Figuring Out a Complex Patient with an SI Joint Cyst: Interventional Orthopedics
Should we perform a low back or SI joint fusion on an active young woman just because we don’t know why she hurts? SR is a 15 year old cheerleader who was referred to our clinic because of severe and disabling low back pain. She went from a competitive cheerleader to being in severe pain, unable to walk without crutches and in bed most of the day. She had been off school for months. Her major medical diagnosis was a pars fracture at L5-S1. She had tried all the traditional steroid based pain management procedures like facet injections, SI joint injections, epidurals, etc… All were no help. She had also failed PT several times, chiropractic, and acupuncture. Prior to seeing us, she had seen a local alternative doctor who tried prolozone (prolotherapy plus ozone). This is the only treatment that provided a few days of temporary relief.
She was finally referred to our clinic by a local chiropractor. This was a difficult case, one where I had serious doubts we could help. From reviewing her records, almost all of her physicians were very focused on the pars fracture (this is a part of the vertebra often seen injured in active kids), but when I ordered additional imaging, it was healed or not found at all on various images. However, there were some clues in her history about what may be really causing her disability.
Like many flier cheerleaders, she had been dropped just before the onset of all of this, landing on her back side. When patients get this kind of trauma, it’s usually an SI joint injury (the joint between the tailbone and side of the hip). However, someone had already injected that joint with high dose steroids and this didn’t work. On the other hand, blind prolozone injections into the SI ligaments did provide some relief. Since the SI is a difficult joint to get into and few providers can accurately document that they have injected the joint accurately, I decided to re-inject the joint. Several years ago I published a paper on a better SI joint injection technique that allows us to more reliably get injections into that difficult to inject joint. After that first SI joint procedure, her whole leg immediately went numb and became weak. This made no sense, as the SI joint doesn’t connect with any spinal nerves at all. However, this also provided a second telling clue. The only way her leg could go numb as a result of this injection was if the major nerves that travel from the spinal cord to the leg (lumbosacral plexus) were being contacted by a leak or cyst in the front of the SI joint.
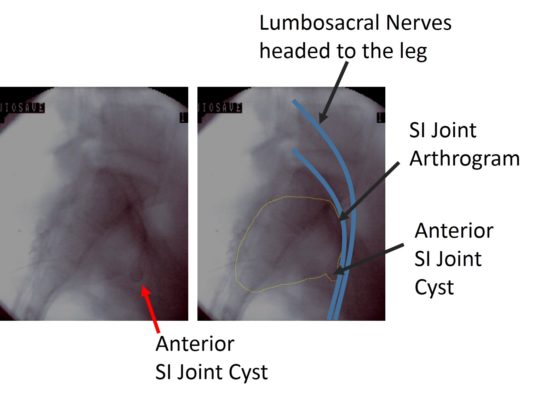
The next injection into the SI joint that was performed was an arthrogram (an injection of radiographic contrast to outline the joint). This is above. The first thing that jumped out was a very uncommon cyst in the front of the SI joint. This made sense, in that injecting anything into the joint would make the cyst temporarily bigger and press on the nerves that supply the leg (which are shown above in blue, traveling right past the cyst). The next step? Use regenerative therapies in the SI joint to get rid of the cyst. The end result? The patient’s pain is now a 1/10 and her leg strength has returned. She’s off crutches and walking normally and has just started rehab to return to competitive cheer leading
The upshot? Just placing magic stem cells or platelets into random areas that hurt, blind without any rationale, often doesn’t work. However, a sophisticated and thoughtful approach to finding the cause and applying a common sense therapy is what interventional orthopedics is all about. This also distinguishes it from surgical orthopedics, which would have led to a low back fusion to treat what was initially seen on imaging (the pars fracture). Performing a fusion in an active 16 year old would have been sub optimal to say the least, leaving her with a lifetime of overload injuries above and below the fused area. In particular, it would have almost certainly made the SI joint cyst much worse! The other approach favored by surgical orthopedics would have been an SI joint fusion, again leaving this active young girl with a lifetime of overload injuries at the levels above and below (the L5 area and the hip joint). Instead, a single well placed injection as an SI joint fusion alternative, was all she required.
NOTE: All Regenexx procedures are medical procedures and therefore have a success and failure rate. Not all Regenexx patients experience the same results.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.