Alar Ligament Treatment for CCJ Instability
Due to our high level of expertise in the field, for many years, our practice has collected a group of patients with upper cervical (CCJ) instability. This awful problem has been very difficult to treat, but the patients have been generally happy that any physician knows what’s wrong with them and is willing to do something about it. However, for years I’ve known that there was more that could be done, but there was just no way to get it done. This is the story of a new injection technique (alar ligament treatment) we now use to help these difficult-to-treat patients.
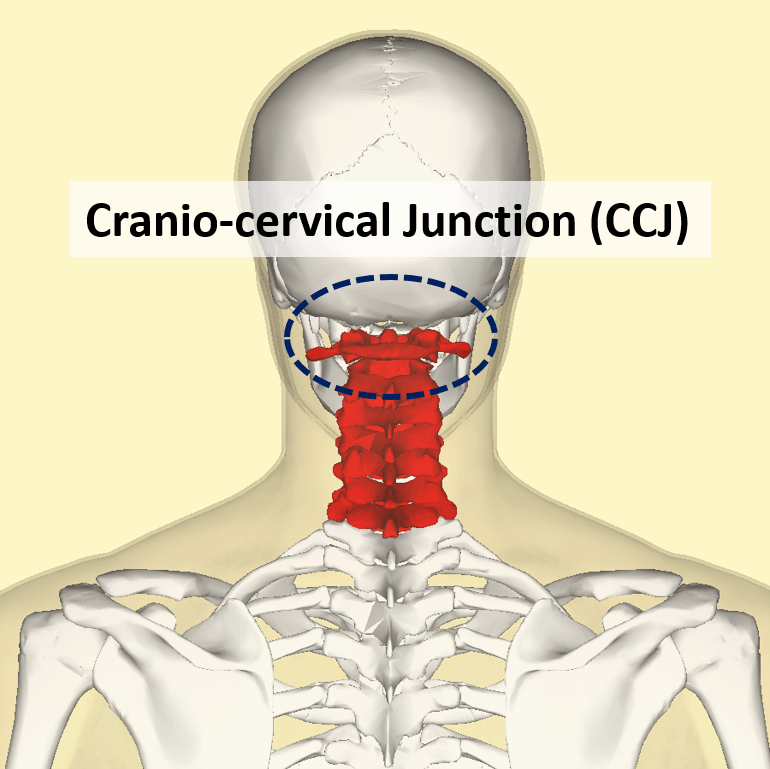
The Upper Cervical Spine and CCJ
The uppermost neck is called the craniocervical junction (CCJ). It includes the skull, which sits on the atlas bone (C1 vertebra), which sits on the axis bone (C2 vertebra). So the CCJ is the skull though C2.
As we develop in the womb, the upper neck and head actually develop as one unit. Hence your brain doesn’t differentiate one from the other when it comes to deciphering pain signals. Hence, patients with upper neck problems often experience headaches.
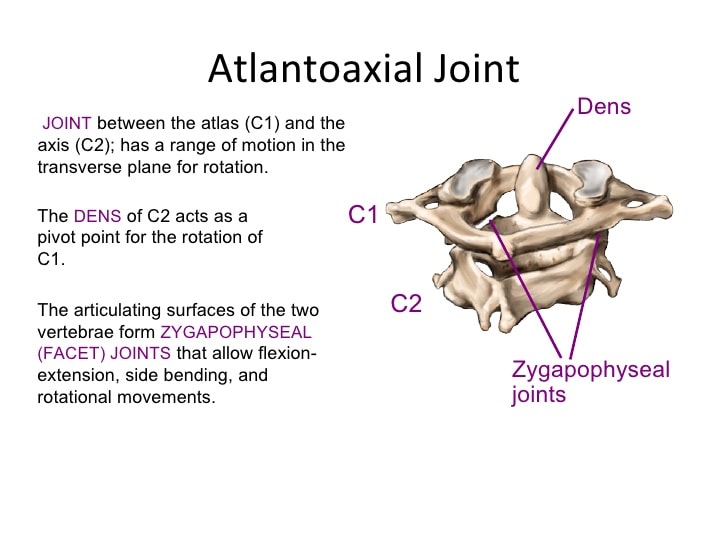
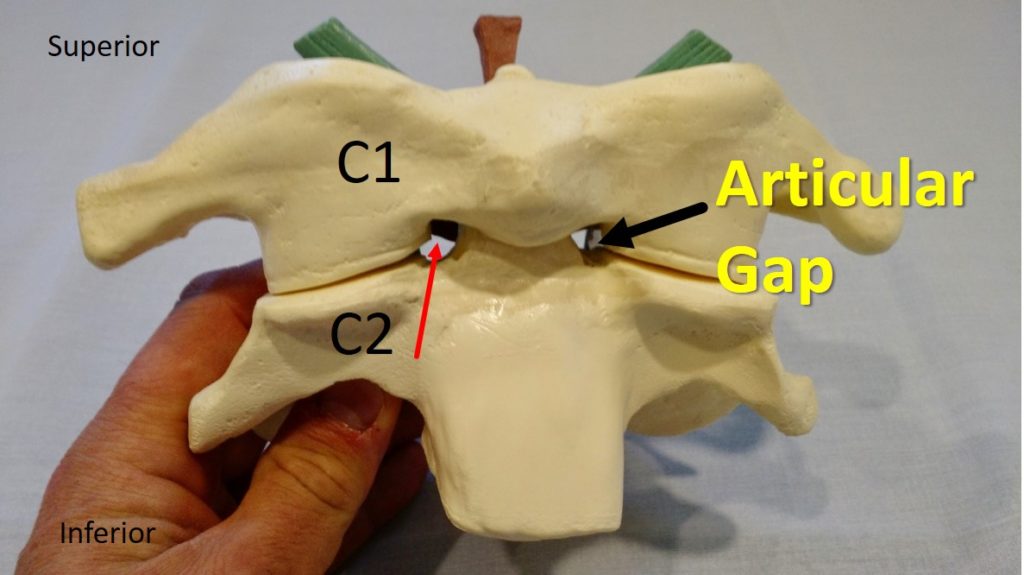
The upper neck has facet joints, just like the rest of the spine. These normally finger-sized joints are larger than usual and are actually the biggest spine joints. The C0–C1 joint facilitates a head-nodding motion, and the C1–C2 joint allows for 50% of head rotation. In fact, the C1–C2 facet joint is the most mobile joint in the spine.
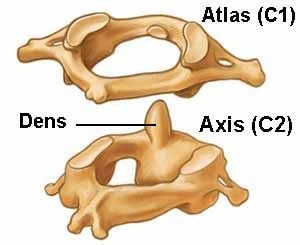
The C1 and C2 vertebrae fit together like a complex puzzle. There’s a projection on the C2 bone (called the dens) that sticks up and acts as a pivot point for the C1 bone. The skull then fits together with the C1 bone with two projections from the bottom (occipital condyles) that sit into the C1 bone.
The Ligaments That Hold This Area Together
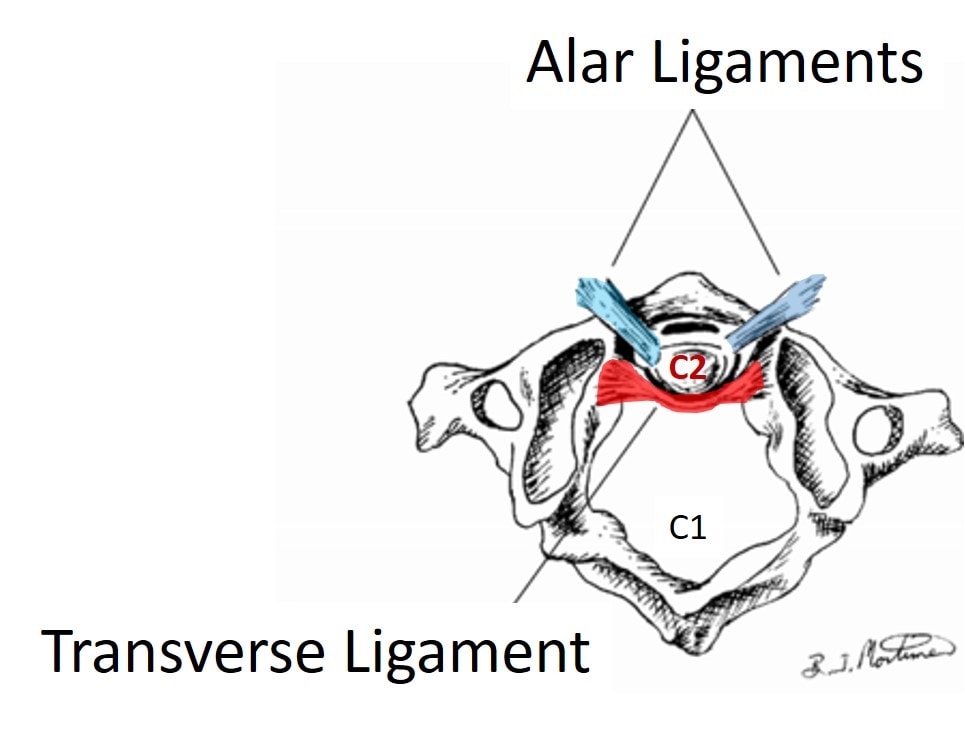
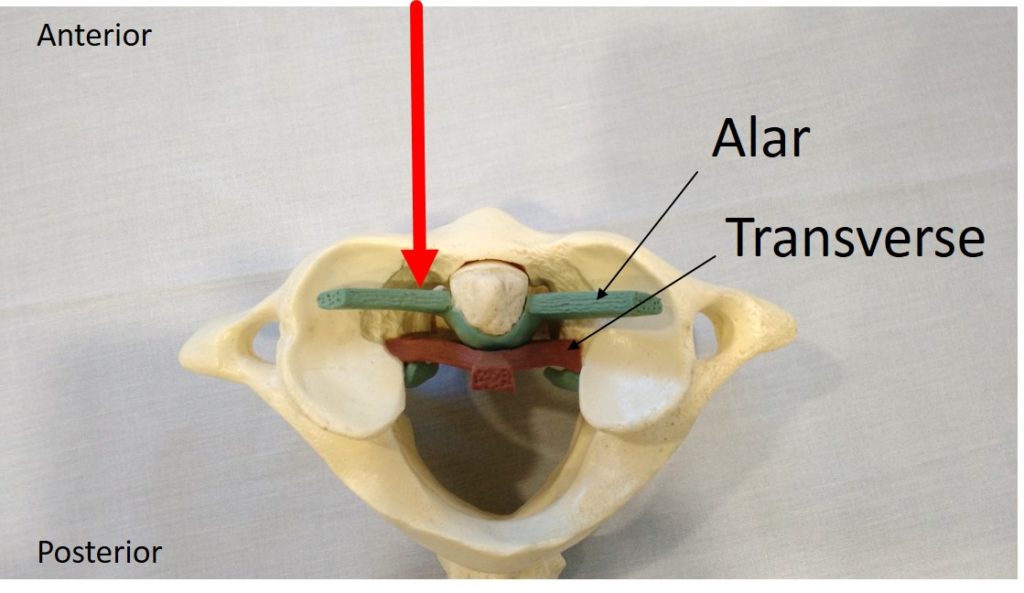
Ligaments are like duct tape that hold the bones together. In the CCJ, the two main ligaments are the alar and the transverse. They literally hold your head on.
The alar ligaments (blue in the image below) come up from the dens and connect the C2 vertebra to the skull. The transverse ligament (red) acts as like a seat belt for the dens. These ligaments stabilize the upper neck when you look down, turn your head, or do both.
What Happens When These Ligaments Get Injured?
Any ligament in the body can be injured in two ways—it can be broken in half and can snap back like a rubber band (known as failure), or it can stretch and get partially torn (subfailure). In the case of the alar and transverse ligaments, the former type of ligament injury is much more common. This means that the upper neck bones become unstable and move around too much. Just like other areas of the spine, when this happens the facet joints (in this case C0–C1 and C1–C2) can be beat up by that movement, leading to arthritis. The muscles and tendons that should stabilize this area become overwhelmed and injured. Finally the nerves can become irritated.
What Causes These Injuries, and What Are the Symptoms?
Injuries to the alar and transverse ligaments can occur with head trauma. Through the years I’ve heard many ways that these areas can be injured including the following:
- A rear-end car crash, especially one where the head hits the back window (e.g., a pickup truck)
- A sudden jolt to the neck/head
- Something falling on the head
- Placing axial loads on the head (e.g., one patient who performed a neck exercise by arching his back to place his whole weight on the head)
Patients usually complain of headaches; dizziness/vertigo (but not always); visual disturbances; disorientation; and/or problems thinking, concentrating, or reading. The symptoms are usually worse with head turning or looking down. There may be clicking or popping and activity such as exercise or physical therapy usually makes the problem worse. Very specific upper cervical manipulation (i.e., by an experienced upper cervical chiropractor or high-level manual therapist) can provide temporary relief.
What Alar Ligament Treatment Is Available for These Patients When Conservative Care Fails?
Many different kinds of injection therapy can be attempted in these patients, but few of them yield any long-term or “home run” results. Through the years, we’ve tried traditional cervical facet injections at C0–C1, C1–C2, and C2–C3. We’ve tried platelet rich plasma (PRP) and stem cell injections into the joints as well. We’ve also tried injecting the ligaments in this area (prolotherapy, PRP, and stem cells). All of this only provides either temporary or small amounts of relief. The same holds true for alternative therapies, including acupuncture, massage, body work, craniosacral therapy, etc…
The big problem with all of this treatment is that there has been no way to get at these ligaments. When coming from the traditional posterior (from the back) approach, the spinal cord is in the way. Several years ago we began to wonder if there was any way that these ligaments could be accessed.
Why is an Non-surgical Alar Ligament Treatment Important?

Yok_onepiece/Shutterstock
The most common surgery offered these patients when conservative and injection-based therapies fail is CCJ fusion. While there may be patients who have such severe CCJ ligament injuries that only bolting together the bones will work, as I tell my patients, “Fusion is a dog with fleas.” This means that fusing any segments of the spine will result in the spinal segments above and below getting overloaded and degenerative. Just take a look at the X-ray here to get a sense of why a CCJ fusion should be avoided if possible.
Getting at the Alar/Transverse Ligament
I spent several years occasionally noodling this problem. This then progressed into about a year spent focusing on how to make this work. I figured out a few posterior approaches to the ligaments, but they all seemed to work better in theory than practice as the spinal cord was always in the way. Then one day I was playing with a model of the upper cervical spine we have in the office. I noticed that the model had a little hole between the C1 and C2 bones. Could it be possible that a needle could be placed through this “articular gap”? Theoretically it should be possible, but nobody had ever attempted this procedure.
I spent the next year researching this approach, reviewing anatomy texts, and consulting with high-level colleagues to ensure this procedure would be possible. In February of 2015, I was ready, and given that we had a collection of these CCJ instability patients that had failed everything, it wasn’t hard to find a patient who had been living with this nightmare collection of symptoms.
Before the first procedure, we had many questions. Was it possible that this “articular gap” was a figment of the imagination of anatomy textbooks and models and wouldn’t allow a needle through? Was there some other reason that this couldn’t be done? Thankfully the first procedure went well, and we soon found out that this “articular gap” was for real. We got a very thin 25-gauge needle into this gap and then into the alar/transverse ligaments from the front. A blue-collar guy who had years of headaches after a car crash, who I couldn’t help in any way, told me that while he was sore for two weeks, one day he noticed a dramatic improvement and most of his headaches went away.
More Experience with This First-of-Its-Kind Procedure
Over the last year, as the video discusses, we were able to treat seven patients in 10 different procedures. All of these patients (except one who was not worked up by us) had failed all other treatments. Five of seven had excellent results for the first time ever, with many logging dramatic results. Examples included a patient who couldn’t sit in meetings who can now have one-hour meetings with a several-minute break and do this all day. This same patient can now cross-country ski for the first time in years. A patient who couldn’t sit in a car without her upper neck “going out” e-mailed that she went on a multimile backpacking and hiking trip! She had been treated by us for a decade with only small, incremental improvements.
Of the two patients who didn’t respond, one had a suboptimal injection (before we had perfected the procedure) and another had a poor diagnostic work-up before seeing us. In that patient, his pain was actually coming from an injured C1–C2 joint, which we later discovered (i.e., CCJ instability was not the problem that was driving his symptoms).
Above is a video that goes into this topic in much more depth. It represents our first public presentation of this technique at a medical conference, which occurred this week at the annual AAOM meeting.
The upshot? Alar ligament treatment is feasible and seems to give home-run results in the patients who had failed many other therapies. We’ll now move from seeing if this procedure is feasible to more formal study of the results when many more patients are injected. The meantime, I’m grateful that we now have a way to help these poor patients with this awful problem.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.