Stem Cell Therapy for Back Pain? Many Different Types

When our clinic first injected stem cells into low back discs in 2005/6, there was no textbook as to how this should be done. Frankly, sitting here writing this a decade later there is still no textbook, just a collection of weekend courses now shut down due to COVID. So today I’d like to let you in on stem cell therapy for back pain secrets your doctor likely doesn’t know that could impact your results. Let’s dig in.
Stem Cell Therapy for Back Pain
The biggest issue I see out there right now is that what’s called stem cell therapy for back pain varies so widely that one procedure bears no resemblance to the other. I can break down this huge disparity into three components:
- What‘s Being Injected?
- Where Is It being Injected?
- How Is It Being Injected?
Until you as a consumer understand all three of these things, you’re a set-up to get scammed by a clinic by paying top dollar for a procedure that has little chance of success.
What’s Being Injected?
What Orthobiologic?
Orthobiologics are substances that can help tissues like bones, joints, tendons, ligaments, muscles, and discs heal. They come in many different categories, but the three you’re most likely to see used to treat back pain are:
- PRP – Platelet Rich Plasma-Concentrated platelets from the patient’s own blood.
- Autologous Stem Cells – The only type of stem cells taken from the same patient and used in that patient (autologous) come from the bone marrow. This is also called bone marrow concentrate or bone marrow aspirate concentrate (BMC or BMAC). While there are some clinics using stem cells derived from fat, this is technically not legal per FDA.
- Allogenic “stem cells” from Birth Tissues – You’ll notice that I didn’t capitalize the word “stem cells” and that I have it in quotes. That’s because multiple studies have now shown that the products that clinics use that are derived from the umbilical cord or amniotic tissues have no living stem cells (1-3). This is likely the OPPOSITE of what you’ve been told.
In our experience, most spinal conditions respond well to platelet based therapies. That means PRP (platelet-rich plasma) or a derivative product used in different tissues like platelet lysate. BMC/BMAC works well in patients with disc pain due to a tear or that 20-30% of patients that don’t respond to PRP. The birth tissue products that claim to be stem cells are basically hyper-expensive PRP. Meaning, if they work at all (there is very little research that they do), the effect comes from the same type of growth factors that live in your own platelets.
Where Is It Being Injected?
Here I mean what structure is being injected? This is usually where a massive bait and switch happens. Let’s explore this problem.
First, you need to understand that this is a shortlist of things that can be damaged and hurt that may need to be treated with orthobiologics:
- The disc between the vertebra
- The vertebra bone
- The facet joints (finger-sized joints that occur two at each spinal level)
- The main spinal ligaments-too numerous to name here
- Ligamentum flavum (involved in spinal stenosis)
- The area around an irritated nerve (epidural)
- The muscles
The biggest problem in this category is that most of what’s called stem cell therapy for back pain is actually a simple muscle or superficial ligament injection that any first-year medical student or nurse can do. These other structures listed all take significant training and expertise as well as x-ray guidance. They therefore can only be performed by physician super-specialists. Hence the nurse who injects you at the local chiropractic office will have no idea how to get those dead stem cells into these other areas.
To learn more about all of these structures and orthobiologics, see my video below:
How Is It Being Injected?
Here we have three main options:
- Blind
- Ultrasound guidance
- Fluoroscopy guidance
Blind is what it sounds like. A doctor sticks a needle into the tissue and tries to aim the best he or she can, but in the end, has no way to confirm that the cells are going where they should go. In the case of back pain, these are often simple muscle trigger point injections. All of those other structures above are left uninjected. Hence, this really isn’t advanced care, it’s taking the simplest route to get money from the patient.
Ultrasound guidance is using soundwaves to guide the needle. This is a great technology to use in superficial tissues like tendons or ligaments around the knee, but in the spine, it can only be used for a few deeper applications like some facet joints and some easier to perform epidurals. Hence, while it’s a step up from injecting stem cells blind, it’s only a half step.
Fluoroscopy is using x-ray guidance to guide the needle. The advantages in the spine for fluoroscopy are that you can see the deep structures and exactly where the cells will go. Hence, you can inject everything from the disc to the facets to deeper ligaments with high accuracy. The big disadvantage to fluoroscopy is that it costs about 4 times as much as ultrasound to purchase and it costs much more to maintain and run. In addition, the learning curve for fluoroscopy guided spinal injections is steep, so they take years to master.
To learn more about how orthobiologics are injected into discs with fluoroscopy, see my video below:
How Is It Being Injected – Part II
So let’s say you find an experienced interventional pain management physician with many years of experience performing fluoroscopy-guided injections who has recently decided to add stem cell therapy to his or her practice. That’s your choice to get stem cell therapy for back pain. You’re done, right? Maybe. Let’s dig in here.
You now have to vet the degree of knowledge that this provider has in regenerative medicine. Regrettably, this part is the hardest of all for a non-physician expert to vet. Why?
Let’s take two simple examples:
- A Disc Injection
- The Pain Generator vs. The Functional Spinal Unit
A Disc Injection
You go to the doctor and he or she says that you need a low back disc injection. The doctor is trained to perform disc injections and uses fluoroscopy. So how hard could it be to now place stem cells at that spot? Turns out 9 in 10 physicians won’t know how to do that to protect the cells.
Consider these two images below:
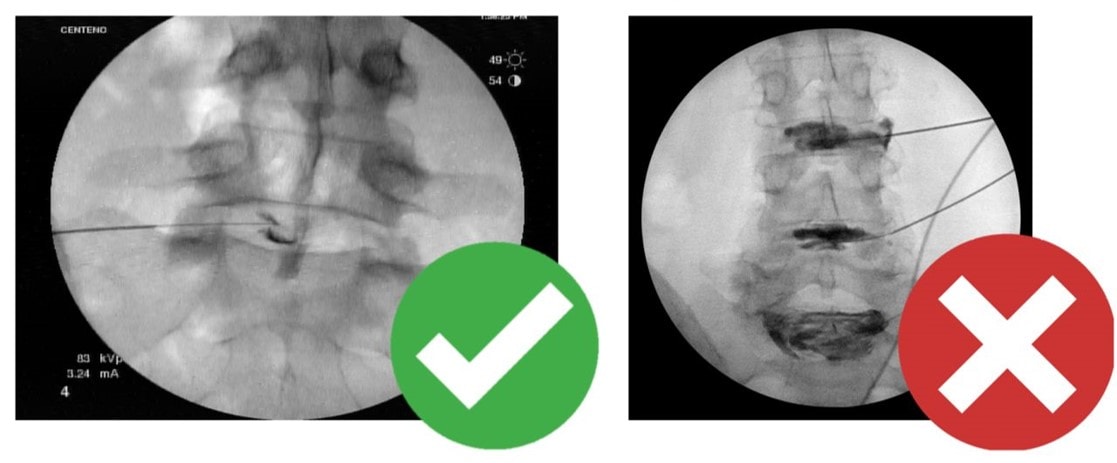
In the one on the right, the doctor has tried to place stem cells by injecting quite a bit of radiographic contrast (the dark stuff). That’s how physicians were taught how to inject the disc because the goal was to use the contrast to see if the disc was torn. However, that’s a serious problem for your stem cells as these contrast agents are toxic to cells, hence injecting too much means killing your stem cells!
In the image on the left, the doctor has injected just a tiny amount of contrast to demonstrate that he or she is in the disc. That amount of contrast is safe with your stem cells, so that patient will get the maximum benefit from the procedure.
We haven’t even gotten into the topic of local anesthetics, where your doctor may inject medications like Marcaine (Bupiviciane) which also kills stem cells rather than the cell-friendly alternative Ropiviciane. Hence, something as simple and seemingly inconsequential as which anesthetic is used could make a HUGE difference. For interventional pain physicians this is a big issue, as most routinely use the cell toxic anesthetic Marcaine.
As you can see, proper stem cell therapy for back pain is more than just adding stem cells to an interventional pain practice. Something as simple as how the disc is injected makes a huge difference. So if the doctor you chose hasn’t been extensively retrained on how this all works, which is about 9 in 10 doctors you could choose, then he or she will botch this procedure. This is just one simple little part of how orthobiologics are injected into the spine. Now let’s expand that a bit so we can learn more.
The Pain Generator vs. The Functional Spinal Unit
Now we get to the level that separates the wheat from the chaff. Meaning, will the physician understand stem cell therapy for back pain at a deep enough level to know where the orthobiologic should be injected? Or will they just try to use orthobiologics like they use a steroid or numbing shot?
Most doctors who are trained in interventional spine using fluoroscopy have been taught that it’s their job to identify “The Pain Generator”. That means the one or two structures in the spine that are causing most of the pain. Why? Because the end goal is to burn or block the nerves with radiofrequency ablation or an implantable stimulator. For these physicians, the use of orthobiologics is simply substituting the corticosteroids or the anesthetics that they usually inject with orthobiologics. However, by doing this they are dramatically reducing the efficacy of the therapy. Let me explain.
For those few of us who have made interventional orthobiologics our career (or who is one of the founders of the whole specialty), the approach is called treating “The Functional Spinal Unit”. This means focusing our injections on all of the parts and pieces in the spine that are damaged like loose ligaments, atrophied stabilizing muscles, irritated nerves, arthritic joints, etc… Let’s dig into one common problem that causes low back pain to illustrate the difference between these two approaches.
The facet joints in your low back are finger-sized articulations between the back of any two vertebrae. They can be injured or get arthritis like any other joint and can cause pain. For the traditional pain generator approach, all the doctor needs to know is that one or more facet joints is causing pain. Then the goal is to temporarily block the pain in these with numbing shots to determine if that specific joint is causing most of the pain. Hence, once that’s done, the doctor will usually burn the nerves that carry pain signals from the joint in a procedure called radiofrequency ablation (RFA).
What most physicians won’t tell you is that there is a dark side to RFA. By burning those nerves, the doctor also kills the stabilizing muscles at that level and makes the spine more unstable in the long run, leading to more facet joint damage. If that same doctor begins offering orthobiologics their focus will be on injecting the joint with that substance (let’s say bone marrow concentrate). While that’s certainly better than burning nerves, it’s doesn’t address how the facet got damaged in the first place.
If we look at the facet joint problem from a functional spinal unit approach, it’s a completely different ball game. In this case, the doctor realizes that the facet joint became painful and arthritic because of lax ligaments, stabilizing muscles that atrophied, and irritated nerves that hammered those muscles. Hence, orthobiologics need to be placed in ALL of those areas to get the maximum benefit for the patient for the longest period of time.
Price
I hope you can now see that there are stark differences in what’s called stem cell therapy for back pain. However, those differences often aren’t reflected in the price of the procedure. Meaning a simple muscle trigger point injection with dead umbilical cord stem cells delivered by a barely trained nurse costs about the same as live bone marrow stem cells delivered by a physician super-specialist to many areas using fluoroscopy guidance. Hence, the value for the consumer is learning how to spot high-quality clinics from low-quality clinics. One way to find a high-quality clinic is to do your homework as described. An easier way is to choose a Regenexx Network physician who specializes in the spine.
The upshot? At the end of the day, there are HUGE disparities in what’s called stem cell therapy for back pain. You really need to do your homework to avoid getting scammed or to avoid ending up in a place that really doesn’t know how to treat the spine with orthobiologics, but is offering “stem cells” because they have seen their competitors do it. So please dig deep before you pull the trigger on orthobiologics for your spine!
_____________________________
References:
(1) Berger D, Lyons N, Steinmetz, N. In Vitro Evaluation of Injectable, Placental Tissue-Derived Products for Interventional Orthopedics. Interventional Orthopedics Foundation Annual Meeting. Denver, 2015. https://interventionalorthopedics.org/wp-content/uploads/2017/08/AmnioProducts-Poster.pdf
(2) Becktell L, Matuska A, Hon S, Delco M, Cole B, Fortier L. Proteomic analysis and cell viability of nine amnion-derived biologics. Orthopedic Research Society Annual Meeting, New Orleans, 2018. https://app.box.com/s/vcx7uw17gupg9ki06i57lno1tbjmzwaf
(3) Panero, A, Hirahara, A., Andersen, W, Rothenberg J, Fierro, F. Are Amniotic Fluid Products Stem Cell Therapies? A Study of Amniotic Fluid Preparations for Mesenchymal Stem Cells With Bone Marrow Comparison. The American Journal of Sports Medicine, 2019 47(5), 1230–1235. https://doi.org/10.1177/0363546519829034

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.