in the regenerative medicine world. For example, people getting IV umbilical cord stem cells for anti-aging before there is clear evidence that these cells will reduce aging. That’s an ethical mess, as while an IV is low risk, the cells’ long-term risk is unknown. I have put this ethical framework out there because I want Interventional Orthobiologics to be better than the anti-aging idiots I see offering these treatments. Meaning if IO doesn’t begin holding itself to self-imposed ethical frameworks, it will NEVER become a widespread standard of care.
The fact that most IO is still being done in a cash payment scenario often means there is little oversight. While many physicians love to hate insurance companies, they can instill basic evidence-based frameworks on what should get paid or not by a third party. Without that oversight in IO and a heavy profit motive to give in to the patient’s wishes, we need to be extra vigilant.
The upshot? Please consider patient risk when deciding if you should inject structures that are likely not causing pain or disability. If we don’t do this as a field, someone else will impose it on us.
__________________________________________
References:
(1) Larghi MM, Grassi M, Placenza E, Faugno L, Cerveri P, Manzotti A. Septic arthritis following joint injections: a 17 years retrospective study in an Academic General Hospital. Acta Biomed. 2022 Jan 19;92(6):e2021308. doi: 10.23750/abm.v92i6.10425. PMID: 35075093; PMCID: PMC8823561.
(2) Kapoor SG, Huff J, Cohen SP. Systematic review of the incidence of discitis after cervical discography. Spine J. 2010 Aug;10(8):739-45. doi: 10.1016/j.spinee.2009.12.022. Epub 2010 Feb 19. PMID: 20171935.
(3) Carragee EJ, Don AS, Hurwitz EL, Cuellar JM, Carrino JA, Herzog R. 2009 ISSLS Prize Winner: Does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine (Phila Pa 1976). 2009 Oct 1;34(21):2338-45. doi: 10.1097/BRS.0b013e3181ab5432. Erratum in: Spine (Phila Pa 1976). 2010 Jun 15;35(14):1414. Carrino, John [corrected to Carrino, John A]. PMID: 19755936.
(4) Cuellar JM, Stauff MP, Herzog RJ, Carrino JA, Baker GA, Carragee EJ. Does provocative discography cause clinically important injury to the lumbar intervertebral disc? A 10-year matched cohort study. Spine J. 2016 Mar;16(3):273-80. doi: 10.1016/j.spinee.2015.06.051. Epub 2015 Jun 29. PMID: 26133255.
(5) Centeno, C., Markle, J., Dodson, E. et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med 15, 197 (2017). https://doi.org/10.1186/s12967-017-1300-y
(6) Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016 Sep 1;14(1):253. doi: 10.1186/s12967-016-1015-5. PMID: 27585696; PMCID: PMC5009698.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.