Why You Can’t Inject a Torn Knee ACL with Ultrasound
When we first began injecting ACL tears with stem cells many years ago, we tried quite a few techniques. At first, it was a very difficult injection that wasn’t reliable. However, after some anatomy review and testing several methods, we finally settled on a procedure that produced reliable results and then began teaching that through a nonprofit course. This morning I’d like to review a case that shows why injecting an ACL with ultrasound only could cause problems.
Can We Inject the ACL?
Designua/Shutterstock
The anterior cruciate ligament, or ACL, is a ligament that stabilizes the knee in front-back and rotational directions. It can be torn in sports or trauma, and these days it’s often surgically removed when torn and replaced with a tendon graft. However, there are problems with ACL surgery, so the idea of keeping your existing ACL is attractive.
When I first tried to inject the ACL, it was after speaking at a prolotherapy conference. This most basic of regenerative-medicine injections involves using a solution that causes a brief inflammatory healing reaction. However, almost all prolotherapy at the time (and most of it still to this day), is performed blind without guidance. In the case of the ACL, this meant that the physician stuck a needle inside the joint and used outside landmarks to ensure that he or she was injecting into the ligament. After I was back in my practice, I decided to use the blind technique with guidance to determine how often the doctor was really injecting into the ligament. Regrettably, I wasn’t able to accurately inject into the ACL using this technique nor did I believe that many of my prolotherapy colleagues were really injecting it either.
Over the next few months, I set out to document that I was injecting the ACL. However, while I would get lucky in some patients and have solid documentation of an ACL injection, the procedure was hit or miss. One of our doctors suggested trying it with ultrasound as he had seen that procedure at a recent course. The good news was that we could visualize the front part of the ligament (insertion), but it was all but invisible at around one-third to one-half way up or more. About that time, we were experimenting with a mini-arthroscope, and we were able to inject the ligament with that device (which I think is the first ACL injected with stem cells using arthroscopy). The issue here was that it seemed silly to put a patient through an arthroscopy just to inject a ligament (basically using a sledgehammer to put in a finishing nail).
Around that same time, I dug into the literature about ACL anatomy and made a breakthrough using fluoroscopy (real-time X-ray). I figured out how to reliably inject the bottom (insertion) and top (origin). Once this happened, we didn’t need the arthroscope, as an injection is always less invasive than a surgery. In addition, we began to see that one of the problems with the ultrasound method was that the torn ACL often leaked out the back of the synovial covering of the ligament about two-thirds of the way up. So by injecting these torn ligaments with ultrasound, while it looked like the doctor was injecting the whole ligament, the upper part wasn’t getting any cells. Finally, we also began to observe that there was a correlation between how well we were able to cover the ligament with cells and the extent of ligament regeneration we saw on MRI. After that, a smart fellow named Dr. Bashir also helped to make the procedure even better.
Images That Explain Why Ultrasound ACL Injections Are Suboptimal
Since we invented this ACL stem-cell-injection technique, we get patients from all over the world. In this case, a professional athlete had an ACL tear and went to a respected surgical orthopedic clinic. The tear was read out as “partial,” and surgery wasn’t recommended, so a nonsurgical provider injected bone marrow concentrate into the ACL using ultrasound. The patient was then braced and went back to working out hard. I was told by the athlete’s trainer that all providers thought that the ACL was healing one month later, but when I looked at both films (before and after the injection), the ACL had, in fact, substantially worsened. There was now a new retracted part in the area where an ACL ultrasound image couldn’t reach, the tibial offset measurements that we use to determine candidacy had substantially worsened, and there was new bone swelling. Why had this happened when this technique is usually very reliable in the right patients? Meaning that if performed properly, we usually see the opposite on MRI (i.e., evidence of ACL regeneration, a stable or the same offset measurement, and a reduction in bone swelling). While it’s possible that a poor result would have occurred regardless of injection technique, given the candidacy data we’ve amassed, that seemed unlikely (i.e., he was an excellent candidate coming into the procedure).
I think the image below may help explain what happened. Note that the image on the left below is an ACL ultrasound, and the image on 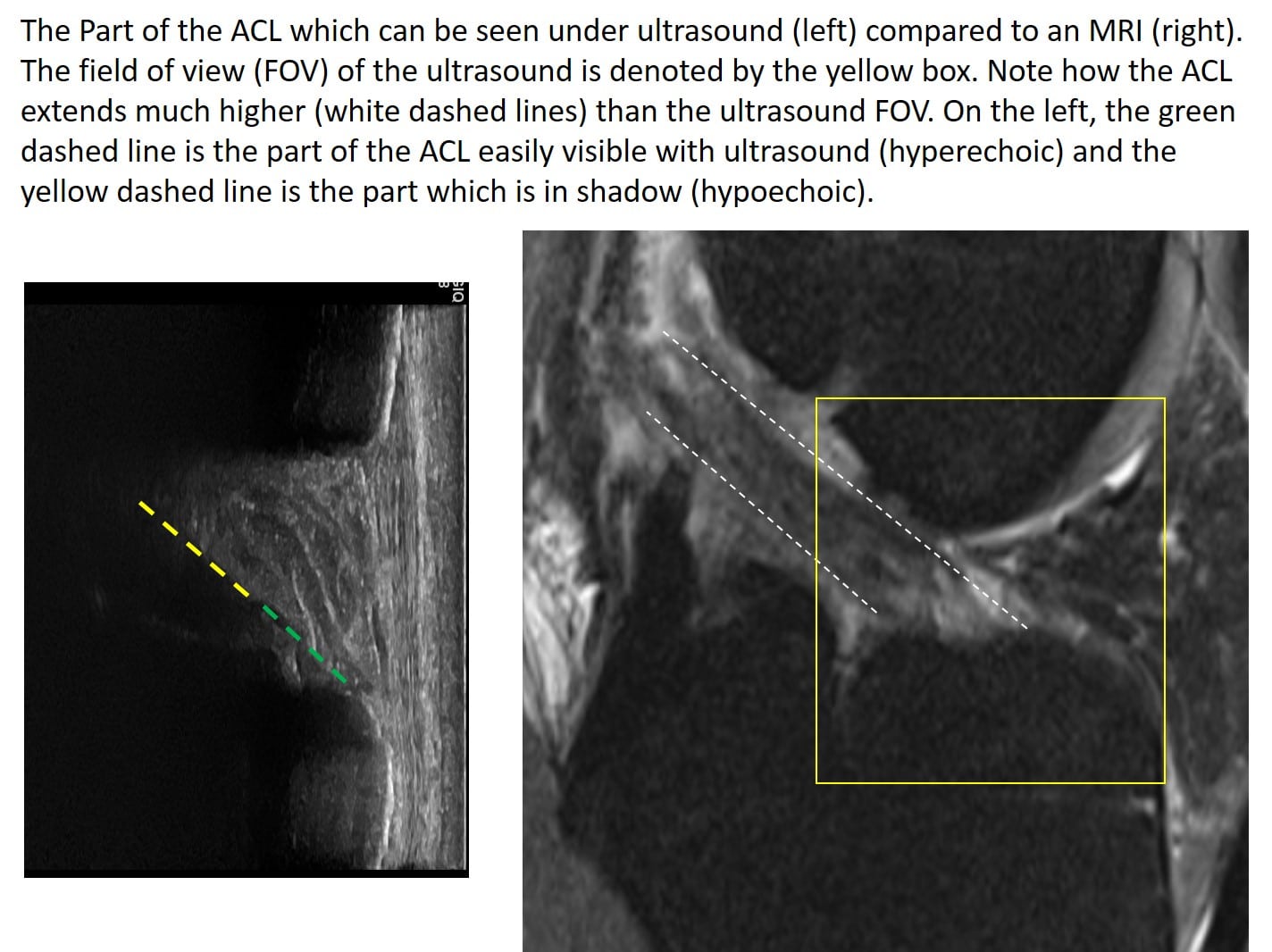
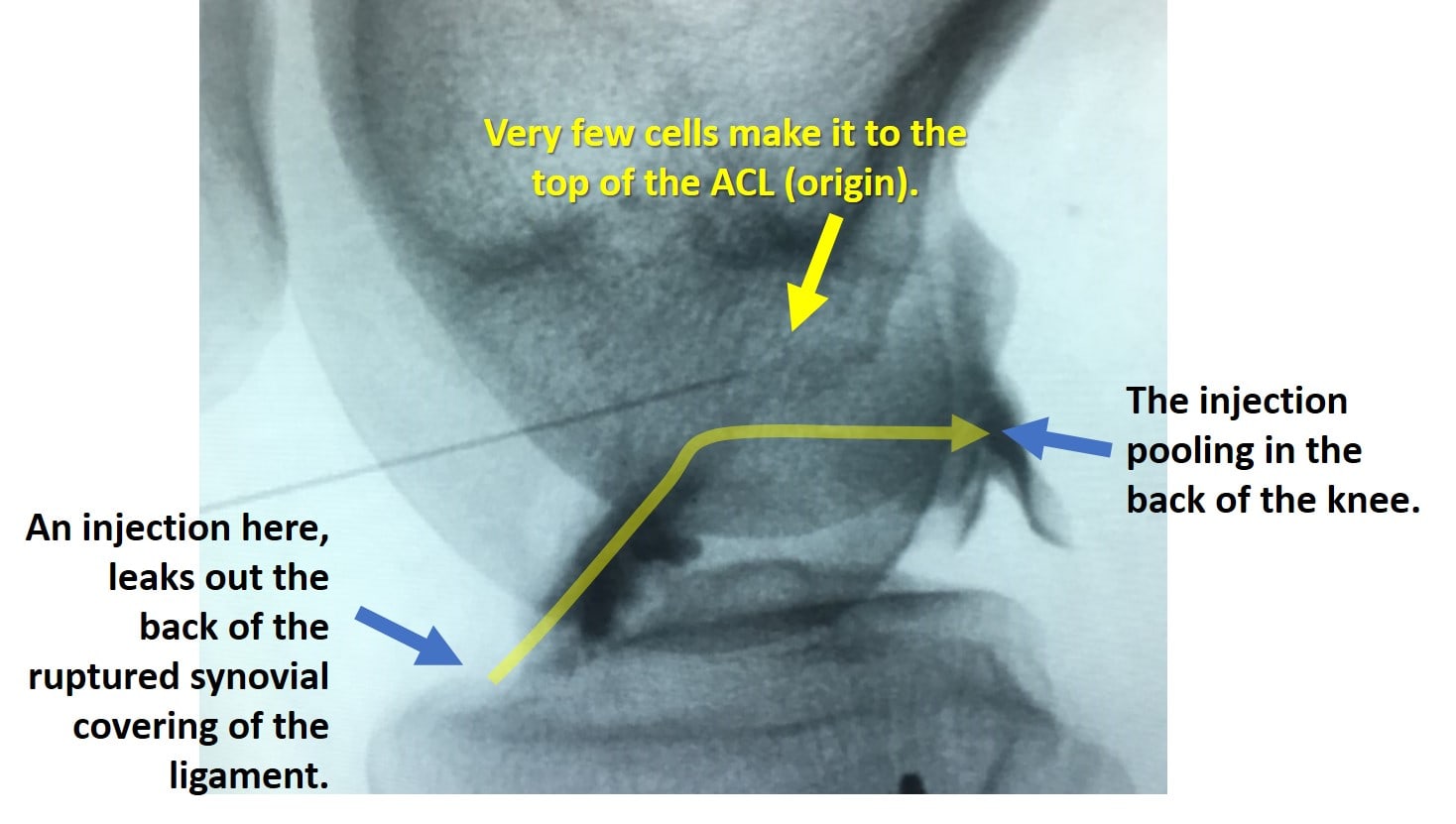
Now consider this image of a properly injected ACL tear where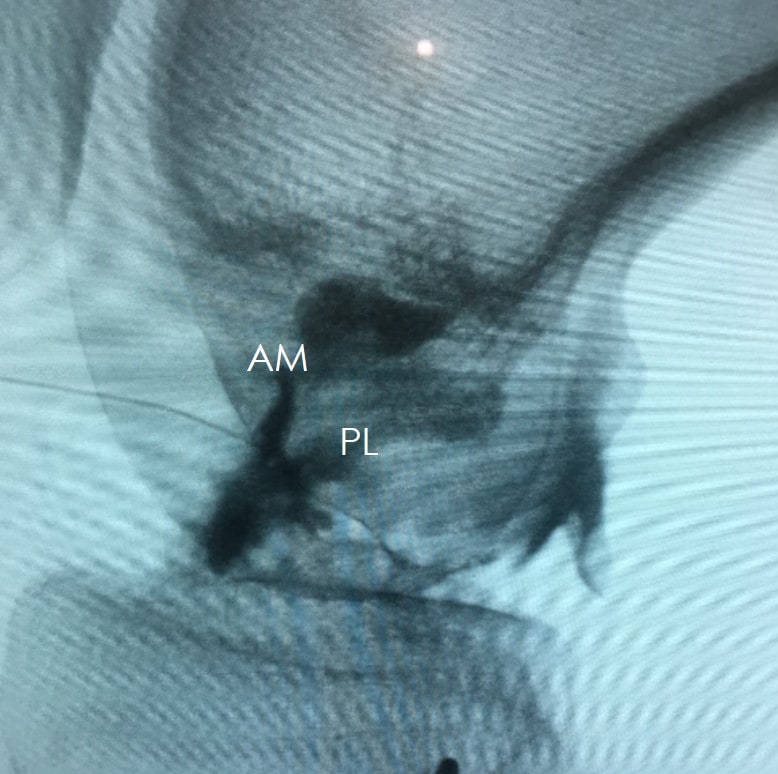
The upshot? While you can likely inject an intact ligament with ultrasound and have it work reasonably well, a torn ACL is another matter. While fluoroscopy is more expensive to own and operate, it’s needed to perform a proper injection of the torn ACL with stem cells. So please, please, please don’t inject a torn ACL with ultrasound, doubly so if the patient depends on that knee to make a living!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.