Buttock Pain After Hip Replacement? It Could Be Your Tendons
On this page:
- Why gluteal tendinopathy is a pain in the butt
- Hip replacement with gluteal tendinopathy
- How to avoid butt pain after hip replacement
- How to treat pain after hip replacement
- Other causes of pain after hip replacement
- What we know about hip replacement
If you’re planning a hip replacement or have already had one, a new study could mean you should be looking at the health of your tendons. Why would your tendons matter if you have arthritis of the joint? Is there a way to avoid or fix continued pain after hip replacement? Let’s dig in.
Why Gluteal Tendinopathy Is a Pain in the Butt
Hip Replacement With Gluteal Tendinopathy
How to Avoid Butt Pain After Hip Replacement
How can you avoid pain after hip replacement? Many times these tendon issues will be talked about on your MRI report. So look for terms like “tendinopathy,” “tendinosis,” or “tendon tear” in muscles like:
- Gluteus maximus
- Gluteus medius
- Gluteus minimus
- TFL (tensor fascia lata)
If you don’t have an MRI, take some time to press on these spots:
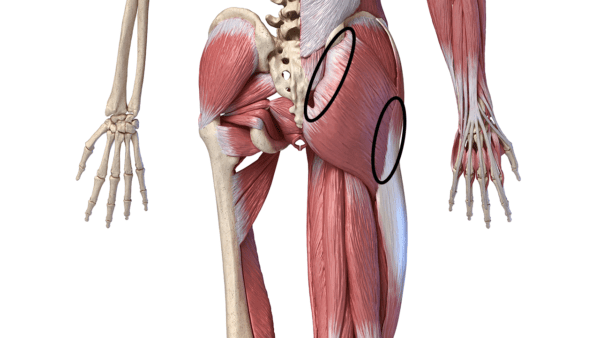
Matis75/Shutterstock
If they’re tender, get an MRI to check if you have gluteal tendinopathy.
How to Treat Pain After Hip Replacement
If you have these gluteal tendon issues, first trying to figure out why is a good idea. For example, irritated nerves in the back can cause this problem. That doesn’t have to be full-on sciatica, it can just be low-level irritated nerves with or without back pain. Since the nerves tell the muscles what to do, bad nerve signals can cause these muscles to misfire and the tendons to get ripped up.
Second, treating the tendons before or after hip replacement is a good idea. The most common way to treat beat up tendons these days is using your own concentrated blood platelets (called platelet-rich plasma or PRP). In this case, ultrasound guidance would be used to guide the needle to the bad parts of the tendon and then relief can be achieved in weeks to months as the growth factors from the platelets stimulate healing and growth of the tendon cells. However, note that if the bad tendons were in fact caused by irritated nerves in your back, the back will need to be treated as well.
Other Causes of Pain After Hip Replacement
First, watch my video above for some causes of butt pain after hip replacement. Then, please read this extensive review of hip replacement materials and sizing and other things that can go wrong. Here’s the abbreviated list of other things that you should consider if you’ve already had a hip replacement and still have pain:
- An allergy to the hip replacement materials (2). The cement used or the nickel and/or cobalt used to make the device are common allergies.
- A prosthesis that is too short or long. This will cause a leg length discrepancy.
- Hip pain that was from elsewhere, other than your arthritic hip. That means that the hip pain could have always been referred from the low back or from the SI joint (see video above). Hence, replacing the hip joint never treated the original pain generator.
- A pseudotumor (3). This is a growth caused by irritation of the local tissues due to the hip replacement device.
- Wear particles from a metal-on-metal or minimally invasive anterior hip replacement (Birmingham hip or “Hip Resurfacing”). This is wear debris that then irritates the tissues and causes pain.
What We Know About Hip Replacement
_____________________________________________
References
(1) Rosinsky PJ, Bheem R, Meghpara MB, et al. Asymptomatic Gluteal Tendinopathies Negatively Impact Outcomes of Total Hip Arthroplasty: A Propensity Score-Matched Study. J Arthroplasty. 2021;36(1):242-249. doi:10.1016/j.arth.2020.07.063
(2) van der Merwe, JM. Metal Hypersensitivity in Joint Arthroplasty. JAAOS. March 2021;5(3). doi:10.5435/JAAOSGlobal-D-20-00200
(3) Bosker BH, Ettema HB, van Rossum M, et al. Pseudotumor formation and serum ions after large head metal-on-metal stemmed total hip replacement. Risk factors, time course and revisions in 706 hips. Arch Orthop Trauma Surg. 2015;135(3):417-425. doi:10.1007/s00402-015-2165-2
(4) Gofton W, Beaule PE. Serum Metal Ions with a Titanium Modular Neck Total Hip Replacement System. J Arthroplasty. 2015;30(10):1781-1786. doi:10.1016/j.arth.2015.04.040
(5) Blizzard DJ, Sheets CZ, Seyler TM, et al. The Impact of Lumbar Spine Disease and Deformity on Total Hip Arthroplasty Outcomes. Orthopedics. 2017;40(3):e520-e525. doi:10.3928/01477447-20170327-03
(6) Harding P, Holland AE, Delany C, Hinman RS. Do activity levels increase after total hip and knee arthroplasty?. Clin Orthop Relat Res. 2014;472(5):1502-1511. doi:10.1007/s11999-013-3427-3
(7) Haynes J, Sassoon A, Nam D, Schultz L, Keeney J. Younger patients have less severe radiographic disease and lower reported outcome scores than older patients undergoing total knee arthroplasty. Knee. 2017;24(3):663-669. doi:10.1016/j.knee.2016.11.004
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.