Why You Might Want to Avoid Rotator Cuff Surgery

Credit: Shutterstock
Earlier this month I presented the almost final data from our randomized controlled trial on shoulder rotator cuff tears at a large national conference on orthobiologics. The research will soon be submitted for publication, but you’ll get the first look at our data here. Let’s dig in.
The Problem with Shoulder Rotator Cuff Tears and Surgery
The muscles that move and stabilize your shoulder are called the rotator cuff. The tendons and/or muscles can be torn through wear and tear as we age or through trauma. When that happens, if it’s a mild tear, physical therapy is often prescribed. However, for bigger tears or those smaller ones that won’t get better with PT, surgical repair is often used. However, rotator cuff surgery has the following problems:
- Large meta-analyses show that we have no convincing evidence that rotator cuff repair beats physical therapy (3,8,9)
- Shoulder range of motion and glenohumeral biomechanics are not restored to normal levels after rotator cuff repair (4)
- Only half of throwing athletes return to their sport after this surgery (1)
- Contrary to what one may think, the size of the rotator cuff tear doesn’t dictate the pain that patients experience, instead, the inflammatory markers in the joint are directly correlated with pain (IL-8) (2). Meaning that the whole idea behind why rotator cuff tears hurt may be upside down.
- Surgical rotator cuff repair doesn’t reverse or improve fatty atrophy of the muscles (5). This is a big problem, as this atrophy is believed to cause long-term shoulder problems.
- Despite the surgery, the retear rate is 21% (6)
- 1/3 of repaired rotator cuffs in patients over age 60 fail by 1 year with an 8% complication rate (7)
Hence, it’s time for something else. To that end, we have been using a procedure we call Percutaneous Shoulder Rotator Cuff Repair (Perc-RCR) for many years.
Perc-RCR
Almost two decades ago, we began to use imaging guidance to inject autologous mesenchymal stem cells into rotator cuff tears. In fact, this was one of our first before and after images posted online back in 2010:
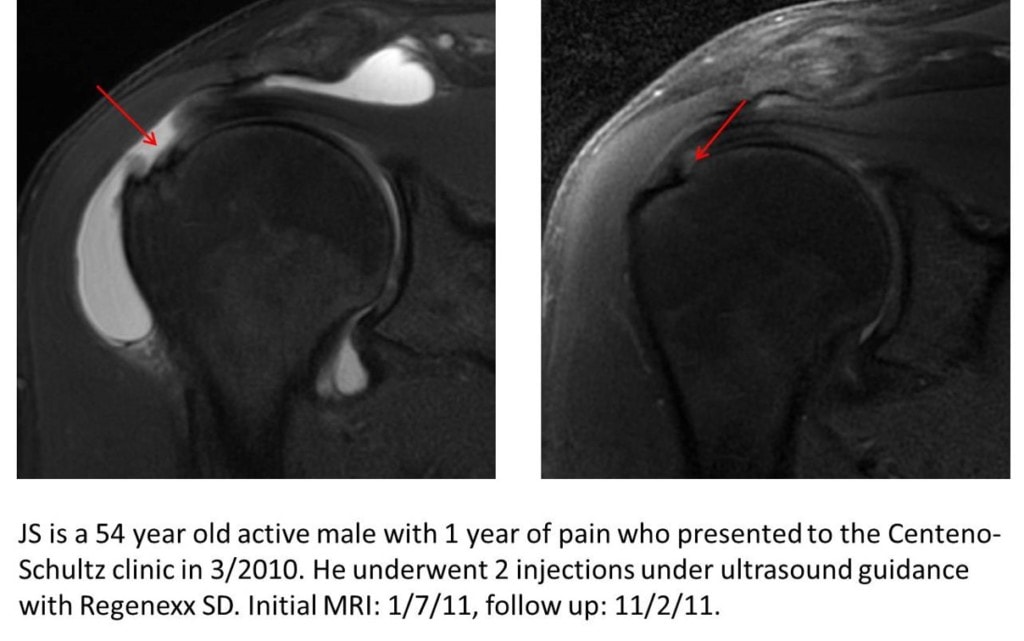
That treatment eventually morphed to using bone marrow concentrate which contains the patient’s own stem cells and eventually we published a large case series in 2015 (10).
However, this field needs more evidence. Over the years, this treatment proved itself in our experience to be highly successful in helping patients avoid surgery, so we eventually began a randomized controlled trial.
Our Perc-RCR RCT
The RCT or Randomized Controlled Trial is the bedrock of modern evidence-based medicine. In this type of study, you randomize patients either to receive the therapy you’re studying or another treatment and then observe the results between the groups. In this case, our focus was on randomizing patients to either Perc-RCR or physical therapy as that replicates what’s published in the orthopedic surgery literature. Meaning when the surgeons perform one of the few RCTs available for surgical rotator cuff repair they usually compare it to physical therapy.
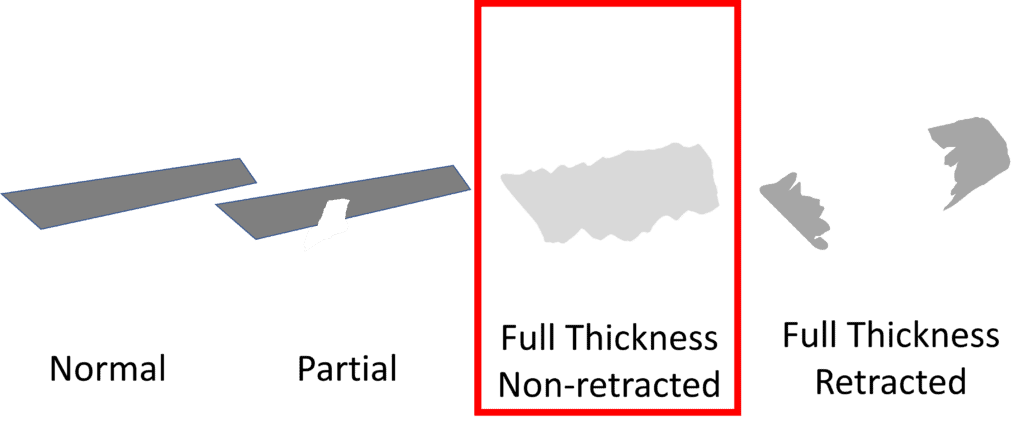
The Perc-RCR procedure is focused on patients with complete non-retracted rotator cuff tears:
The actual procedure involves taking a bone marrow aspirate and then concentrating two stem cell fractions in the sample to create a high-dose bone marrow concentrate (BMC). That’s then precisely injected using ultrasound guidance into the tears.
We published a mid-term analysis of this 50-patient RCT back in January of this year (11). This demonstrated excellent results compared to physical therapy. That’s a big deal because as I showed above, surgical rotator cuff repair was unable to beat the results of physical therapy in three different trials. However, that was only half of the data, so what does the whole dataset tell us?
The Final Perc-RCR RCT Data
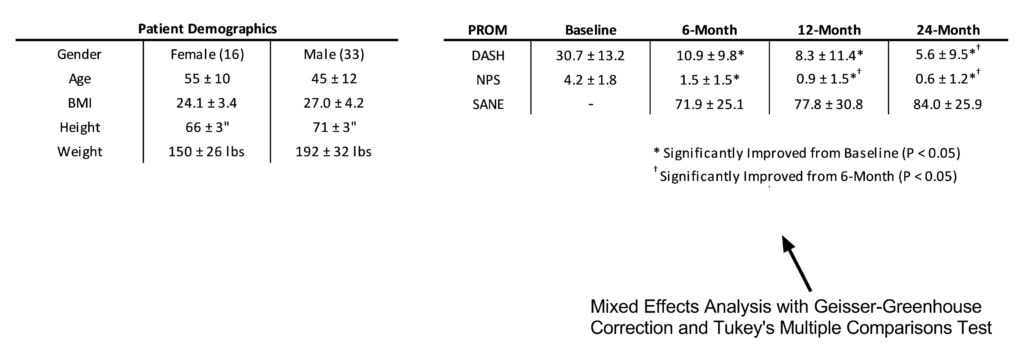
I presented the almost final dataset at the recent TOBI conference in Florida. Here’s what that looks like:
This is the demographic data showing that we ended up with 49 patients with a 2-1 male/female ratio who were in the range from normal weight to slightly heavy.
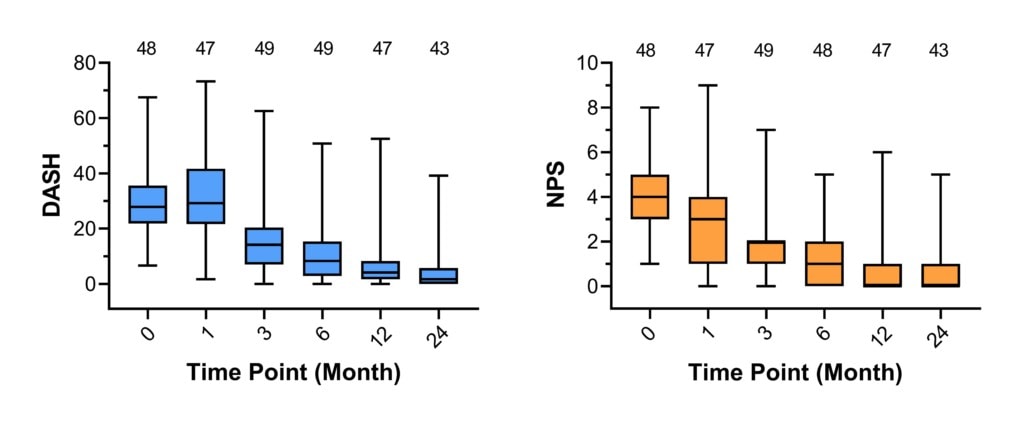
Above you see the results of the DASH questionnaire (shoulder function) and the pain scale (0-10 numeric pain or NPS) for the Perc-RCR group. Both excellent results with marked improved function and reduced pain by 3-6 months post-procedure.
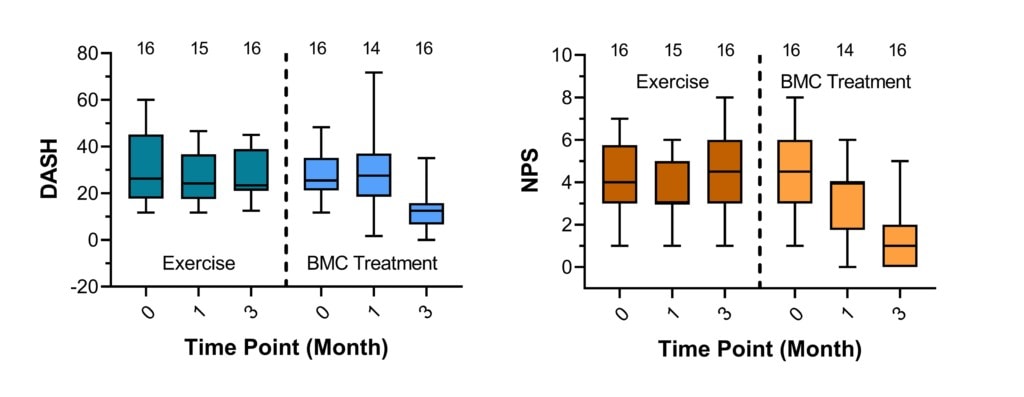
Above is the comparison between the exercise and Perc-RCR groups. On the left is the DASH and the right NPS. The exercise group had no significant improvements in both DASH or NPS while the Perc-RCR group had excellent responses. This data is only out to three months because patients who had been assigned to the exercise group were permitted to switch over to the Perc-RCR group at 3 months (cross-over RCT design).
Again, it’s important to emphasize that a trial against physical therapy is the surgical standard. For example, if we look at all shoulder rotator cuff tear RCTs, almost all that compare against conservative care use PT as the comparator arm. In addition, all surgical treatments have lost that battle to date.
The upshot? Our rotator cuff tear RCT data looks solid. We have just one more 24-month data point to get on one patient which shouldn’t change these results. Then, we’ll submit this for publication, which should take 3-6 months.
________________________________________
(1) Klouche S, Lefevre N, Herman S, Gerometta A, Bohu Y. Return to Sport After Rotator Cuff Tear Repair: A Systematic Review and Meta-analysis. Am J Sports Med. 2016 Jul;44(7):1877-87. doi: 10.1177/0363546515598995. Epub 2015 Aug 27. PMID: 26316611.
(2) Okamura K, Kobayashi T, Yamamoto A, Shitara H, Osawa T, Ichinose T, Takagishi K. Shoulder pain and intra-articular interleukin-8 levels in patients with rotator cuff tears. Int J Rheum Dis. 2017 Feb;20(2):177-181. doi: 10.1111/1756-185X.12581. Epub 2015 Apr 30. PMID: 25930944.
(3) Seida JC, LeBlanc C, Schouten JR, Mousavi SS, Hartling L, Vandermeer B, Tjosvold L, Sheps DM. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010 Aug 17;153(4):246-55. doi: 10.7326/0003-4819-153-4-201008170-00263. Epub 2010 Jul 5. PMID: 20621893.
(4) Bey MJ, Peltz CD, Ciarelli K, Kline SK, Divine GW, van Holsbeeck M, Muh S, Kolowich PA, Lock TR, Moutzouros V. In vivo shoulder function after surgical repair of a torn rotator cuff: glenohumeral joint mechanics, shoulder strength, clinical outcomes, and their interaction. Am J Sports Med. 2011 Oct;39(10):2117-29. doi: 10.1177/0363546511412164. Epub 2011 Jul 7. PMID: 21737834; PMCID: PMC4601100.
(5) Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007 Aug;89(8):1770-6. doi: 10.2106/JBJS.F.00749. PMID: 17671017.
(6) Longo, U.G., Carnevale, A., Piergentili, I. et al. Retear rates after rotator cuff surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord 22, 749 (2021). https://doi.org/10.1186/s12891-021-04634-6
(7) Dezaly C, Sirveaux F, Philippe R, Wein-Remy F, Sedaghatian J, Roche O, Molé D. Arthroscopic treatment of rotator cuff tear in the over-60s: repair is preferable to isolated acromioplasty-tenotomy in the short term. Orthop Traumatol Surg Res. 2011 Oct;97(6 Suppl):S125-30. doi: 10.1016/j.otsr.2011.06.006. Epub 2011 Jul 27. PMID: 21798838.
(8) Khatri C, Ahmed I, Parsons H, Smith NA, Lawrence TM, Modi CS, Drew SJ, Bhabra G, Parsons NR, Underwood M, Metcalfe AJ. The Natural History of Full-Thickness Rotator Cuff Tears in Randomized Controlled Trials: A Systematic Review and Meta-analysis. Am J Sports Med. 2019 Jun;47(7):1734-1743. doi: 10.1177/0363546518780694. Epub 2018 Jul 2. PMID: 29963905.
(9) Nazari G, MacDermid JC, Bryant D, Athwal GS. The effectiveness of surgical vs conservative interventions on pain and function in patients with shoulder impingement syndrome. A systematic review and meta-analysis. PLoS One. 2019;14(5):e0216961. Published 2019 May 29. doi:10.1371/journal.pone.0216961
(10) Centeno CJ, Al-Sayegh H, Bashir J, Goodyear S, Freeman MD. A prospective multi-site registry study of a specific protocol of autologous bone marrow concentrate for the treatment of shoulder rotator cuff tears and osteoarthritis. J Pain Res. 2015 Jun 5;8:269-76. doi: 10.2147/JPR.S80872. PMID: 26089699; PMCID: PMC4463777.
(11) Centeno C, Fausel Z, Stemper I, Azuike U, Dodson E. A Randomized Controlled Trial of the Treatment of Rotator Cuff Tears with Bone Marrow Concentrate and Platelet Products Compared to Exercise Therapy: A Midterm Analysis. Stem Cells Int. 2020 Jan 30;2020:5962354. doi: 10.1155/2020/5962354. PMID: 32399045; PMCID: PMC7204132.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.