The Evidence Supporting Common Orthopedic Surgeries Is AWFUL

Credit: Shutterstock
I’ve been blogging on the evidence base behind orthopedic surgery for years and I’ve taken HUGE amounts of flak from a handful of orthopedic surgeons who don’t like my approach. Now a new British Medical Journal study confirms what I’ve been saying for the last decade-plus, common orthopedic surgeries have embarrassingly poor evidence. Let’s dig in.
The BMJ and Orthopedic Surgery
While the orthopedic research alarm has been raised in many different studies and reviews since the early 2000’s, my favorite was a 2015 letter to the editor of the British Medical Journal entitled, “The evidence base for orthopaedics and sports medicine: scandalously poor in parts” (1). First, I loved the adjective “scandalously” as it’s just so darn British. Second, the letter concluded that about 80% of common orthopedic surgeries don’t have adequate evidence of efficacy. However, a brand new BMJ article ups the ante from there, blowing away the old one. Before we see how much water the HMS Ortho has taken on, let’s review how much this stuff costs.
Orthopedic Surgery Spending
There are about 7 million orthopedic surgeries a year in the United States and getting a handle on how much is spent here is tough as the US is a patchwork of private insurance companies and public programs, but this quote is interesting (2):
“In 2017, elective orthopedic procedures for BCBS…cost the organization about $25 billion. Elective orthopedic procedures are estimated to be 47 percent of total spend for orthopedic treatments. Since 2010, this amount has grown approximately 44 percent.
Between 2010 to 2017, the greatest expensive increase has been the number of knee and hip procedures across all age segments of the BCBS insured population. For example, in 2017, 242,000 adult BCBS members below the age of 65 had a knee or hip implant.”
So for just one large insurance company, 25 billion is spent annually on orthopedic surgery with about half of that in elective procedures. In addition, that includes hundreds of thousands of joint replacements. So we can say with some confidence that when all programs are considered, 100+ billion annually is not unrealistic for total U.S. orthopedic surgery costs.
However, what if, most of that spending was being wasted? That would qualify as one of the biggest financial missteps in history. In steps in the new BMJ research.
The 10 Most Common Orthopedic Surgery Procedures
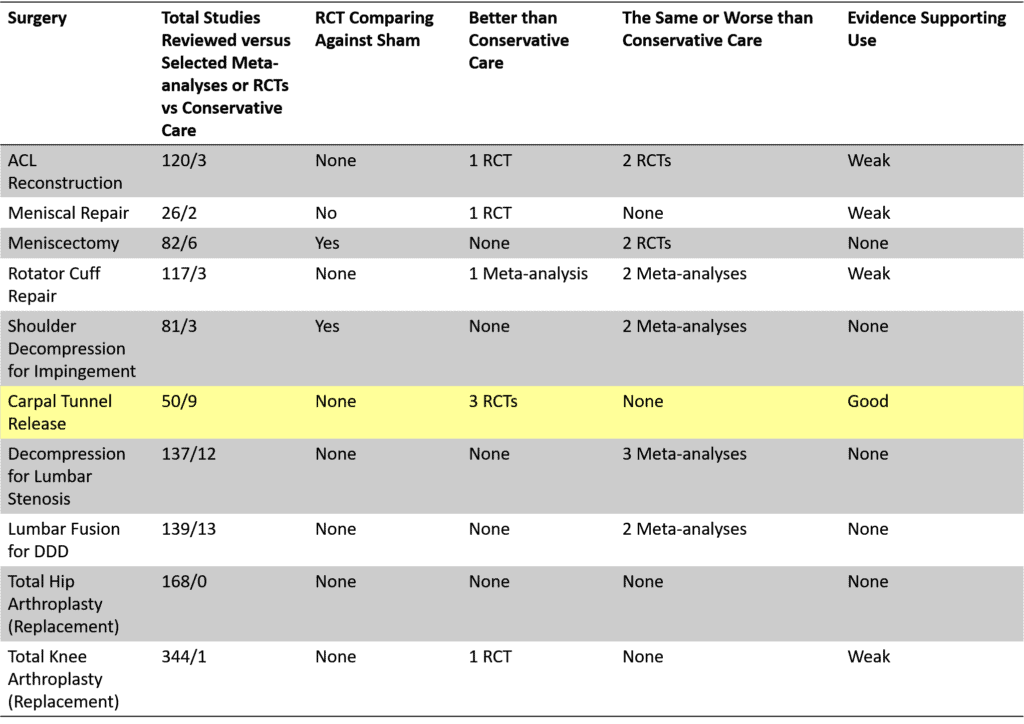
I created the table above after reading a recent research article published by scientists within the UK hospital system and National Health Service (3). This was a Herculean effort where the authors reviewed thousands of published orthopedic surgery studies and ultimately chose 1,264 articles for further review. Their focus was to find research that compared orthopedic surgery to conservative care or a sham procedure (a placebo surgery). Why?
The standard for all research on invasive procedures is to make sure that they can pass the test of being better than less invasive therapies with fewer complications. That’s not rocket science, just plain old common sense. In these studies, the less invasive “conservative care” could be injections, physical therapy, or other non-surgical treatments.
The top 10 most common orthopedic surgeries are listed above that account for most of all elective, non-emergent surgeries. On the left above you can see the surgery and then the following columns:
- Total Studies Reviewed versus Selected Meta-analyses or RCTs vs Conservative Care – The number of studies that the authors were able to select followed by the number of studies that compared surgery versus conservative care or sham
- RCTs Comparing Against Sham – Whether or not any study pitted the surgery versus a placebo.
- Better than Conservative Care – How many studies of which type showed that the surgery was better than conservative care?
- The Same or Worse than Conservative Care – How many studies of which type showed that the surgery was the same as or worse than conservative care?
- Evidence Supporting Use – In summary, what level of evidence exists that shows that the surgery is effective? The choices are none, weak, or good.
The Reader’s Digest
Only one of the top 10 most common surgeries had adequate evidence to support that it worked better than conservative care or a placebo. Four surgeries had weak evidence, meaning not adequate to meet any reasonable evidence-based standard. The other 5 surgeries had no evidence that they were effective. Only 2 of the 8 surgeries had a study comparing the procedure to a placebo, a key piece of evidence that’s required. Hence, in the end, 9 in ten of these common procedures had poor evidence support.
This Is Pitiful
There really isn’t any other way to describe this state of affairs other than pitiful. We have a VERY RICH surgical specialty that rakes in more than a Trillion dollars each decade with striking year-over-year increases in utilization. Yet, of the top 10 most common elective procedures, only ONE has adequate evidence of efficacy.
What’s even more nuts is that many in this same specialty often give those using orthobiologics a hard time because they claim that there isn’t enough evidence to support those injections. That’s of course just orthopedic surgery gaslighting as we have several dozen RCTs that show that PRP works to treat knee OA.
This Is NOT a Zero-Sum Game
If these surgeries had no morbidity and they didn’t work or we didn’t know if they worked, that would be one thing. However, we know that they cause significant harm. How much?
- ACL Reconstruction – 38% complication rate [includes graft failure] (4) with 100,000+ procedures annually=38,000 people injured (5) or in need of a second surgery
- Meniscal Repair – 18% complication rate (6) with 13,400+ procedures each year (7)=2,400 people injured
- Partial Menisectomy – 0.3% complication rate (8) with 500,000+ performed annually (9)=15,000 injured
- Rotator Cuff Repair – 10.6% complication rate (10) with 500,000 annual procedures (11)=53,000 injured
- Shoulder Decompression Surgery – 3% complication rate (12) with 30,000 procedures annually (13)=9,000 injured
- Decompression for Lumbar Stenosis – 20% complication rate [including reoperation for failure] (14) with 500,000 procedures annually (15)=100,000 people injured or in need of a second surgery
- Lumbar Fusion for DDD – 23% complication rate (16) with 325,000 procedures annually (17)=74,750 injured
- Hip Arthroplasty (Replacement) – 7% complication rate (18) with 450,000 procedures annually (19)=31,500 injured
- Knee Arthroplasty (Replacement) – 14% complication rate (20) with 754,000 procedures (21)=105,500 injured
That’s a grand total of several hundred thousand people injured per year. Let that sink in. We injure hundreds of thousands with procedures paid for by insurance companies that have no convincing evidence that they are effective.
The upshot? We have a 100+ billion a year medical subspeciality with some of the worst evidence base in medicine. Despite this, insurers pay for these procedures. Is this nuts or what?
______________________________________
References:
(1) Lohmander LS, Roos EM. The evidence base for orthopaedics and sports medicine. BMJ. 2015 Jan 2;350:g7835. doi: 10.1136/bmj.g7835. PMID: 25555826.
(2) Orthopedic Design and Technology. U.S. Healthcare Spending in Orthopedics. https://www.odtmag.com/issues/2019-05-24/view_columns/us-healthcare-spending-in-orthopedics/ Accessed 7/21/21
(3) Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. BMJ. 2021 Jul 7;374:n1511. doi: 10.1136/bmj.n1511. PMID: 34233885.
(4) Rousseau R, Labruyere C, Kajetanek C, Deschamps O, Makridis KG, Djian P. Complications After Anterior Cruciate Ligament Reconstruction and Their Relation to the Type of Graft: A Prospective Study of 958 Cases. Am J Sports Med. 2019 Sep;47(11):2543-2549. doi: 10.1177/0363546519867913. Epub 2019 Aug 12. PMID: 31403824.
(5) Csintalan RP, Inacio MC, Funahashi TT. Incidence rate of anterior cruciate ligament reconstructions. Perm J. 2008;12(3):17-21. doi:10.7812/tpp/07-140
(6) Austin KS, Sherman OH. Complications of arthroscopic meniscal repair. Am J Sports Med. 1993 Nov-Dec;21(6):864-8; discussion 868-9. doi: 10.1177/036354659302100619. PMID: 8291641.
(7) Kawata M, Sasabuchi Y, Taketomi S, et al. Annual trends in arthroscopic meniscus surgery: Analysis of a national database in Japan. PLoS One. 2018;13(4):e0194854. Published 2018 Apr 3. doi:10.1371/journal.pone.0194854
(8) Abram SGF, Judge A, Beard DJ, Price AJ. Adverse outcomes after arthroscopic partial meniscectomy: a study of 700 000 procedures in the national Hospital Episode Statistics database for England. Lancet. 2018 Nov 17;392(10160):2194-2202. doi: 10.1016/S0140-6736(18)31771-9. Epub 2018 Sep 24. PMID: 30262336; PMCID: PMC6238020.
(9) Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Kalske J, Nurmi H, Kumm J, Sillanpää N, Kiekara T, Turkiewicz A, Toivonen P, Englund M, Taimela S, Järvinen TLN; FIDELITY (Finnish Degenerative Meniscus Lesion Study) Investigators. Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med. 2020 Nov;54(22):1332-1339. doi: 10.1136/bjsports-2020-102813. Epub 2020 Aug 27. PMID: 32855201; PMCID: PMC7606577.
(10) Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007 Feb;23(2):124-8. doi: 10.1016/j.arthro.2006.09.001. PMID: 17276218.
(11) iData Research. Over 460,000 Rotator Cuff Surgeries per Year Reported in the United States by iData Research. https://idataresearch.com/over-460000-rotator-cuff-surgeries-per-year-reported-in-the-united-states-by-idata-research/ Accessed 7/21/21
(12) Karjalainen TV, Jain NB, Page CM, Lähdeoja TA, Johnston RV, Salamh P, Kavaja L, Ardern CL, Agarwal A, Vandvik PO, Buchbinder R. Subacromial decompression surgery for rotator cuff disease. Cochrane Database Syst Rev. 2019 Jan 17;1(1):CD005619. doi: 10.1002/14651858.CD005619.pub3. PMID: 30707445; PMCID: PMC6357907.
(13) Jones T, Carr AJ, Beard D, et al. Longitudinal study of use and cost of subacromial decompression surgery: the need for effective evaluation of surgical procedures to prevent overtreatment and wasted resources. BMJ Open. 2019;9(8):e030229. Published 2019 Aug 28. doi:10.1136/bmjopen-2019-030229
(14) Bydon M, Macki M, Abt NB, et al. Clinical and surgical outcomes after lumbar laminectomy: An analysis of 500 patients. Surg Neurol Int. 2015;6(Suppl 4):S190-S193. Published 2015 May 7. doi:10.4103/2152-7806.156578
(15) HCUP. Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb171-Operating-Room-Procedure-Trends.jsp Accessed 7/21/21
(16) Reis RC, de Oliveira MF, Rotta JM, Botelho RV. Risk of complications in spine surgery: a prospective study. Open Orthop J. 2015;9:20-25. Published 2015 Jan 31. doi:10.2174/1874325001509010020
(17) iData Research. How Many Spinal Fusions are Performed Each Year in the United States? https://idataresearch.com/how-many-instrumented-spinal-fusions-are-performed-each-year-in-the-united-states/ Accessed 7/21/21
(18) Aggarwal VK, Elbuluk A, Dundon J, Herrero C, Hernandez C, Vigdorchik JM, Schwarzkopf R, Iorio R, Long WJ. Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Joint J. 2019 Jun;101-B(6):646-651. doi: 10.1302/0301-620X.101B6.BJJ-2018-1474.R1. PMID: 31154834.
(19) AAOS. Total Hip Replacement. https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/#:~:text=Since%20the%20early%201960s%2C%20improvements,year%20in%20the%20United%20States. Accessed 7/21/21
(20) Heo SM, Harris I, Naylor J, Lewin AM. Complications to 6 months following total hip or knee arthroplasty: observations from an Australian clinical outcomes registry. BMC Musculoskelet Disord. 2020 Sep 10;21(1):602. doi: 10.1186/s12891-020-03612-8. PMID: 32912197; PMCID: PMC7488141.
(21) AAOS. Total Knee Replacement. https://orthoinfo.aaos.org/en/treatment/total-knee-replacement Accessed 7/21/21
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.