SI Joint Fusion: Does This Work?
The Rise of Sacroiliac (SI) Joint Fusion Surgery
I have been following with interest the rise of SI Joint fusion surgery. This has exploded over the last five years. So what does SI Joint fusion look like? Can SI Joint dysfunction be cured? How successful is SI Joint fusion? Are there better and less invasive options you haven’t tried? Let’s dig in.
SI Joint Fusion Surgery
This surgery addresses SI Joint injury and SI Joint instability using screws that are placed through the joint from the Sacrum to the Illium. Like all fusion surgeries, the goal is to make the joint unable to move. This is called SI Joint fusion. There is both open and minimally invasive SI Joint Fusion. In open SI Joint fusion a 7 or 8 inch incision is used and the muscles and tissues are “opened” surgically to access the area. In minimally invasive Si Joint fusion surgery, two small incisions are made and the instruments are guided with x-rays.
One system (iFuse SI Joint Fusion implant shown here) uses specialized titanium implants that are placed across the joint. This is billed as “minimally invasive” because it uses a device to place these implants. However, while less invasive than open surgery, the device is large enough to cause tissue destruction as it has to be placed through the gluteal muscles to access the SI joint.
The SI Joint: What Is It and What Does It Do?
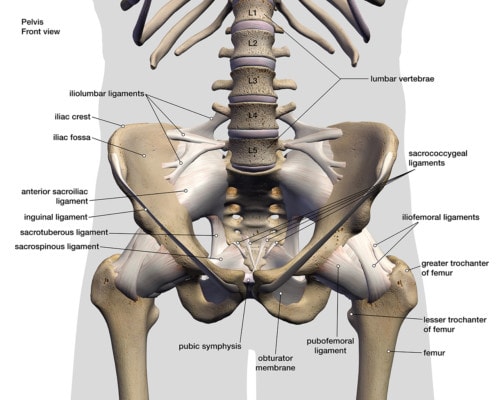
The SI Joint lives between the tailbone and the back of the hip. It’s a shock-absorbing joint that transfers forces from the leg into the pelvis and spine. It’s supported by tough ligaments that give and allow small amounts of motion (7). Because of it’s more shock-absorbing role, it doesn’t have a large range of motion like the hip or knee joints.
The Sacroiliac Joint Injury
Hank Grebe/Shutterstock
The SI Joint can be injured with trauma from a things like a fall on the buttocks or a car accident, or surprising to some from childbirth, or simply because of the patient’s lax ligaments. The biggest issue that we observe is SI Joint instability, which happens when the ligaments get stretched. This means that the SI Joint moves too much which can cause the cartilage in the joint to be injured. It can also get “stuck” in the wrong position, or misaligned.
Take a look at the complex of ligaments shown here. What if the healing agents from your own body could get those ligaments that make up the SI joint functioning normally rather than just bolting the joint together? Let’s look at that a bit later…
What Does It Feel Like When Your SI Joint Is Out of Place?
The SI Joint connects the illium to the tailbone and that connection often results in symptoms felt in either, or both, areas. Symptoms such as low back pain (below L5), pelvis or buttock pain, hip or groin pain, and disturbed sleep due to pain are common with SI Joint injuries. When the ligaments are injured and the joint moves around too much, this is called “SI Joint Instability”.
If the SI Joint is unstable, then it can get into positions of excessive motion where it’s out of its normal range. Patients often describe this as “stuck”. That problem can impact walking or even make the leg feel suddenly weak. Other possibilities include pain in the back of the hip near the dimples of venus (PSIS) or even strange sensations down into the thigh or the back of the leg. Many patients say that these sensations can be helped by manipulation of the joint. However, if the joint is unstable, the problem will return.
The Research: How Successful Is SI Joint Fusion Surgery?
The earliest studies published on this surgical procedure were one and two-year follow-ups of patients that were previously enrolled in a randomized trial (RCT) with a 6-month follow-up [8,9,10]. The two-year study seems to report good results. However, how good is debatable. For example, before the procedure, 76% of the patients needed to take opioids and two years after the procedure, 55% were still taking narcotics. Given the significant side effects caused by long-term opioid use, reducing that use by a mere 21% with more than half of the patients still addicted to narcotics is not impressive.
The Results: What They Say About The Surgery
The above research reports that only about 5% of the patients had significant side effects, but is that correct? Another research paper which was not paid for by the company making the implants disputes that claim [11]. This study was a compilation of insurance company data on complications from more than four hundred SI joint fusion surgeries. The complication rate in this research study was more than 300% higher than the complication rate reported in the company-sponsored study (4.7% vs. 16.4%) [11]! A common complication of this research was new spinal problems. I’ll review that further below.
In yet another company-funded and written study, the SI-Bone fusion device was used in 103 patients with many patients reporting good results at four years (2). However, you always need to read the fine print. I noticed this statement: “In total, 114 adverse events were reported between years 3 and 4; however, none were rated as probably or definitely related to the study devices or index surgical procedure.” Why did this capture my attention? Because this statement worries me: “Many events indicated underlying degenerative disease associated with age and osteoarthritis (eg, hip, knee, shoulder, neck, and lumbar spine osteoarthritic degeneration).” The next joints up from the SI joint are the lumbar spine and the next joint down is the hip. Hence any degenerative arthritis that occurs in either location would be due to the SI fusion until proven otherwise. Why? Let’s dig in.
“Say Hello to My Little Friend”: Adjacent Segment Disease
ASD or Adjacent Segment Disease is a known entity in all types of spinal fusion. Since fusion stops one area from moving and since that area was built to move, that force must go someplace. Where does it go? Usually above and below the fusion. Watch my video below for more information:
So what happens? The places above and below the fusion get arthritic and degenerative, often meaning more surgery. Does this happen right away? No, it takes years to destroy the joints above and below. As an example, if you fuse the low back, we know that those forces clearly overload the SI joint (1). Hence, the insurance study above that demonstrates new low back problems due to SI joint fusion makes sense. This hasn’t stopped the company that makes the hardware from trying to influence this discussion with its own study purporting to show that fusing the SI joint minimally impacts the lumbar spine (3). However, this study clearly showed the opposite, as there were increases in the movement at the adjoining low back levels that were due to the SI joint fusion. In addition, because the SI joint has very little motion to begin with, this study is asking the wrong questions.
What is the Recovery Time for SI Joint Fusion Surgery?
The recovery here requires that the bones that make up the SI joint fuse together. Hence, you’re looking at 6 months before that happens to a significant and safe degree. Expect to be in pain for several weeks to months, depending on how you respond to surgeries. I would not expect to get back to all of your activities for 6 months to a year.
How Much Does SI Joint Fusion Cost?
According to the Healthcare Bluebook, the cost of a spinal fusion is between $28,463 and $85,956 (4). However, in one study, the more specific cost of SI joint fusion was lower and quoted at $21,696 (5). However, these are medicare prices which are often lower than out of pocket costs. That quote also doesn’t include hospital or surgical center fees, so expect to pay for these as well. This study quoted $10,224 for those costs. The costs could be less if the procedure is performed in a physician’s office.
The above price also didn’t include pre-operative workup for a sacroiliac joint diagnostic injection, which when performed in an office can run as little as $650. However, many of these procedures are performed in a surgery center where costs can run $1-2,000 in total as the surgery center fee is often at least that much. The above study on SI joint fusion also quoted 7-11 sessions of physical therapy after the procedure at a cost of approximately an additional $1,000.
Hence, the average total cost for an SI joint fusion is likely to be in the $34,000 range. That could go as low as $16,000, or even higher, if the patient has complications or needs to be hospitalized.
Is There a Better Treatment that’s Much Less Invasive?
The hardest thing for me to see with these surgeries is that I know that 90% of these patients could easily avoid this invasive SI joint fusion procedure by using their own body to heal these loose SI joint ligaments. What does that look like? For most, it’s getting an injection of their own platelet-rich plasma into the ligaments and joint (6). If that doesn’t work, then getting their own bone marrow stem cells injected usually takes care of the problem.
How do these procedures work? By promoting the weakened, stretched out, and loose ligaments to beef up and tighten down. This means ligaments that are now working to protect the joint and that still allow normal motion and none of the overload and adjacent segment disease that happens with SI joint fusion.
Both of those procedures are far less invasive than an SI joint fusion and far less costly. However, in my experience, very few patients who end up getting an irreversible SI joint fusion surgery get offered these newer options. Why? SI joint fusion is simply more profitable.
The upshot? Should you get an SI fusion? If this were me or a family member, I would say no for all of the reasons stated. While there may be a handful of patients out there that really need this surgery, those are just a small percentage of the patients who end up with the procedure. The vast majority could have these loose SI joint ligaments treated through a simple injection without invasive surgery.
_____________________________________
References:
(1) Asil K, Yaldiz C. Retrospective Assessment of Early Changes in the Sacroiliac Joint After Posterior Lumbar Fusion Surgery via Magnetic Resonance Imaging and Computed Tomography. World Neurosurg. 2018 Dec;120:e546-e550. doi: 10.1016/j.wneu.2018.08.127.
(2) Darr E, Cher D. Four-year outcomes after minimally invasive transiliac sacroiliac joint fusion with triangular titanium implants. Med Devices (Auckl). 2018;11:287–289. Published 2018 Aug 29. doi:10.2147/MDER.S179003
(3) Lindsey DP, Kiapour A, Yerby SA, Goel VK. Sacroiliac Joint Fusion Minimally Affects Adjacent Lumbar Segment Motion: A Finite Element Study. Int J Spine Surg. 2015;9:64. Published 2015 Nov 13. doi:10.14444/2064
(4) Healthcare Bluebook. Search on “Sacroiliac Joint Fusion”. Accessed 28 August 2019. https://www.healthcarebluebook.com/ui/proceduredetails/22
(5). Cher DJ, Frasco MA, Arnold RJ, Polly DW. Cost-effectiveness of minimally invasive sacroiliac joint fusion [published correction appears in Clinicoecon Outcomes Res. 2016;8:305]. Clinicoecon Outcomes Res. 2015;8:1–14. Published 2015 Dec 18. doi:10.2147/CEOR.S94266
(6) Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017 Jul;17(6):782-791. doi: 10.1111/papr.12526.
(7) Richard L. DonTigny, B., Dysfunction of the Sacroiliac Joint and Its Treatment. The Journal of Orthopaedic and Sports Physical Therapy, 1979. 1(1): p. 13. https://www.ncbi.nlm.nih.gov/pubmed/18810188
(8) Duhon BS, Cher DJ, Wine KD, Kovalsky DA, Lockstadt H; SIFI Study Group. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: A Prospective Study. Global Spine J. 2016;6(3):257–269. doi:10.1055/s-0035-1562912
(9) Duhon BS, Bitan F, Lockstadt H, et al. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: 2-Year Follow-Up from a Prospective Multicenter Trial. Int J Spine Surg. 2016;10:13. Published 2016 Apr 20. doi:10.14444/3013
(10) Whang P, Cher D, Polly D, et al. Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. Int J Spine Surg. 2015;9:6. Published 2015 Mar 5. doi:10.14444/2006
(11) Schoell, K., et al., Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J. 2016 Nov;16(11):1324-1332. doi: 10.1016/j.spinee.2016.06.016.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.