TFCC Surgery Issues and Jennifer’s Story
Our opposable thumbs are one of the things that have allowed our brains to get so big. To make that work, there’s a structure you may never have heard of called the TFCC which can become damaged and cause immense pain. When that happens TFCC surgery is often recommended. Is that a good idea? No, it’s usually not the right choice. I’ll illustrate that today with Jennifer’s story so let’s dig in.

Credit: Shutterstock
What Is a TFCC?
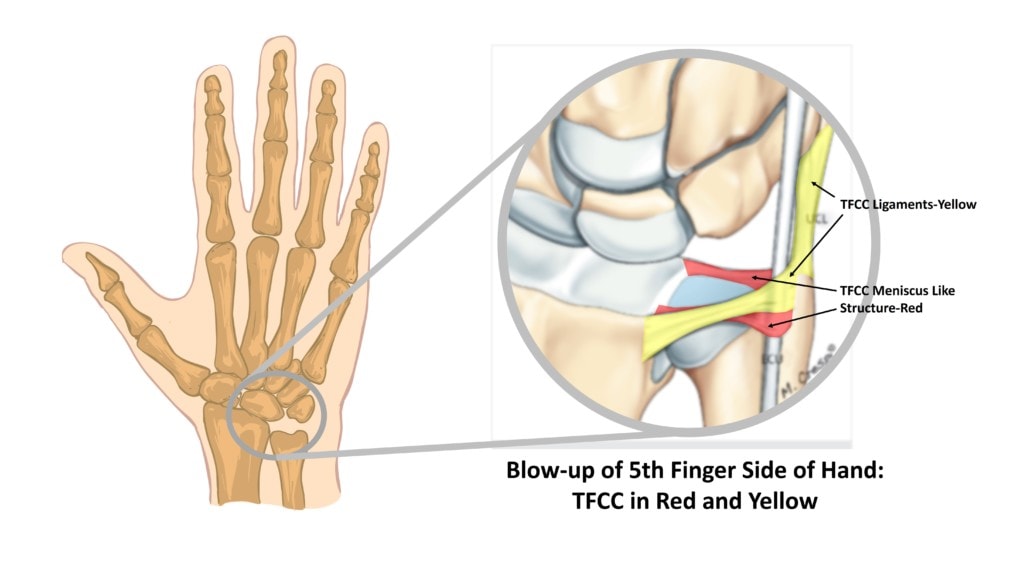
TFCC stands for Triangular Fibrocartilage Complex. This is a meniscus like disc and associated ligaments that live on the pinky finger side of the hand at the base of the wrist:
Credit Shutterstock and Mathoulin, Christophe Louis. “Chapter 7 Anatomy of the Triangular Fibrocartilage Complex: Current Concepts.” (2015). Mathoulin et al image with extensive illustration and editing.
The TFCC first holds this side of the Radius and Ulna wrist bones together. Second, it’s a shock absorber for forces coming to this side of the wrist. Third, without the TFCC, we would be relegated to animals without opposable thumbs.
How Does the TFCC Get Injured?
The most common cause of injury is a fall on an outstretched hand. I personally found this out the hard way several years back when I fell onto my hand/wrist after tripping. I had immense pain in that area and was barely able to hold objects for several weeks. Once the pain calmed down, I had our doctors perform precise injections into the injured disc and ligaments, and have had few issues since. Had I gone to a hand surgeon, I’m sure I would have ended up with TFCC surgery. So let’s see what going down that surgical path can look like by diving into TFCC surgery types and then Jennifer’s story.
TFCC Surgery Types
The main type of TFCC surgery is arthroscopic repair. Here, several small incisions are made and small scope is inserted. The goal is to sew together any small tears in the disc or ligaments. If that fails, revision surgeries or scar tissue removals usually ensue. In addition, at some point, the repair may be extended out to include the crossing tendons (i.e. ECU) or even a Carpal Tunnel Release. If all of that fails, either an ulnar shortening or a wrist fusion are often recommended. The shortening procedure removes a piece of the Ulna bone to attempt to remove pressure from this side of the wrist and the Fusion involves placing plates and screws to ensure that the wrist is unable to move.
Jennifer’s TFCC Story and Recovery
Jennifer is a 41-year-old woman who injured her TFCC. When the wrist didn’t heal, she had the following TFCC surgery procedures:
- 2014 TFCC repair
- 2017 TFCC repair
- 2018 carpal tunnel release / “scar tissue excision”
- 2018 carpal tunnel release revision
- 2019 ECU tendon/ TFCC repair
None of these surgeries helped and each surgery made things worse. Her hand surgeon then suggested ANOTHER TFCC surgery which was to be ulnar shortening. I’ve blogged in the past on that barbaric surgery.
At that point, she started looking at other options to avoid TFCC surgery and found Dr. Markle. She was treated with precise ultrasound and x-ray guided injections of her own Bone Marrow Concentrate into the TFCC ligaments, disc, distal ulnar bone, and tendons in a single-day procedure. Dr. Markle also carefully injected the growth factors derived from her platelets (platelet lysate) around the injured median nerve at the carpal tunnel in the wrist. To get a sense of what some these procedures look like, see my video on precise, image-guided hand/wrist procedures:
The result? At 6 months out, she’s reporting 90-100% improvement and close to full range of motion. All numbness and tingling are gone and her grip strength has returned to normal. She still has a little soreness, likely from the TFCC surgery caused arthritis in the wrist, but after five failed surgeries, she otherwise got her life back.
Betting at the Surgical Casino
One of the things I’ve noticed through the years is that patients can take on a Vegas mentality with surgeries. Like being at a blackjack table, when the first surgery fails (or the blackjack hand busts), they double down for a second surgery. When that fails they triple down on another and so on. Hence, after the damage caused by 5 TFCC surgery procedures, Jennifer is VERY lucky to finally get a winning hand due to precise Orthobiologic injections. After 5 failed bets, most patients wouldn’t be so lucky.
Why? Each procedure causes a small amount of damage to these structures. While the goal of surgery is to repair more than you damage, when the repair isn’t working, you end up with the cumulative damage done by multiple procedures.
I bring this up because if this is you and you’ve had one or two surgeries that haven’t worked and have made things worse, it’s much better to step away from the surgery betting table. I know that this can be hard to do, as each surgery and successive surgeon tells you they can fix your wrist, but the earlier you step back and look for non-surgical alternatives, the better.
The upshot? I’m so happy we could help Jennifer’s wrist and TFCC with precision image-guided Orthobiologics. I thankfully never went down that TFCC surgery road. Like me, if you or a loved one have a TFCC injury that hasn’t healed on its own, you probably don’t need any surgery. However, if you’ve had TFCC surgery and it went bust, then begin looking at non-surgical options!
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.