CCI and DMX: Can You Still Have Instability with a Normal DMX? What Is a False Negative?

Credit: Shutterstock
You can’t beat movement-based imaging for finding Cervical Instability. However, all imaging has a false-negative rate. Let’s discuss that and learn about instability in the process. Let’s dig in.
What Is Instability?
If you had to choose a single concept of what goes wrong in the spine as the most important thing you should know, it wouldn’t be bulging discs, herniated discs, sciatica, or bone spurs. It would be instability. What’s that and why?
The spine is like a tall building made up of lots of floors. Each floor is a vertebra (spine bone) and is stacked on the other floor like a building. However, the difference is that the tall building doesn’t have to move like your spine. That ability to be both stable and move creates a tremendous engineering challenge.
Solving the problem of something stacked 24 vertebrae high that moves is all about dynamic stability. Meaning, we have to keep these bones perfectly aligned as the spine bends into a c-shape. Doing that with millimeter precision takes two things:
- Ligaments
- Muscles
The ligaments act as duct tape that holds the bones together. The muscles provide fine-tuning of the position of each vertebra relative to the next while the whole unit bends. It’s quite the symphony of precision timing as each small muscle does its job within milliseconds of the next.
What happens when the ligaments get damaged or the muscles no longer contract with such precision? The spine becomes unstable. That means that one vertebra moves in a weird way relative to the next and that can cause all sorts of problems. For example, the joints where the vertebrae meet can get beat up and arthritic, the nerves or spinal cord can get banged into and misfire and the muscle tendons can get badly overworked and become painful. That’s called instability and it’s the single biggest problem that people face that causes chronic neck or back pain.
The spine surgeon’s solution to instability is usually to bolt the problem vertebrae together in a procedure called Fusion. However, this creates as much of a problem as it solves, as now two bones that were built to move no longer move at all, causing overload above and below the Fusion. Hence, Fusion is at best a bull in the china shop solution to a complex problem.
CCI is just one type of instability where the skull (cranial) and the neck (cervical) meet (CCI=craniocervical instability). We’ll focus here today to demonstrate a problem called a false negative test.
How Is Instability Diagnosed?
Since instability involves movement, it makes sense that movement-based imaging would be the way to detect it. However, since spine imaging with movement is less common, most doctors try to diagnose instability on common static x-ray or MRI images. However, there are some much better image types where motion is used.
These moving spine images include flexion-extension x-rays, upright MRI, CT Scans in different positions, and DMX. That last one is where we’ll focus today, as it’s the most natural of the four. This test known as a Digital Motion X-ray is a live video of the spine in motion. For the neck, there are published standards for what’s normal and not (1). The idea behind DMX is simple, we observe how the bones move against each other, and if there is excessive motion, the ligaments or muscles or both aren’t doing their job to hold the neck bones together.
What’s a False Negative?
All medical diagnostic tests have false negative and false positive rates. For a false negative, this means that the test showed normal, but the disease was actually present. For DMX in the context of the blog this morning, this means that the study failed to find instability, even though it was really there. Let’s look at a case example from yesterday’s clinic that has to do with a neck measurement called the ADI.
What Is the ADI?
ADI means Atlanto-Dental Interspace. This is the distance between the front of the C1 bone and the Dens of C2. The two fit together like this:
That upward projection on C2 (Dens or “tooth” in Latin) fits inside the ring of C1 and acts as the rotation point for much of your ability to turn your head and neck. The Dens has a “seatbelt that holds it against C1 called the Transverse Ligament (shown in red here):
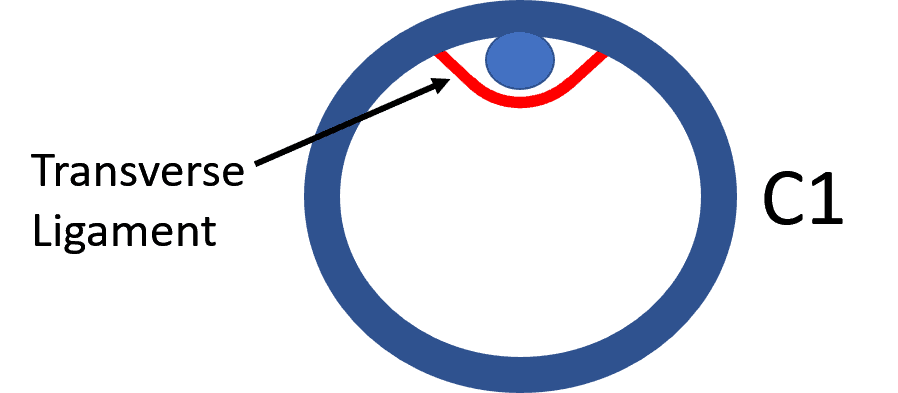
If you look down and flex your neck, the Transverse Ligament keeps C1 and C2 held firmly together. The distance between the two bones is called the ADI (Atlanto-Dental Interspace). That’s not supposed to be more than around 2-3 mm (2).
A Seriously Problematic ADI Missed by DMX
Yesterday, I was performing a second PICL procedure on a patient who did well with the first, but then got into a car crash. Since the procedure injects these ligaments that hold the head on to help a patient avoid neck Fusion, the great news was that her second DMX showed a significant 50% improvement on a measurement called “overhang” and a normal ADI. Hence the second procedure was meant to fix the problems caused by the new car crash. However, during the procedure, as we had her asleep and in flexion, I got a big surprise:
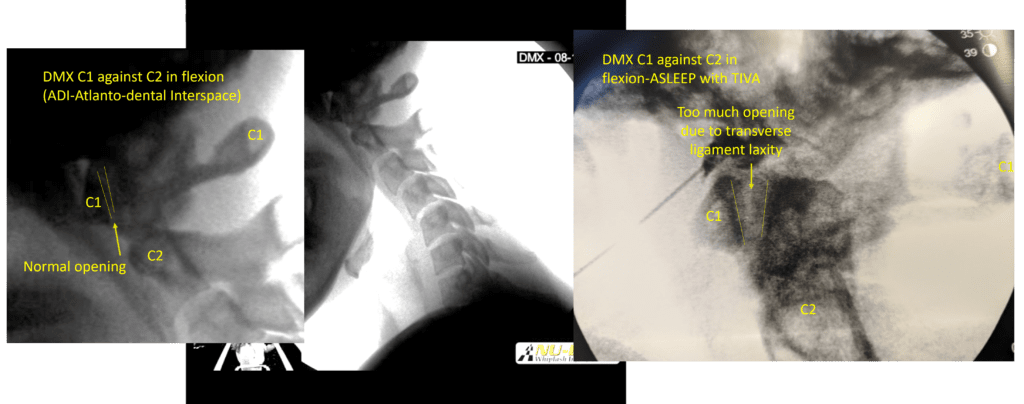
While this may look like a bunch of mishmash to you, focus on the yellow vertical lines on the left. On the DMX there, those lines represent the ADI. On the right is the image from the procedure. Note now that the vertical lines are now much farther part (6 mm at their widest). Why the HUGE difference?
In the DMX, she’s conscious and the muscles are working their magic to keep the dens plastered onto C1. However, during the procedure, she’s been put to sleep with anesthesia and her muscles are taken out of the picture. Here her body is relying only on the Transverse Ligament, which in this case is loose. Hence, the ADI opens up.
What does this mean for this patient? That she’ll likely need a few more treatments of this Transverse Ligament. However, she’s young and has already responded favorably to a single injection of her own Bone Marrow Concentrate into these ligaments, so maybe one more will get it done.
Ligaments are The Last Defence Against Instability
This example shows the function of muscles and ligaments in terms of stability. When you’re conscious or when the muscles are working well, the ligaments are less active in ensuring stability. However, when the muscles are off-line, either due to sleep, fatigue, or injury, the ligaments are your last defense against vertebrae moving too much. Hence, any treatment solution that tightens ligaments also needs a muscle-strengthening component as well.
The upshot? False-negative tests in medicine happen all the time. Given that I have seen this one several times (open ADIs during procedures that looked fine on DMX), I intend to start recording these to figure out the false-negative ADI rate for DMX. This also means that we’ll likely have to take some patients who have all of the clinical aspects of CCI and a normal DMX and put them asleep and retake a few images to see if their ligaments fail once their muscles are taken out of the picture!
________________________________________
(1) Freeman MD, Katz EA, Rosa SL, Gatterman BG, Strömmer EMF, Leith WM. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int J Environ Res Public Health. 2020 Mar 5;17(5):1693. doi: 10.3390/ijerph17051693. PMID: 32150926; PMCID: PMC7084423.
(2) C.A. Rojas, J.C. Bertozzi, C.R. Martinez and J. Whitlow. American Journal of Neuroradiology October 2007, 28 (9) 1819-1823; DOI: https://doi.org/10.3174/ajnr.A0660
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.