The Nerves at the Back of Your Head and Headaches
Most people don’t realize that there are nerves at the back of their neck and head that can cause headaches. So what’s up with that? How does this become an issue? How can you fix it?
Headaches from Your Neck
Most people out there still use the term “migraine” to refer to a headache. Oftentimes this obscures the cause in the neck, as a migraine is supposed to refer to a vascular headache in the brain. In fact. most people don’t know that their neck can cause headaches (cervicogenic headaches). Some however figure it out on their own because they can feel their headaches radiating up from the neck.
The Patient Pinball
One of the most common things I see happen in patients with cervicogenic headaches is that they invariably get treated for migraines, as that’s what neurologists, who generally underdiagnose cervicogenic headaches, are used to treating. Those medications either don’t help at all or only help minimally. Or the patient finds them effective but ultimately realizes that they don’t want to be on medications for the rest of their lives and begins seeking out other treatments. That’s when the patient begins to feel like a pinball in a specialist pinball machine, as they are shuffled from one specialist to another, each time getting a slightly different opinion about what’s wrong or what to do about it.
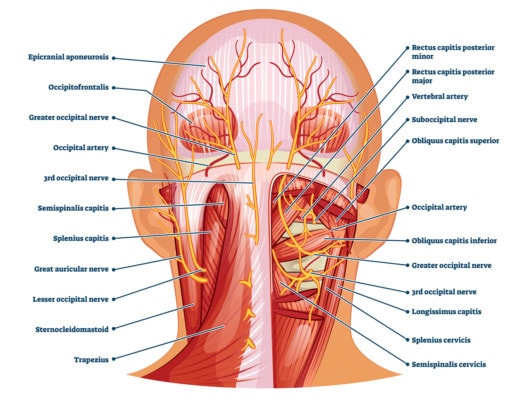
VectorMine/Shutterstock
Causes of Cervicogenic Headache
So if lots of headaches come from the neck, what are the common causes:
- Irritated nerves at the back of the head
- Irritated upper spinal nerves
- Damaged upper neck facet joints
- Upper neck ligament instability or malposition
This morning I’ll focus on nerves at the back of the head.
The Nerve Roadmap
Here’s a wiring diagram of the nerves that live back there:
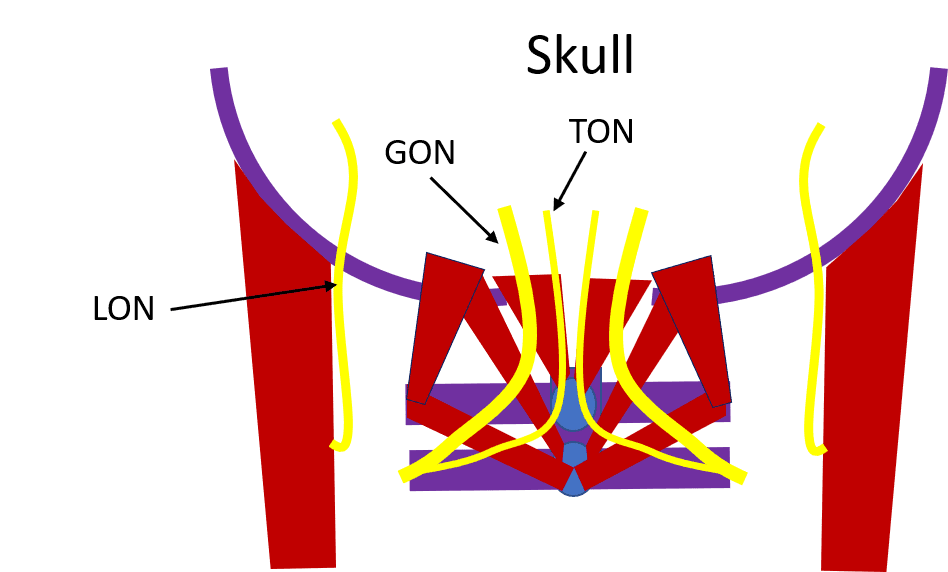
Above you see the two upper neck vertebrae, C1 and C2 in purple and the skull in that same color. In red are the deep muscles that control your head on your neck. In yellow, you see the following nerves:
- GON – Greater occipital nerve – This along with the TON originate from the C2 spinal nerve. The GON comes exits alongside the upper trapezius (not shown as that muscle is more superficial than the deep ones illustrated above).
- TON – Third occipital nerve – This pierces through the upper trapezius and comes out closer to the middle of the skull.
- LON – Lesser occipital nerve – This nerve exits the back of the sternocleidomastoid muscle and then it ascends and lives in a grove behind where that muscle attaches to the skull.
What all of these nerves have in common is that they cause headaches. In addition, the reason I’ve shown them above this way is that they all lie superficial to the deep cervical muscles (rectus capitis and obliques). Meaning anything that causes these upper neck muscles to go into spasm can piss off these nerves. In the same way, they all go through or exit near major more superficial neck muscles like the upper trapezius and SCM, so anything that causes these big muscles to spasm can also irritate the occipital nerves and thus cause headaches. When this happens, it’s called “occipital neuralgia”.
Occipital Neuralgia Treatment
So how do you treat these nerves causing headaches? For starters, conservative care like physical therapy, acupuncture, and chiropractic. If that doesn’t work, the most common treatments are:
- Steroid shots – These are usually blind in the office and injected where the upper trapezius and SCM meet the skull. The goal is to temporarily reduce the inflammation and hope that the original cause is no longer there.
- Botox – The idea here is to weaken the spasming muscles for a few months, giving the nerves a break.
One issue with these therapies is that both are generally temporary and destructive. Steroids destroy local cells and botox negatively impacts where the nerve talks to the muscle (neuromuscular junction). Are there other options?
Fix the Cause
Common causes of irritated nerves include:
- Upper neck instability or malpostion
- Facet joint damage
- Loss of the normal neck curve
- Irritated spinal nerves
Specific upper cervical chiropractic (NUCCA or AO) can often help. This is generally not the chiropractor down the street.
Treating instability requires injecting ligaments to tighten them down to reduce the extra movement. Helping damaged facets can be accomplished with x-ray guided injections into those joints with PRP or stem cells. Helping a lost neck curve can usually be done with specialized chiropractic techniques (CBP) or ligament injections. Sore spinal nerves can be treated by x-ray guided epidural injections.
Use Regenerative and Not Destructive Techniques-The Regenerative Occiciptal Car Wash
First, why not inject something that can help nerves repair themselves? Platelet based therapies have that potential (1-4). Second, it would make sense that the highest impact injection point would be the one shown above, injecting just superficial to these deep muscles would bathe all of these nerves at the same time. I call this the Regenerative Occipital Car Wash. To do this, you need to perform these injections using precise ultrasound guidance.
The upshot? There are lots of nerves at the back of your head and when they get irritated, you’ll get a mean headache. Understanding that this can cause your headache is the first step in getting rid of them!
_________________________________________
References:
- Platelet-derived growth factors (PDGFs) stimulate neurotrophic factors to be released, which promote the regeneration of peripheral nerve. Glia. 2009 Jul;57(9):947-61
- Insulin-like Growth Factor-1 (IGF-1) directly binds to IGF-1 receptors to stimulate the first step in fatty acid synthesis for re-myelination. Glia. 1997 Mar;19(3):247-58
- Vascular endothelial factor (VEGF) induces angiogenesis, which is a critical step that precedes axon regeneration in animal models. Exp Neurol. 2001 Dec;172(2):398-406.
- In both animal models and case reports that the application of PRP can significantly improve peripheral nerve axon regeneration with gaps varying from 3 – 12 cm. Prog Neurobiol. 2014 May;116:1-12 and Neurosurgery. 2011 Dec;69(6):E1321-6.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.