Is Injecting a Knee Blind Associated with Worse Health Outcomes?
Credit: Shutterstock
Like a headline from the Onion, I recently read an email describing a big orthopedic surgery conference where a panel was sourced on whether or not you needed ultrasound guidance to inject a knee. While the result of this panel was a LOL moment for many of my colleagues, none of us really knew the negative health implications of blind knee injections. So let’s dig into this concept and dive into some “newish” research.
X-ray Vision
If you’re an old guy like me, you may remember the ads that used to live in every comic book or Mad magazine about x-ray vision glasses. While I never ordered them, like most young boys, I wanted to get them. A cursory read of the ad showed how using these glasses could allow you to see bones in hands or even through clothes. You could basically, for a buck, gain one of Superman’s powers!
These, of course, turned out to be fiction, and at some point, the term “optical illusion” became a part of these ads. However, there’s a modern version of x-ray glasses out there, it’s called your average orthopedic surgery practice. So today we’ll review the research that shows that the Superman x-ray vision of these modern surgical demigods is also an optical illusion.
Before I launch into this blog, let me congratulate orthopedic surgeons like Don Buford who have been beating this drum for a long-time. Don has run ultrasound education for orthopedic surgeons every year for as long as I can remember. As a result of his work and others like him, there are more orthopedic surgery practices using ultrasound than ever before. However, as you’ll see, even that Herculean effort hasn’t yet resulted in the justified death of the blind knee injection in most orthopedic clinics.
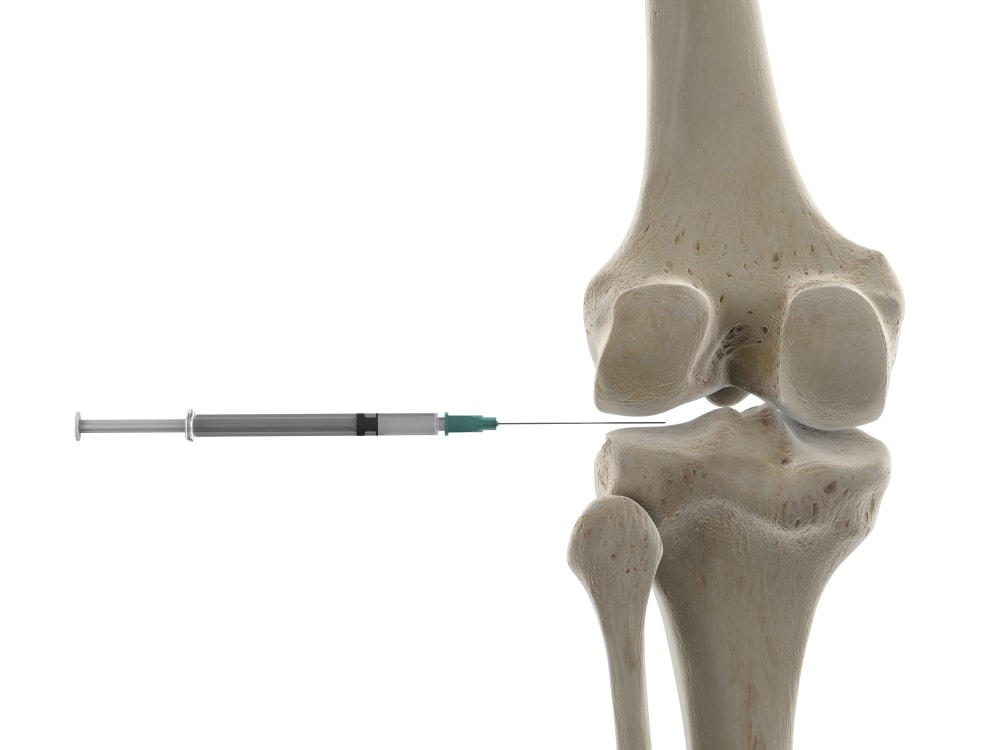
Blind Knee Injections
A blind injection means that the needle is inserted without any type of imaging guidance. Because knee joints have traditionally been injected blind, in most orthopedic surgery practices this still happens. Is this a good idea?
We’ve known for a while now that blind knee injections are a bad idea. For example, in a 2012 study, using ultrasound imaging to guide the needle and make sure it was in the joint increased the accuracy of injecting into the joint capsule from 84% to 96% (1). Why is that a big deal? Because things like hyaluronic acid won’t work well if injected into the soft tissues rather than inside the joint.
In fact, there are now so many studies on how the use of ultrasound imaging makes knee injections more accurate, that there’s an entire systematic review on the subject. This “study of studies” reviewed data from many other research papers (12 in this case). A systematic review is therefore considered the highest level of evidence. This one, published in June of this year concluded (2):
“This study showed that ultrasound-guided knee injections were more accurate across every anatomical needle injection site compared with blind injections. Injections made by a blind/anatomically guided method had inconsistent accuracy rates that seemed highly dependent on the portal of entry.”
Pretty definitive.
The Onion Orthopedic Conference Panel
Given that using ultrasound to make sure you’re inside a knee joint is a no brainer in 2021 and that courses for this skill are plentiful and ultrasound machines are cheap, I first thought someone was messing with me when I heard that a large orthopedic conference, just this year, had an entire panel on whether or not ultrasound was needed. Even more ridiculous, the orthopedic surgeons on the panel all agreed that they didn’t need ultrasound guidance. In opposition to that idea was the sole non-surgeon on the panel who brought up the above studies, but ultimately, that lone voice was a small contrarian whisper against a tidal wave of surgical bravado.
This has been my experience as well. When I ask my patients, who are from all over the US and world, whether their orthopedic surgeon or clinic used ultrasound imaging to inject their knee, I get a “no” answer about 3 in 4 times. Meaning, the average orthopedic surgeon, as evidenced by the panel and my decade-plus of informal polls, believes that he or she has x-ray eyes like Superman. No need for that girly-man ultrasound machine, I can feel some bone, jam the needle in, and I am always in the joint!
Are the X-ray Eyes of Orthopedic Surgeons Harming Patients?
Given that this issue of x-ray vision in orthopedic surgeons has been a running joke among the physicians who have routinely used ultrasound for many years, the big question has been what impact does this refusal to use modern technology have on health outcomes? For me, that was an unanswered question until a colleague sent me a 2019 paper that sought to answer it (3). This research reviewed the conversion rate of people getting hyaluronic acid injection (knee gel shots) to a knee replacement. Meaning the idea behind HA is that it will help lubricate the arthritic knee and reduce the bad chemicals in the joint and prolong the need for a surgical amputation and insertion of a prosthesis (total knee arthroplasty or knee replacement). The researchers wanted to see whether blind (or “landmark guided”) HA injections produced any more or fewer eventual invasive surgeries. What did they find? Over a decade, 46% of the patients who were injected blind needed a knee replacement versus only 33% of those who got their HA injections done with ultrasound.
This surgery-free survival graph is the money shot from that study:
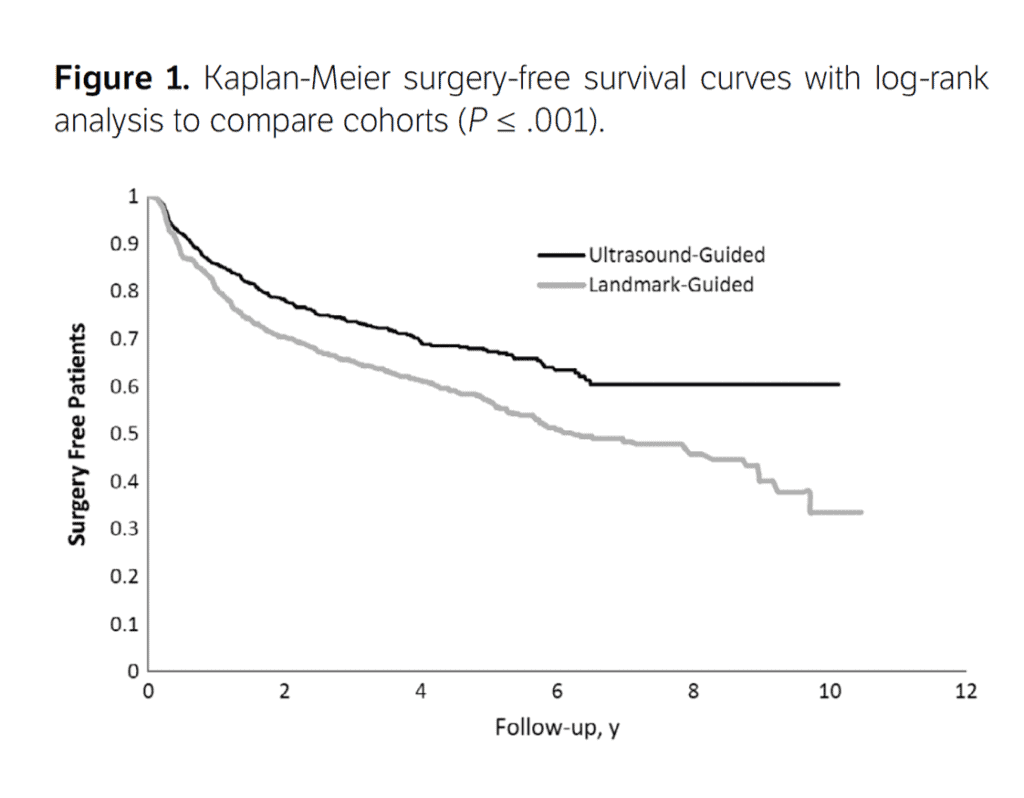
Credit: Lundstrom, et al (3)
Ouch! The black line is the percentage of surgery-free patients per year who had their knee injected with ultrasound. The grey line is the same data from the blind (“Landmark-Guided”) group. More patients remained surgery-free in the ultrasound group over time and this difference widened as the years went on.
The upshot? We know that injecting a joint blind is a bad idea. We also now know that it’s likely also associated with harm. Hence, if you walk into a physician’s office who wants to inject your knee blind, then politely ask for your chart and walk out. As a patient, there is simply no reason in 2021 to tolerate a blind or “landmark guided” injection.
_____________________________________________________
(1) Bum Park Y, Ah Choi W, Kim YK, Chul Lee S, Hae Lee J. Accuracy of blind versus ultrasound-guided suprapatellar bursal injection. J Clin Ultrasound. 2012 Jan;40(1):20-5. doi: 10.1002/jcu.20890. Epub 2011 Oct 28. PMID: 22033897.
(2) Fang WH, Chen XT, Vangsness CT Jr. Ultrasound-Guided Knee Injections Are More Accurate Than Blind Injections: A Systematic Review of Randomized Controlled Trials. Arthrosc Sports Med Rehabil. 2021;3(4):e1177-e1187. Published 2021 Jun 26. doi:10.1016/j.asmr.2021.01.028
(3) Lundstrom ZT, Sytsma TT, Greenlund LS. Rethinking Viscosupplementation: Ultrasound- Versus Landmark-Guided Injection for Knee Osteoarthritis. J Ultrasound Med. 2020 Jan;39(1):113-117. doi: 10.1002/jum.15081. Epub 2019 Jun 25. PMID: 31237389.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.