Hip Replacement or Back Fusion First? Timing Matters When Considering Risks
One of the clinical scenarios where bone marrow concentrate doesn’t work well is severe hip arthritis. In these cases, we often tell patients to get a hip replacement. However, it’s critical to understand that the body is connected, so for example, getting a back fusion may impact your hip replacement. Before I share the newest study, let’s review what we already know about hip replacement and back fusion.
Hip Candidacy for Orthobiologics
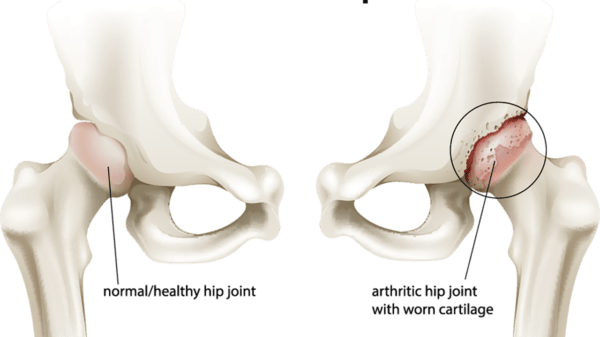
BlueRingMedia/Shutterstock
While mild to moderate hip arthritis can respond to precisely placed platelet-rich plasma or stem cells injected using imaging guidance, the most severe form of the disease doesn’t respond well to these orthobiologics. In addition, hip osteoarthritis (OA) is different than it’s cousin in the knee. While the latter can smolder for years and change only a little bit, hip OA can come on quickly. So time is of the essence in its’s diagnosis and non-surgical treatment.
The Problems with Hip Replacement…
We still send selected patients for hip replacements. However, when we do, we make sure our patients go into the surgery with eyes wide open. Let me explain.
Well-known problems with hip replacement include continued chronic pain after hip replacement; development of pseudotumors in metal on metal joints, which can disrupt function, cause pain, and generally lower outcomes; and a slightly increased risk of stroke.
If you have to have a hip replacement, getting the alignment right and understanding that your hip is connected to your low back are key concepts. Hip replacement has also been associated with not only hip alignment problems following surgery but also knee alignment issues. Why both? The knee and hip work in a close collaboration with one another, so a disruption in the biomechanics of one will put more stress on the other. In addition, if you had low-back problems prior to your hip surgery, there’s an increased risk of continued pain after surgery. If there’s a disc bulge, for example, that is irritating a nerve, this can present as pain in the back and/or anywhere along the nerve branch, such as the knee, hip, ankle, and so on.
It’s important to note that we don’t recommend hip resurfacing, but instead a full hip replacement. Why? hip resurfacing, typically pushed as a less-invasive alternative to hip replacement, has its own big problems that, in some cases, are worse than those with the hip replacement itself. These include pseudotumors, metal particles that slough off these devices causing high levels of metal in patients’ bloodstream, early failure of poorly sized resurfacing prosthetics, and so on.
The Problems with Lumbar Fusion…
Arthritis that develops in segments of the spine adjacent to the fused segment or segments is called adjacent segment disease, and this, unfortunately, is very common following spinal fusion. The reason this occurs is because those adjacent segments are put under a great deal of stress as they overwork to compensate for the immobilized segments that have been fused. More on back fusions and adjacent segment disease in my video below:
Pain, disability, and general quality of life, in most cases, don’t seem to improve any more with a back fusion than they do with conservative measures or physical therapy. In addition, opioid use is common in patients with chronic back pain, and many will opt for fusion as they believe it will get them off the opioid sauce. Unfortunately, the literature isn’t supporting this to be the case. Not only are over 90% of patients who were taking opioids prior to surgery still taking opioids after surgery, but 13% of those who weren’t taking opioids prior to surgery begin taking them after surgery.
If you’ve had a hip replacement and back fusion, we already know this can increase the risk of dislocation. In fact, the more spine levels you have fused, the greater your risk of dislocation following a hip replacement. Now, it seems that even the timing of when you have that hip replacement, either before or after the fusion, has a significant effect on dislocation and revision risks. Let’s review.
Between Hip Replacement and Back Fusion, Which Should Come First?
While we already know side effects for both procedures individually are extensive and significant, the new study looked at side effects in patients who had both a hip replacement and a lumbar fusion. This was a comparison study in which researchers set out to determine whether risks were greater for hip replacement that occurs after lumbar fusion or before lumbar fusion. The results? When compared to patients who had lumbar fusion after hip replacement, those who had lumbar fusion before hip replacement had a 106% increase in dislocation risk. In addition, hip replacement revisions were also greater in those who had lumbar fusion before hip replacement (43% at one-year post hip surgery, 41% at two years, and 49% at five years). In other words, for patients who have had both hip replacement and back fusion, those who have a hip replacement after a lumbar fusion are more likely to have hip dislocations and revisions than those who have a hip replacement before a lumbar fusion.
The upshot? If you have severe hip OA you may need a hip replacement. Understanding what you’re getting yourself into and that your low back can impact that new hip is critical. After all, the backbone is connected to the hip bone and the hip bone’s connected to the knee bone…

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.