New Research: Low Back Fusion Surgeries Are Ineffective
Low back fusion in medicine is one of those procedures that some doctors have come to hate. Why? While a handful of patients do fine, many become lifelong patients with new problems caused by the procedure. So I have to say that I’m happy that the research has finally caught up to what we see in the clinic. Let’s dive into this topic and that new research.
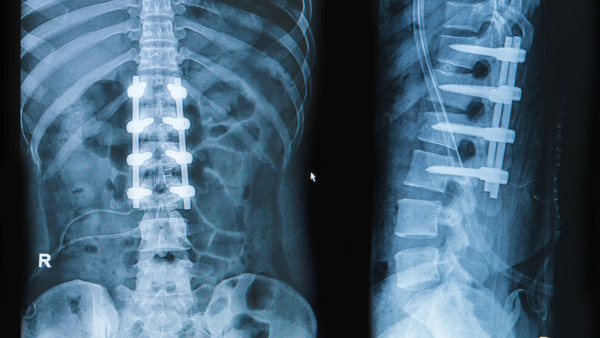
Praisaeng/Shutterstock
A Doctor’s View of This Surgery
I’ll never forget the first time I began encountering patients who had low back fusion surgery. Long before I knew how to help these patients without surgery, many would get a low back fusion and then return to me because they were still in pain. I would ask these patients about why they came back, and they would almost all say that they were still in pain or that their pain had worsened or that one pain had gotten better but a new pain had begun. At first, you dismiss these patients as having psychological problems. However, when it’s most of the patients you send for the procedure, you begin to realize that it’s not the patient, it’s the surgery.
What always blew me away was what the surgeons told the patients. When the patient came back after the surgery still in pain, the surgeon would take an X-ray, which would show that the fusion was healing, and politely say that their job was done because the surgery looked great! Disturbingly, I saw that surgeons were routinely divorcing themselves from the outcome of the procedure. If we were talking about a hangnail removal, that might have been OK, but this procedure is one of the more invasive orthopedic surgeries out there. Really?
The invasiveness of this procedure was what was brought home one day when a local family doctor had a fusion and ended up blind. Yes, you read that right—he was blinded by the surgery. Turns out he lost too much blood during the procedure and was never the same. In fact, as far as I know, he never again practiced medicine.
What Is Involved in a Spinal Fusion?
A spinal fusion is pushed as a way to relieve chronic back pain by permanently disabling movement in the affected area of the spine. Most commonly, these are elective spinal fusions performed for degenerative spine conditions causing chronic pain, such as degenerative disc disease or arthritis. A fusion involves first removing the disc between the affected vertebrae and then using screws, bone graft, or other hardware to connect the bones. The bones, over time, will then fuse together to form one solid bone. Fusions can involve two, three, or more vertebrae, depending on the damage.
Besides disabling movement in a structure that is designed for flexibility, there are many other reasons spinal fusions are a bad idea, including multifidus muscle damage, continued chronic pain, and adjacent segment disease (see my video later in this post).
Is Spinal Fusion Really All That Common?
Every year since 2008, the Agency for Healthcare Research and Quality (AHRQ) has listed spinal fusion within the top 10 of the most common inpatient surgeries performed in the U.S. The last statistics available are from 2015, where spinal fusion climbed to the number 5 spot, just behind C-sections, circumcisions, knee replacement, and hip replacement. Compare this to 1998, for example, when spinal fusions had barely cracked the top 40 most common inpatient surgeries, and you get a sense of the explosion in the use of the procedure.
So, yes, spinal fusion is very common today, and the vast majority of these, as mentioned above, are elective spinal fusions for degenerative back conditions, such as degenerative disc disease. With fusion being such a major, invasive, and fast-growing surgery, it must mean there’s an abundance of good, strong evidence that elective spinal fusion is effective. Nope…let’s review the latest research.
Overwhelming Evidence Against Spinal Fusion
For the new study, researchers collected and analyzed data from 33 randomized controlled trials (RCTs) and other studies comparing spinal fusion to nonoperative solutions for low back pain and degenerative conditions. In addition, they reviewed the quality and bias level of each study.
What did they find? Of the 33 reviews, they found only two RCTs with “clinically meaningful benefits” of fusion; however, one of these had a high risk of bias, and both included discography, which may more accurately diagnose back pain but comes with its own high risk of side effects. Their review of the other studies found elective spinal fusion to be no more effective than nonoperative solutions, such as physical therapy, and so on. In addition, they highlighted one study that also found high complication rates following spinal fusion for back pain, which included infections, major bleeding, and nerve injuries. Their final conclusion? The overwhelming evidence simply doesn’t support spinal fusion (and its high costs and risks) for back pain and degenerative conditions over nonoperative solutions.
My Review of Spinal Fusion Studies
If you are regular reader of this blog, you know I often share my own reviews of these spinal fusion studies. Let’s take a look at a small handful of these:
- Back pain, quality of life, and disability were found to be no better with spinal fusion than without.
- Spinal fusion for stenosis, according to another study, improved pain and function no better than physical therapy alone.
- Yet another study found that physical therapy was just as effective as spinal fusion.
- Think you’ll toss the opioids after spinal fusion? Not so fast. The study I covered here found 91% were still taking these dangerous narcotics.
- One study found the more spine levels you have fused, the greater the chance you’ll need even more fusions. Why? Adjacent segment disease (ASD). Learn more about ASD by watching my brief video below:
The upshot? I’m really glad the research has caught up with the day-to-day clinical reality of what we see. Thankfully, we can now help the vast majority of these patients who would otherwise get spinal fusions. However, this surgery isn’t going away tomorrow, as we still see a high percentage of patients walking in with new fusions. So please do your homework and avoid this invasive procedure!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.