What Is Cervical Medullary Syndrome?
What happens when the neck bones impinge on the upper spinal cord and brain stem? This is called Cervical Medullary Syndrome. Let’s explore what this is and why it happens. Let’s dig in.
The Background Anatomy
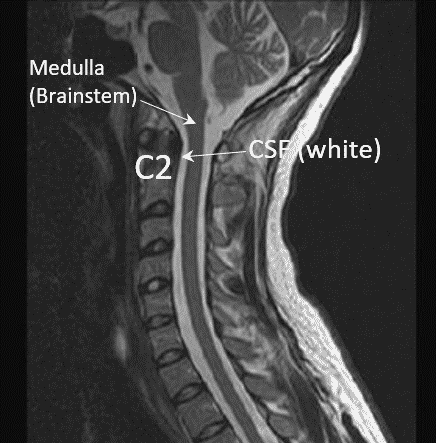
The normal upper neck anatomy is unique in that nature has built in quite a bit of space around the upper spinal cord and brainstem (Medulla). The image above is of this area and note that at around C2 there is white (this is CSF or cerebrospinal fluid) in front of the Medulla (brainstem). This acts as a buffer between this “Dens” part of the C2 vertebra and the upper spinal cord/brain stem.
What Is Cervical Medullary Syndrome?
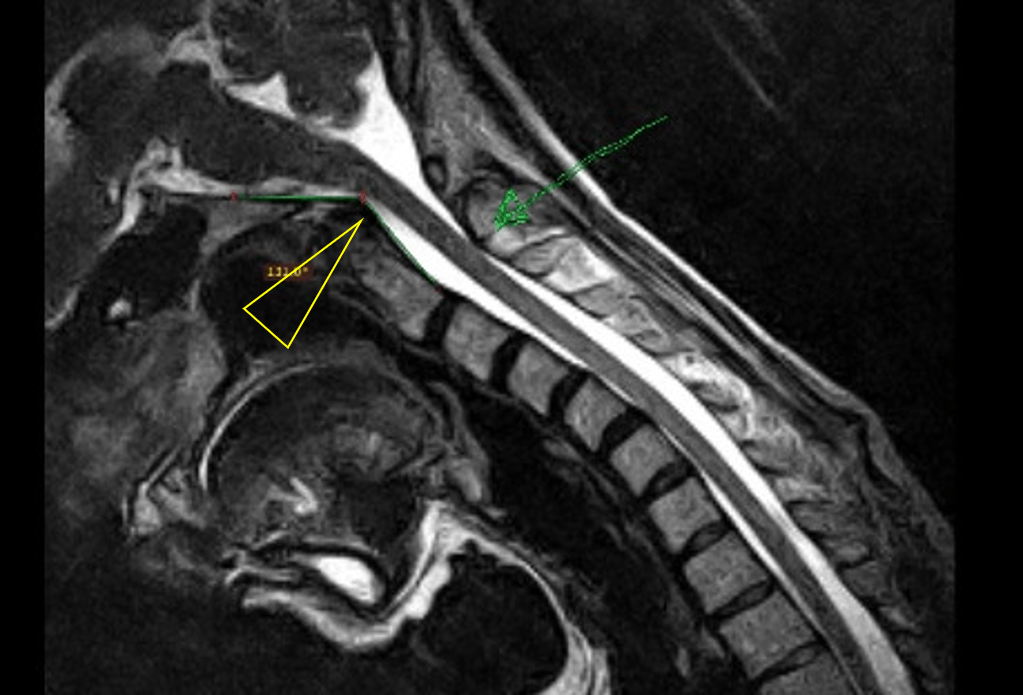
What if the Dens part of C2 (as shown above) moved too far back when the patient flexed? In the image above, note that when this patient is in flexion, the arrow points to the C2 hitting up against the Medulla. Note that at this arrow there is less white (CSF) to the left of the Medulla or less “buffer”. This is related to another concept called Craniocervical Instability or CCI.
How Are Cervical Medullary Syndrome and CCI Related?
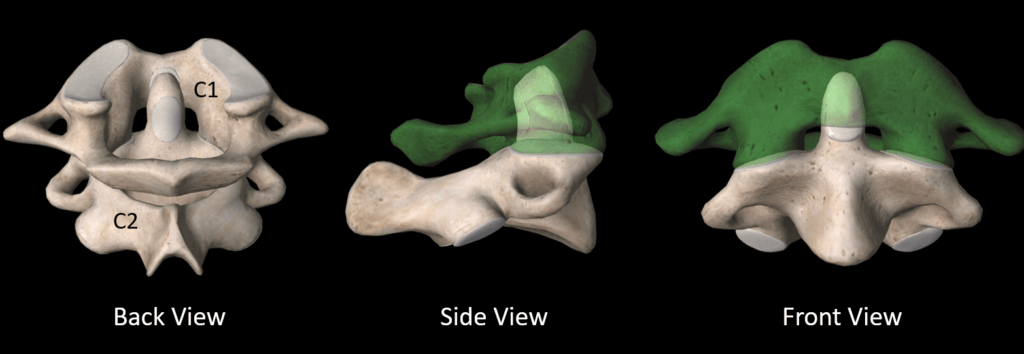
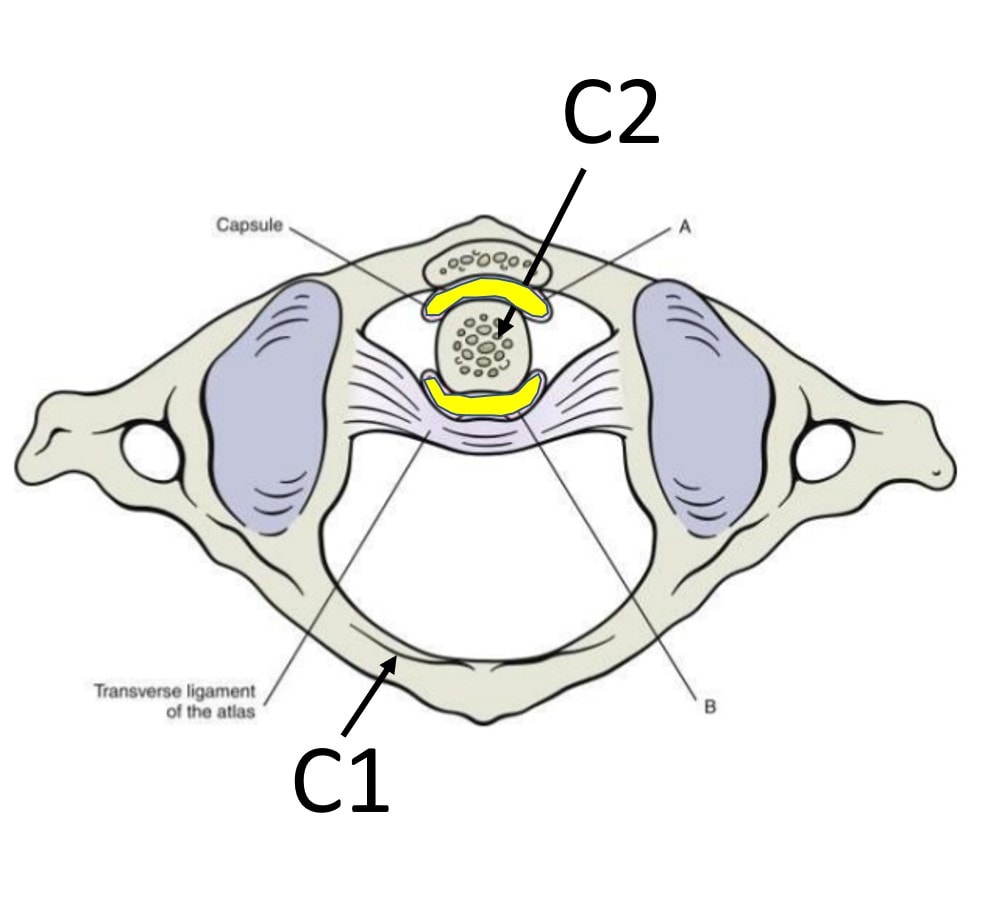
The C2 bone fits inside the C1 bone as shown above. This enables the C2 bone to turn around C1, which is the spot where half of your neck rotation originates.
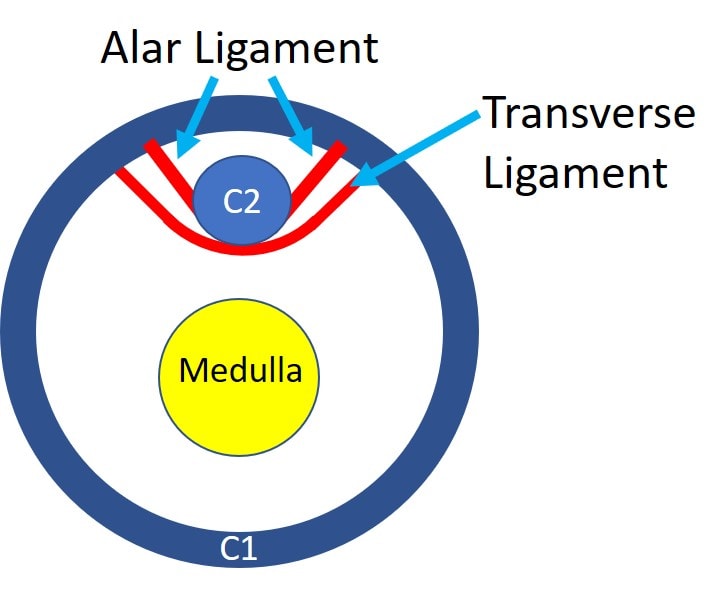
There are strong ligaments that hold the C2 bone (Axis) to the C1 bone (Atlas). In the image above, which is now taken from the top, the Dens (C2) is held in place by the Transverse and Alar ligaments. Note that this prevents the Dens from hitting into the Medulla.
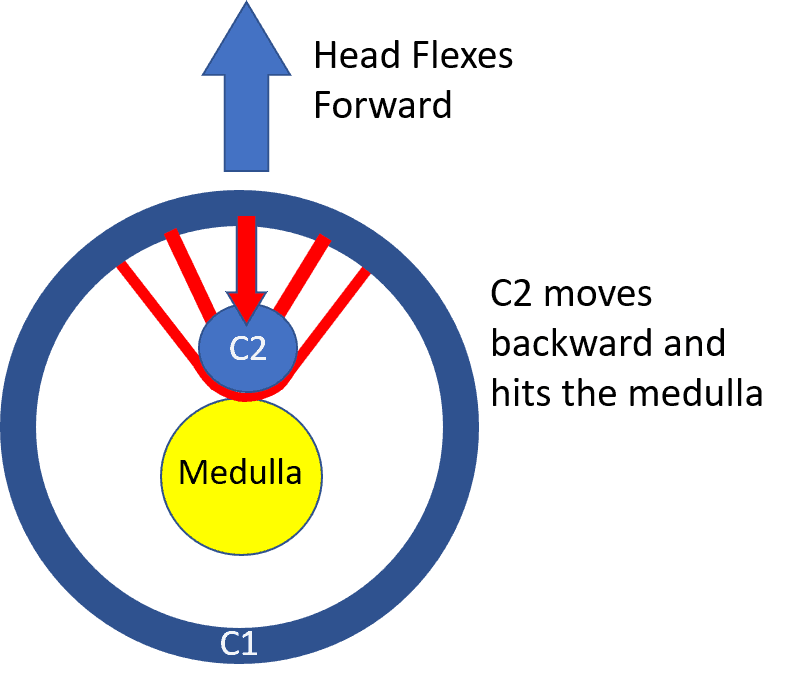
Now let’s look at what happens when the Alar and Transverse ligaments are loose. In the image above the loose ligaments allow the Dens (C2) to move backward and hit the Medulla when the head and neck flexes forward.
Cervical Medullary Syndrome and EDS
While many cases of Cervical Medullary Syndrome are due to head and neck trauma damaging the ligaments, some are due to connective tissue problems like Ehlers Danlos Syndrome (EDS). Patients with this problem have super stretchy ligaments and this can include the Alar and Transverse ligaments, which can lead to a Cervical Medullary Syndrome.
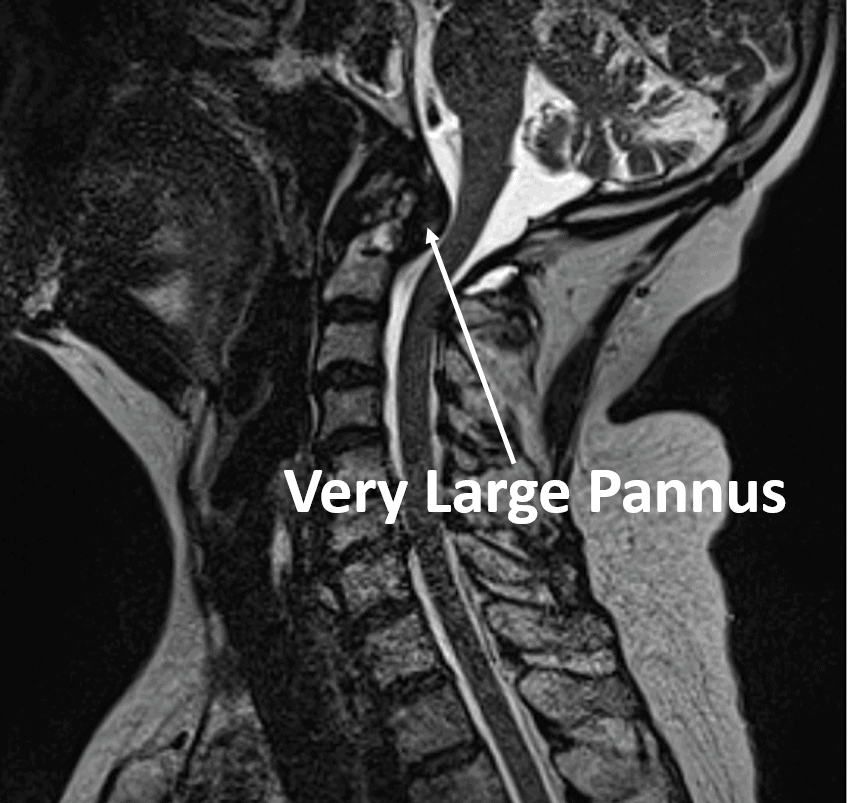
Structural Issues and an Odontoid Pannus
On the front and back of the Dens of C2, there is a bursa (shown in yellow). Those lubricating sacs can become swollen and even scarred down, which produces what’s called a Pannus. This can add to the pressure on the Medulla and the Cervical Medullary Syndrome as shown below:
What Are the Symptoms of Cervical Medullary Syndrome?
What are the symptoms? Given that Craniocervical Instability has overlapping symptoms with a Cervical Medullary Syndrome, separating out the two can be difficult. However, common symptoms include:
- Headache
- Numbness/weakness in the arms, hands, legs, feet
- Dizziness/imbalance
- Brain fog
- And many others
How Is Cervical Medullary Syndrome Treated?
The first-line treatment is often physical therapy or specific upper cervical chiropractic. In my experience, the latter is usually more successful in some patients, as it more directly addresses the malposition of C1 on C2, which tend to rotate on each other when there are loose or damaged ligaments. When this doesn’t help, a surgical fusion of the upper neck bones is usually recommended. This involves using screws and sometimes plates or rods to make sure the upper neck bones don’t move. However, this is a high-risk procedure that can’t be undone. In addition, it can also cause adjacent segment disease (ASD), which means that the spinal levels above and below can get worn out and damaged, requiring the need for more fusions.
An alternative is trying to heal or tighten the ligaments through very specific x-ray guided injections. While prolotherapy (ligament tightening injections) on the ligaments in the back of the neck can be tried, the ligaments discussed here that cause the Cervical Medullary Syndrome can’t be reached or treated using that method. The PICL procedure does treat these ligaments directly:
Want to learn more? Read my book below:
The upshot? Cervical Medullary Syndrome is a real problem that can be caused by Craniocervical Instability. It can usually be treated by helping the instability and non-surgical options are available.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.