A Case Study of Severe CCJ Instability and Our PICL Procedure
CCJ instability is a life-changing problem. Think about the havoc that could be caused by the ligaments that hold your head being injured by trauma or becoming loose due to a connective-tissue disease. Headaches, imbalance, and a myriad of other symptoms become the new normal when you attempt to do anything. This morning, after several years in the making, I’d like to discuss the objective results of our new PICL procedure by reviewing the case of a patient with severe CCJ instability.
Defining CCJ Instability
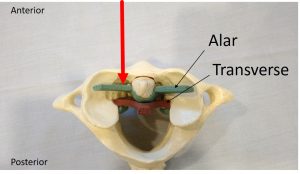
The craniocervical junction (CCJ) is at the top of the spinal column where the head meets the neck. Strong ligaments—the alar, transverse, and accessory ligaments (and others)—hold the CCJ together. A new ligament complex called the ventradural ligament (VDL) has also recently been discovered here. CCJ instability occurs either when there is an injury to these ligaments or due to disease and normal wear and tear with aging. The result is that the ligaments loosen and the upper-neck joints become unstable. This can lead to arthritis in these joints, tendon inflammation, nerves being pinched, and so on.
What might cause an injury to the CCJ ligaments? While there are congenital conditions, such as Ehlers-Danlos syndrome (EDS) that are associated with CCJ instability, the ligaments can also suffer traumatic injuries, such as head or neck trauma. Examples include a rear-end car accident or a blow to the head in sports or some other activity or accident. Symptoms can include dizziness, visual and cognitive disruptions, headaches, and so on.
A Rose by Any Other Name
Before we discuss this new procedure or the results of this treatment, it’s important to note that CCJ instability has many different names. Other monikers include, cranial-cervical syndrome, hypermobility of the cranial-cervical junction, atlanto-axial instability, atlanto-occipital instability, craniocervical instability, craniocervical injury, upper cervical instability, and so on. Now let’s review our interventional orthopedic procedure for addressing CCJ instability called the PICL procedure.
What Is a PICL Procedure, and How Is It Performed?
PICL stands for percutaneous implantation of the CCJ ligaments. I’ve been slowly blogging on this topic for years, revealing more about this new procedure each time. I wanted to wait until we got well past 100 safe procedures and until I had a chance to fully grasp its efficacy before giving it a name. However, it’s now time for what we had called the “CCJ instability procedure” or “alar procedure” to get the more formal PICL label.
During a PICL procedure, bone marrow concentrate (BMC) that contains a stem cell fraction (same-day stem cell procedure) is injected directly into the CCJ ligaments. The percutaneous approach to reach these ligaments is through the posterior oropharynx (the back of the throat). It requires an endoscope to establish and maintain a sterile field and place the needles. It then also uses advanced and precise fluoroscopic (real-time X-ray) guidance with radiographic contrast to ensure the correct ligaments are being injected. The red arrow in the image below provides a visual of the injection vector.
©Regenexx
Why is a PICL procedure better? This is an interventional orthopedic procedure that utilizes a percutaneous minimally invasive technique to treat CCJ instability, meaning it’s much less invasive than surgery. The purpose is to prevent highly invasive cervical fusion surgery, which will immobilize the upper neck by bolting the head to the upper neck bones and will create more problems, such as adjacent segment disease, down the road. Learn more about our PICL procedure for CCJ instability in my early video below:
A PICL Procedure Case Study of a CCJ Instability Patient
The patient is a physical therapist who was involved in a car crash in 2009. He had severe CCJ instability, a lower cervical disc bulge with pinched nerves, upper cervical facet joint injuries, and a traumatic brain injury. He had symptoms in his arms due to the lower-neck disc bulge, but most of his disability was related to the upper neck. I had treated the lower-neck for a couple of years with platelet lysate epidurals, which managed the symptoms in his arms.
He was seen this week for his fourth procedure, after a series of three PICL procedures. His first was in February 2017, the second was in October 2017, and the third was June 2018. Before, during, and after these three procedures, I measured the lateral movement of the C1 neck bone on the C2, called the C1–C2 overhang, while the patient bent his head to the side. A damaged alar ligament allows too much overhang, and that can cause upper cervical symptoms. You can watch my featured video at the top of the page for a detailed timeline and dramatic visuals of his progress, but briefly, here are his current results (prior to his fourth procedure):
- Left C1–C2 overhang has reduced by more than 50% (5.6 mm to start, currently 2.3 mm)
- Right C1–C2 overhang has reduced by a whopping >80% (7.2 mm to start, currently 1.2 mm)
How do these results translate to the patient? He’s reporting about a 65% improvement. Before his procedures, he could only walk about 100 yards max; now he can do four miles. He does still have some head injury symptoms, and it’s important to note that there are things he still doesn’t do. However, his life has changed from highly disabled to just significantly limited in certain activities. In summary, the PICL procedure has dramatically improved his function, and objective imaging that measures his CCJ instability has supported that conclusion.
Where Is the PICL Procedure Performed? Are There Research Studies?
Currently, the PICL procedure can only be performed at our Regenexx HQ in Colorado. We have a few physicians there who have trained directly with me and who also perform it. Given the complexity of the anesthesia, the use of multiple imaging modalities, and the procedure itself, it’s unlikely that I will be teaching this one to anyone else outside of Colorado for a while. That will have to wait until we get multiple publications in print.
We have an ongoing randomized controlled trial (RCT) research study currently in process for our PICL procedure. This is a free study, but you have to meet certain inclusion and exclusion criteria as well as agree to be randomized to the sham procedure (where you will be put to sleep and the back of your throat will be poked without the PICL procedure being performed). The good news is that you can cross over from the placebo group to the real PICL procedure at six months.
We have been very cautious over the last four years as we have developed this procedure, and now we feel comfortable with the risk-benefit profile to share the first clinical results. These will generate a large case series publication with objective imaging analysis, which is in the works. So we’ll have research published even before the RCT is completed.
The New CCJ Instability Institute
One of the things we have seen in treating CCJ instability for more than 20 years is that few physicians know much about this issue. This extends to specialists such as surgeons and interventional spine doctors who should know more. As an example, just arranging an upper-cervical facet injection for our CCJ instability patients is tough. There are fewer than 100 US physicians who have any substantial experience (performed 20 or 30 or more of these injections) and fewer than 10 who have a lot of experience (performed more than 100). As a comparison, we have performed thousands.
As a result, we are forming the CCJ Instability Institute. This will highlight the fact that we’re one of the few places on Planet Earth with expertise in the minimally invasive treatment of the upper-cervical spine. In addition, one of the missions of the institute will be to educate physicians on these problems so that CCJ instability patients don’t get a blank stare when they see a doctor. So stay tuned for more info as this is launched.
The upshot? The PICL procedure is proving itself to be a game changer. While we know we have much more research to finish to prove our point that most CCJ instability patients don’t need a hyperinvasive surgical fusion, we will begin to share more and more results. Also, we’re launching an entire institute to make sure that CCJ instability patients who want to avoid surgery have a home.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
