Using Upright Cervical MRI to Diagnose CCI

Credit: Shutterstock
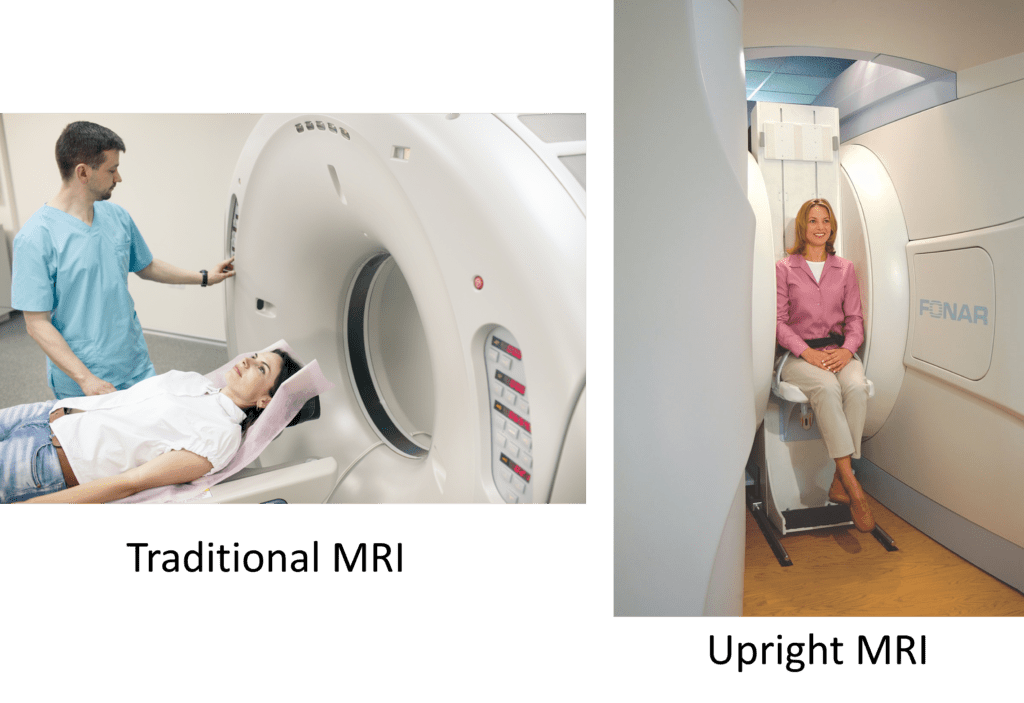
Neck MRI is often an art and there are units that allow the patient to be imaged while sitting or standing. Today we’ll get into why these units can be very helpful and how that impacts the diagnosis of Craniocervical Instability or CCI. Let’s dig in.
What Is CCI?
CCI stands for Craniocervical Instability. That means that the ligaments that hold the head on have been damaged and this can cause headaches, dizziness, imbalance, or other symptoms. To learn more, read my book on craniocervical instability (form to get the book at the bottom of the page).
What is Upright MRI? Traditional MRIs are usually a claustrophobic affair with the patient lying face up in a tube. Upright MRI means that the patient is seated or standing in a machine that is open to the room:
Credit: Shutterstock
Upright MRI has positives and negatives. One of the big positives is that it can show what’s happening to structures as they move. This is the “killer app” of this technology. For cervical instability, that can mean that bones that should stay aligned as the patient moves can be followed to see if they move too much, indicating ligament injury and instability. In addition, the patient can be MRI’ed while weight-bearing, which may show different things than what can be seen when lying face up in a tube. One of the downsides of the technology is that the images won’t be as clear as a lie-flat MRI which isn’t designed to allow motion.
Weight-bearing vs Not
In the neck and low back, many providers who have used both upright and traditional lie flat MRI have noted finding more pathology in the weight-bearing position of an upright unit. Why? Disc bulges are generally bigger and more “true to life” as most of these are symptomatic when upright and not symptomatic when lying down. The same holds true for instability as you’ll see below.
Things that Indicate Instability that May or May Not Be Seen on an Upright MRI
Below are several things we look for to determine if someone has Craniocervical Instability (CCI). Let’s go through these to see how this technology performs in each instance:
C1-C2 Overhang
Credit: Christopher Centeno, M.D.
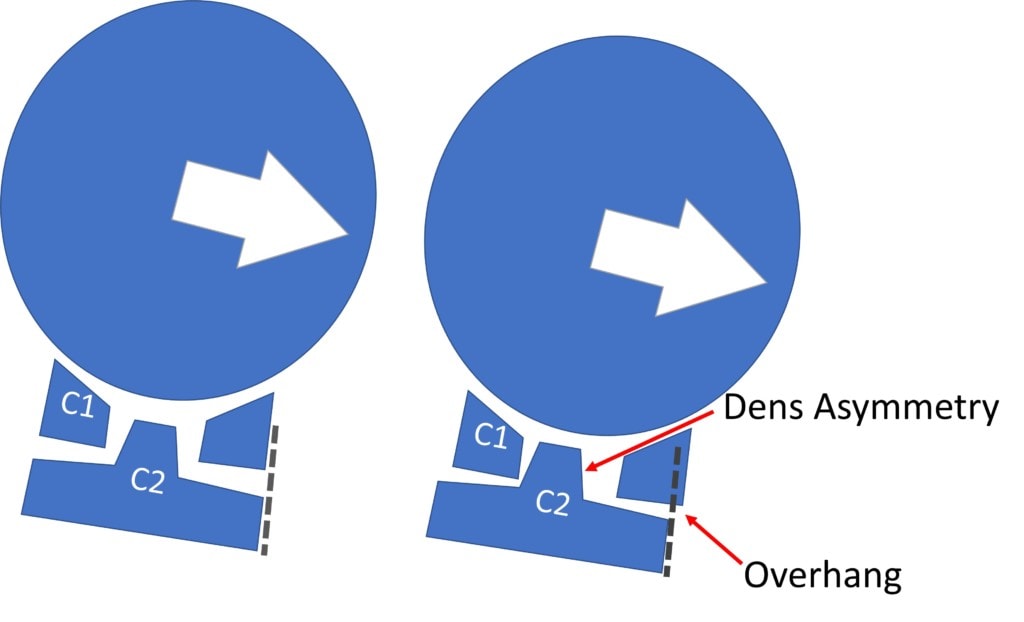
This measurement of how much C1 “overhangs” C2 with side bending is usually used with a technology called Digital Motion X-ray or DMX. When C1 overhangs (slips sideways) C2 more than 3 mm, that’s an indication that this is likely to be traumatic CCI (1). That’s usually caused by Alar and/or Accessory ligament injury. However, having someone laterally bend in an upright MRI and then trying to get this data on an overhang measurement, in my experience, rarely shows the same things as we find on a DMX study. This is because this type of overhang happens for only a second or two in the right position on DMX and you just can’t get an MRI image that quickly. Hence using upright MRI to get an overhang measurement is just not a good application of this technology.
What can you see with lateral bending on upright MRI? You can see the Dens become asymmetrical in the Atlas as shown above. By itself, this may or may not mean much, but it is another piece of the CCI puzzle that can be correlated with other imaging findings and/or symptoms and a hands-on physical exam to help make a diagnosis.
Dens Movement in Flexion and Extension
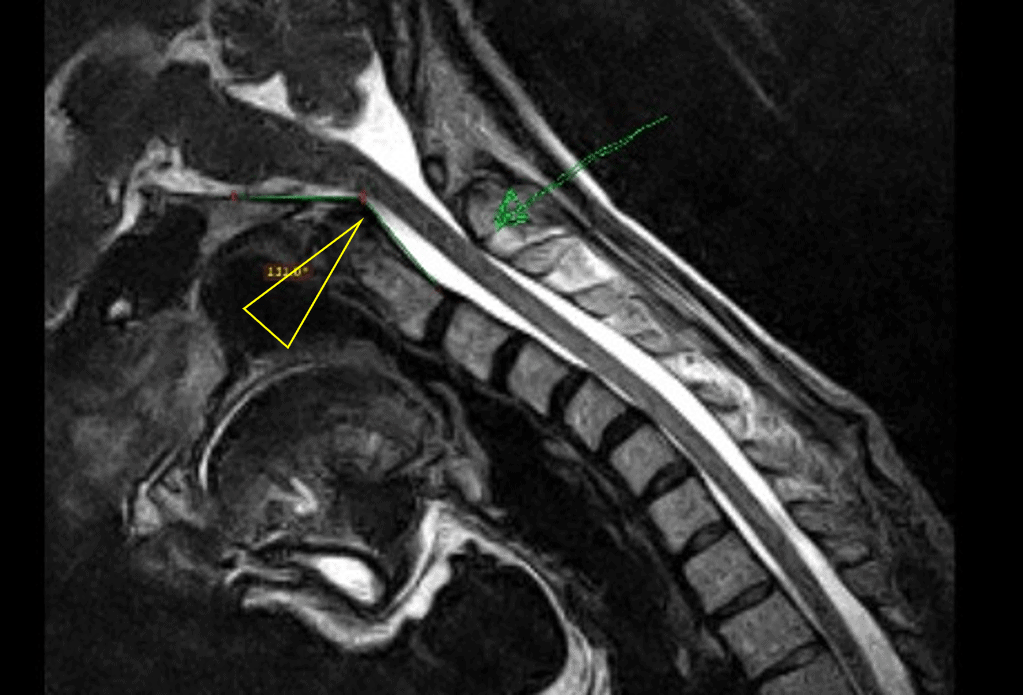
Credit: Christopher Centeno, M.D.
In this case, we’re looking for the posterior movement of the Dens of C2 with neck flexion (yellow triangle above). This can be compared to that position in neutral versus extension. This measures the strength of the Transverse ligament. To see if this is happening, a measurement called the Grabb-Oakes Measurement can be compared. If it increases more than 2-3 mm between the flexion and extension position and the Dens comes close to the upper spinal cord and brainstem in flexion, this is an indication of CCI. Upright MRI is a good technology for this measurement.
C1 or C2 Motion in Flexion and Extension
This one is interesting as it requires a good MRI image, but again, it can be very helpful in identifying CCI using upright MRI. Patients are often told by upper cervical chiropractors that their C1 or C2 bones or both are rotated. Can you see this? Yes, in some CCI patients. In these patients, you can often see the C2 bone being off and out of position on one side or the other. Below is a new video with a detailed explanation of just such a case:
Where Upright MRI is Less Helpful
As discussed above, if the goal is to get the best image of a ligament possible, then the higher the magnetic field the better. Regrettably, upright MRIs have lower magnetic fields. Hence, while static lie face-up MRI machines can’t show damaged ligaments based on too much motion, they do provide better images of what those damaged ligaments may look like.
The good news is that we often get so much information from upright MRIs, that we rarely rely on traditional lie face-up MRI machines. However, there are a few times that having this greater clarity of image helps.
The upshot? Upright MRI has its distinct advantages, especially when motion is involved. It’s usually the preferred type of MRI to diagnose CCI given the information it can provide.
______________________________
(1) Freeman MD, Katz EA, Rosa SL, Gatterman BG, Strömmer EMF, Leith WM. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int J Environ Res Public Health. 2020 Mar 5;17(5):1693. doi: 10.3390/ijerph17051693. PMID: 32150926; PMCID: PMC7084423.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.