SI Joint Fusion: A Case Study of Why Healthcare Costs Are Out of Control
If you’re a company in the healthcare cost containment space, your chances of seriously bending down the cost curve are slim, and none, and “Slim’s on vacation in Texas.” What I mean is that many great ventures have tried to control healthcare costs, and all have failed to make meaningful dents because they approach the problem from the wrong angle. Today I’d like to use one recent popular pain relief procedure to show why these companies have failed and how Regenexx has been successful. Let’s dig in.
“They Tried and Failed? No, They Tried and Died.”
This is a quote from Dune, where Paul is with the reverend mother and asks about men trying the water of life. If you have never read the books or seen either movie, it’s also self-explanatory. It’s also emblematic of all approaches that have tried to control healthcare costs.
Take, for example, the venture between Amazon, Berkshire Hathaway, and JP Morgan called Haven Healthcare. It was announced with great fanfare because of the sheer gravitas of these three outsider businesses. However, within three years of starting the venture, it was shuttered.
Why? The most innovative cost containment systems now involve bundling and capitation. Nothing about these approaches changes the game drug/device manufacturers, physicians, and hospitals play. Today, I’ll explain how that game works using a single device that has taken off like wildfire.
Why SI Joint Instability is a Great Way to Learn About Controlling Healthcare Costs
If you want to understand US healthcare and its perverse incentives, look no further than the panoply of SI joint fusion devices currently on the market. If you’re not in medicine and, in particular, involved in spine care, you probably have no sense of what I’m talking about, so let me begin with some background.
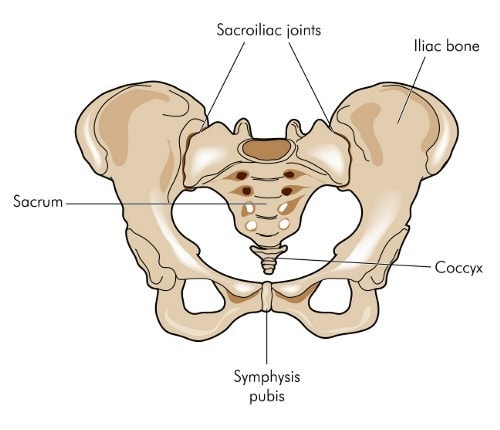
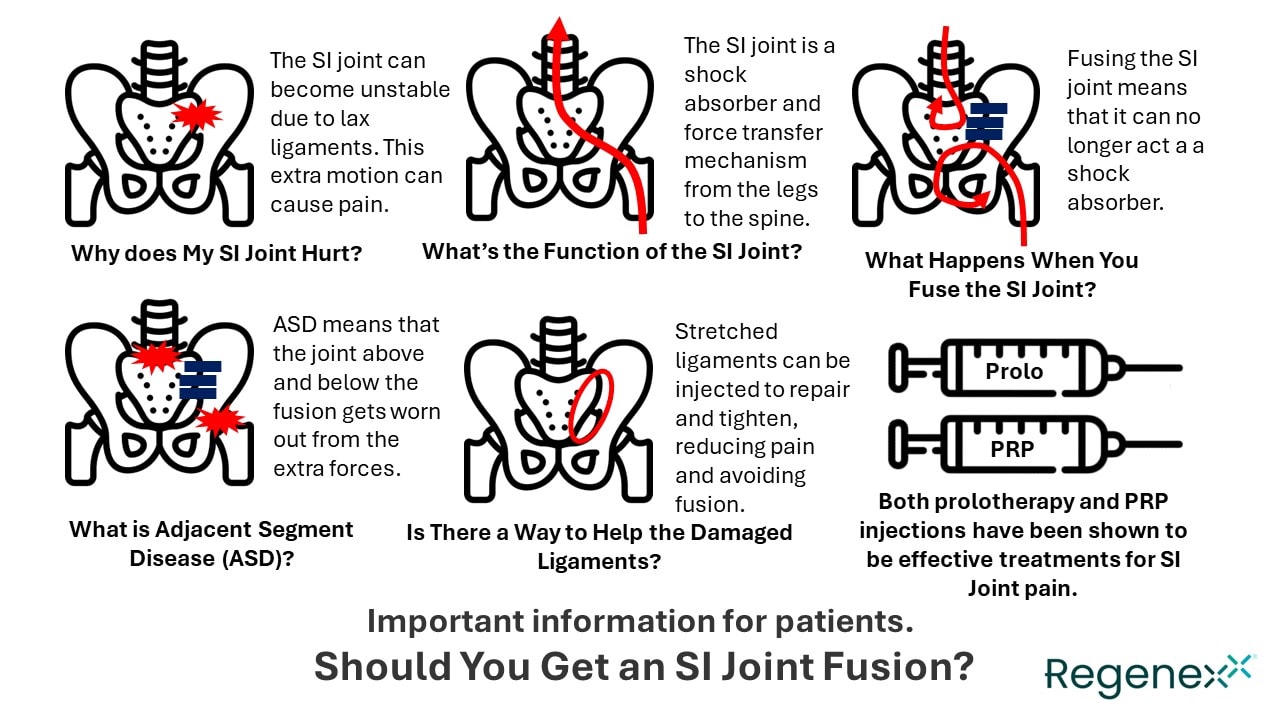
The SI joint is short for the sacroiliac joint, which lives between the hip joint and the lower back in the pelvis. It’s a critical shock absorber that transfers forces that come up from the leg and travel down the spine. It doesn’t move like a hip or knee but instead “gives” as you walk, run, or twist.
Tough ligaments hold the SI joint together and can become unstable when its ligaments get stretched out. This can happen due to injury or simply in pregnancy as the baby’s head traverses the birth canal in the pelvis. SI joint instability can be miserable in that the joint itself can become painful, and any activity, such as walking, running, or even turning over in bed, can be pain-provoking. In addition, pain and or numbness down the leg is not uncommon.
The traditional treatment for SI joint pain has been either PT or manual manipulation, like chiropractic. However, for some SI joint instability patients, these treatments provide only temporary relief. The next step is often a high-dose steroid injection into the joint, usually performed by a highly trained interventional spine physician using fluoroscopy (x-ary) guidance. This, again, only usually provides temporary relief.
The SI Joint Fusion Game
The most interesting thing about SI instability is that it’s easy to fix. We’ve known for years that treatments like prolotherapy and PRP are very effective (6-8). For example, in my career, I’ve seen hundreds of these patients, with 95% returning to normal, healthy, and active lives, using simple injections into the damaged ligaments to promote healing and tightening. However, despite randomized controlled trials showing efficacy, traditional insurance plans don’t cover these simple treatments. That lack of coverage opened the door for an opportunistic and overly aggressive solution known as minimally invasive SI joint fusion.
To understand SI fusion, you need to grasp its bizarre history. In the late 90s and early 2000s, SI joint fusion, as performed by spine surgeons, was gaining steam and momentum. These procedures, usually placing screws or plates across the SI joint, caused it to be fixed and not to move or give. These surgeries’ results were generally considered poor, as the forces that the flexible SI joint should have absorbed now bombarded the lower back and hip. Hence, by around 2005 or so, the procedure fell out of favor.
Despite the first failure of SI joint fusion as a procedure, the business plan for spine hardware companies makes these ventures some of the most profitable businesses in healthcare. For example, unlike a pharma drug company that spends hundreds of millions on FDA approval for a substance, these companies can pursue a 510K FDA device clearance pathway that costs 1/100th of getting a drug approved. These screws, plates, and other devices cost tens or hundreds of dollars to produce and then can be sold to insurance companies for thousands of dollars. Basically, in the case of SI fusion, you’re taking a titanium screw that you can buy on Amazon right now for $10, custom manufacturing it in Vietnam, China, or India for $50, and selling it for thousands.
It is because of this crazy profitability that SI fusion didn’t stay down for long. However, the screw manufacturers had a problem. Most surgeons in practice remembered or had heard about the disastrous SI joint fusions of the turn of the 21st century, so interest among spine surgeons wasn’t high. That problem, however, could be solved by targeting a new breed of physicians who were increasingly getting into quasi-surgical procedures. This was the specialty of interventional pain management.
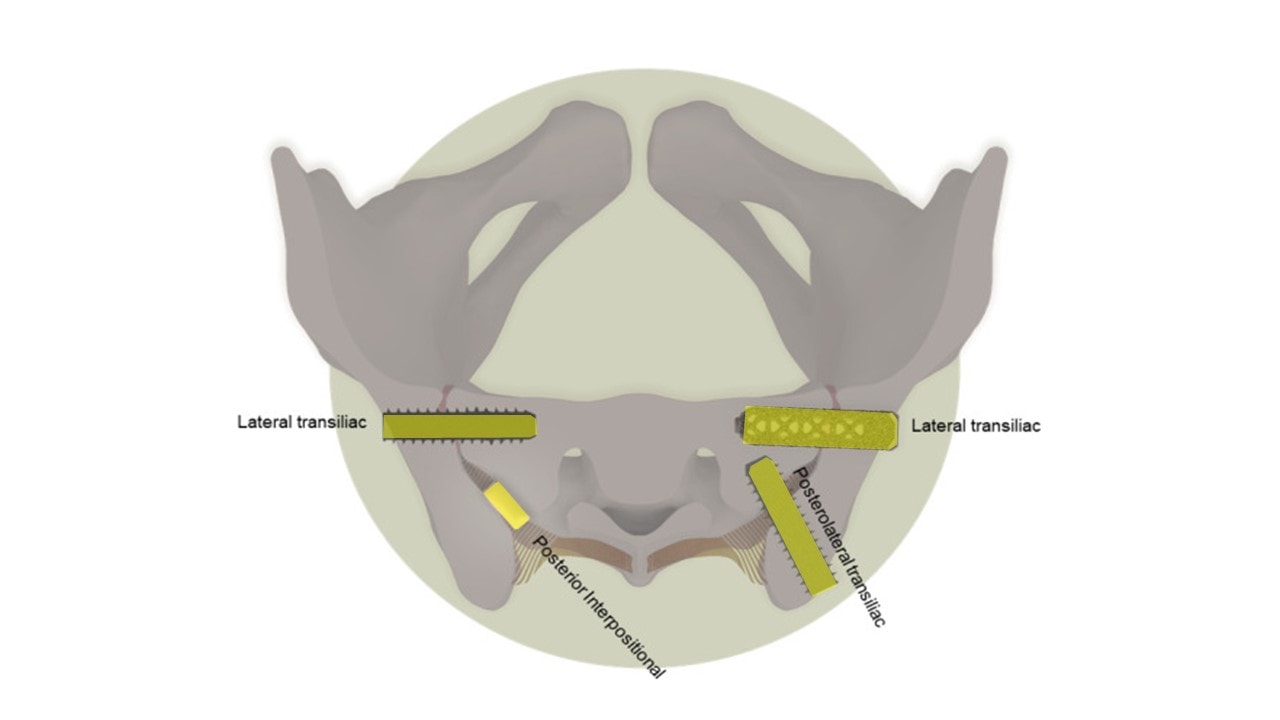
As a result of the confluence of these factors, “minimally invasive” Si joint fusion was born. These device companies invented tools that could place these screws without major open spine surgery, just using a few small incisions and x-ray guidance to seat them across the SI joint. Above is a diagram of the pelvis. Note that the yellow screws and dowels represent the many different types of SI joint fusion devices on the market, now being sold by about a dozen companies.
There was another reason that IPM physicians were interested in SI fusion. Severe reimbursement cuts were battering their traditional procedures, so the specialty sought a flight to reimbursement safety. Basically, per unit time, doctors could make 2-4X for performing an SI fusion over another procedure like an epidural. In addition, these physicians were often owners or part-owners of surgery centers, which could also collect much higher facility fees for SI fusion. Finally, with high-profit margins, SI fusion screw manufacturers could afford to throw gobs of trips, dinners, and other benefits toward IPM physicians.
The Problems with SI Fusion
So did the laws of physics change since the 90s when SI fusion was popular? Nope. Fusing the SI joint is still the same whether it’s done with open surgery or through a small incision. Let’s look next at the complication rates and outcomes for these procedures.
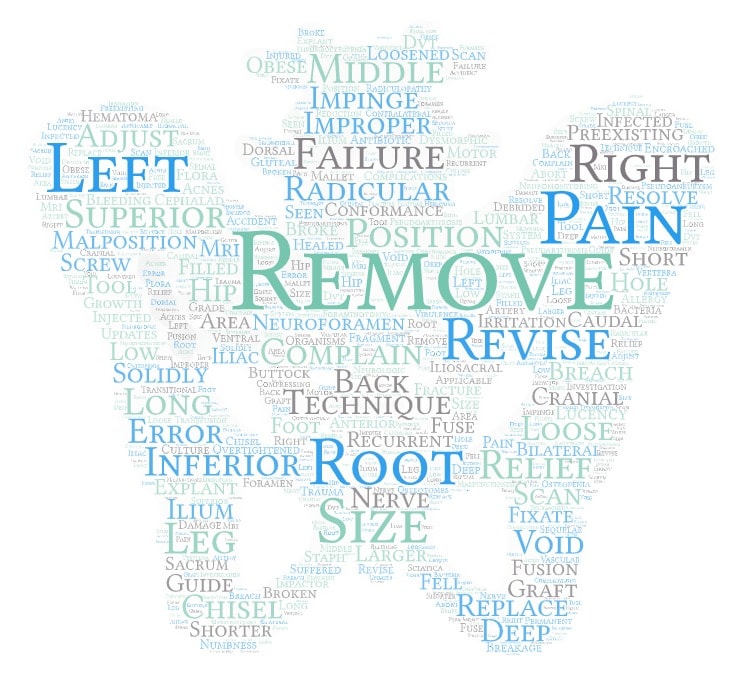
As I have previously blogged, the complication rates are high if you remove the device manufacturer-sponsored trials and focus on independent reviews of this procedure. For example, the 5% of complications reported by one manufacturer ballooned to 16% in a study of healthcare insurance claims (1). In addition, we know that adjacent segment disease is a problem with any spinal fusion (2-5). This means that the forces that the fused segment should have handled get thrown to adjacent healthy segments, and these get worn out in most patients, requiring more surgery in the future to fuse these segments. Hence, it’s almost certain that these SI fusions will wear out hip joints and low back levels as time passes. Finally, I have collected the phrases (shown above) in an FDA database with more than a thousand reported complications. The word’s size represents the word’s frequency in these reports. This speaks for itself.
Does SI fusion work? It depends heavily on how you define that term. For example, in one industry-sponsored study, 70% of the patients who were taking opioids and had an SI fusion continued to take opioids (9). Not exactly a ringing endorsement. Perhaps this quote from a recent review article sums up the state of the SI joint fusion outcomes literature:
“Although outcomes have been widely studied, more studies, especially prospectively designed and those without industry influence, be performed to elucidate the optimal management of patients with intractable SIJ pain.”
The Decision Matrix that We Should Have Versus the One We Do Have
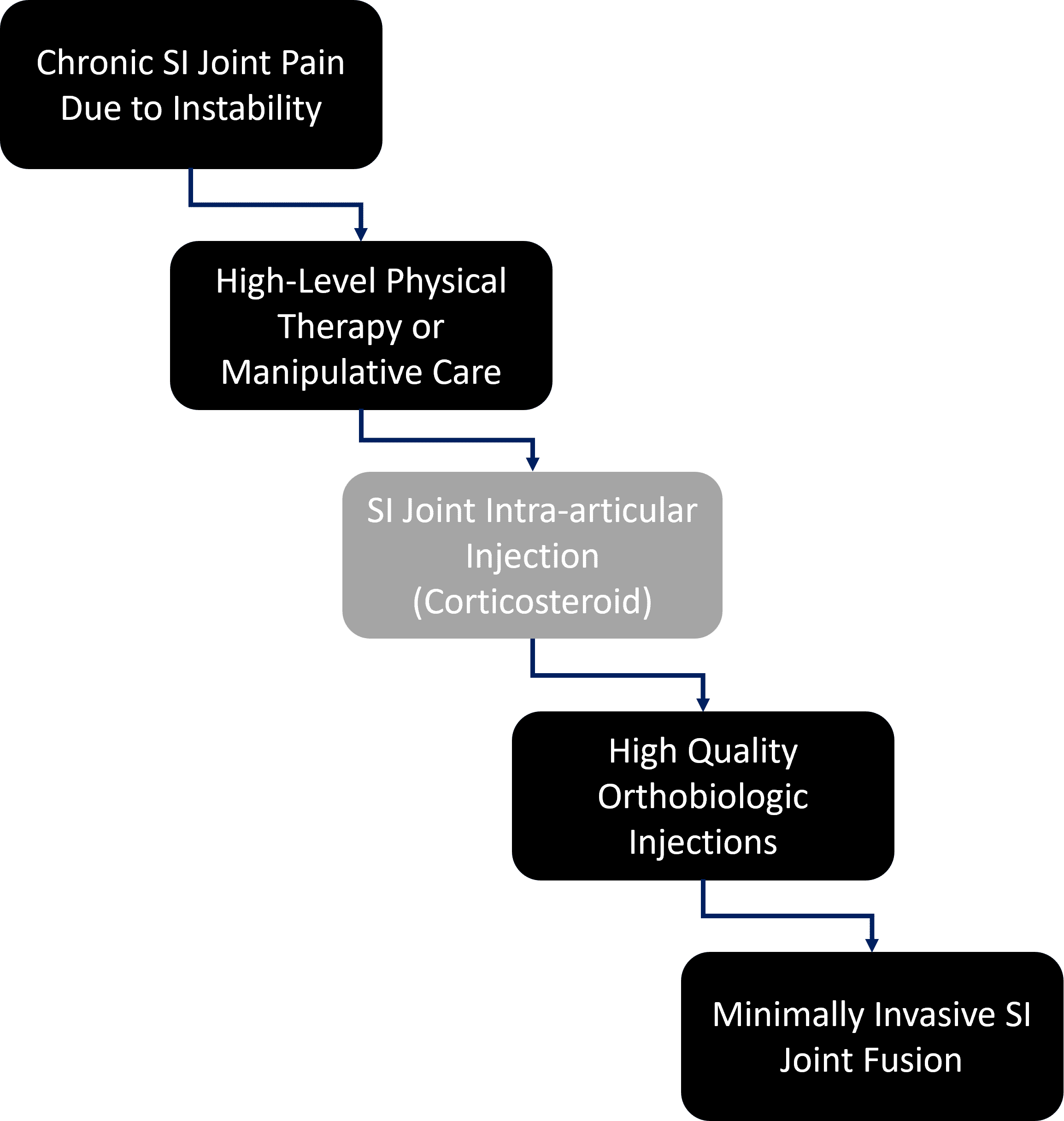
The decision matrix above makes sense. You end up starting with conservative care and moving toward a simple SI joint injection. If none of this works, you target the ligaments and try to heal them with orthobiologics. In my experience, this will leave very few patients getting SI Joint Fusion. So if we begin with 100 patients who begin PT/chiropractic who have serious disability due to an SI joint problem, we end up with 50 getting a steroid shot in the joint and likely 25 who end up getting orthobiologics and only one patient getting fusion.
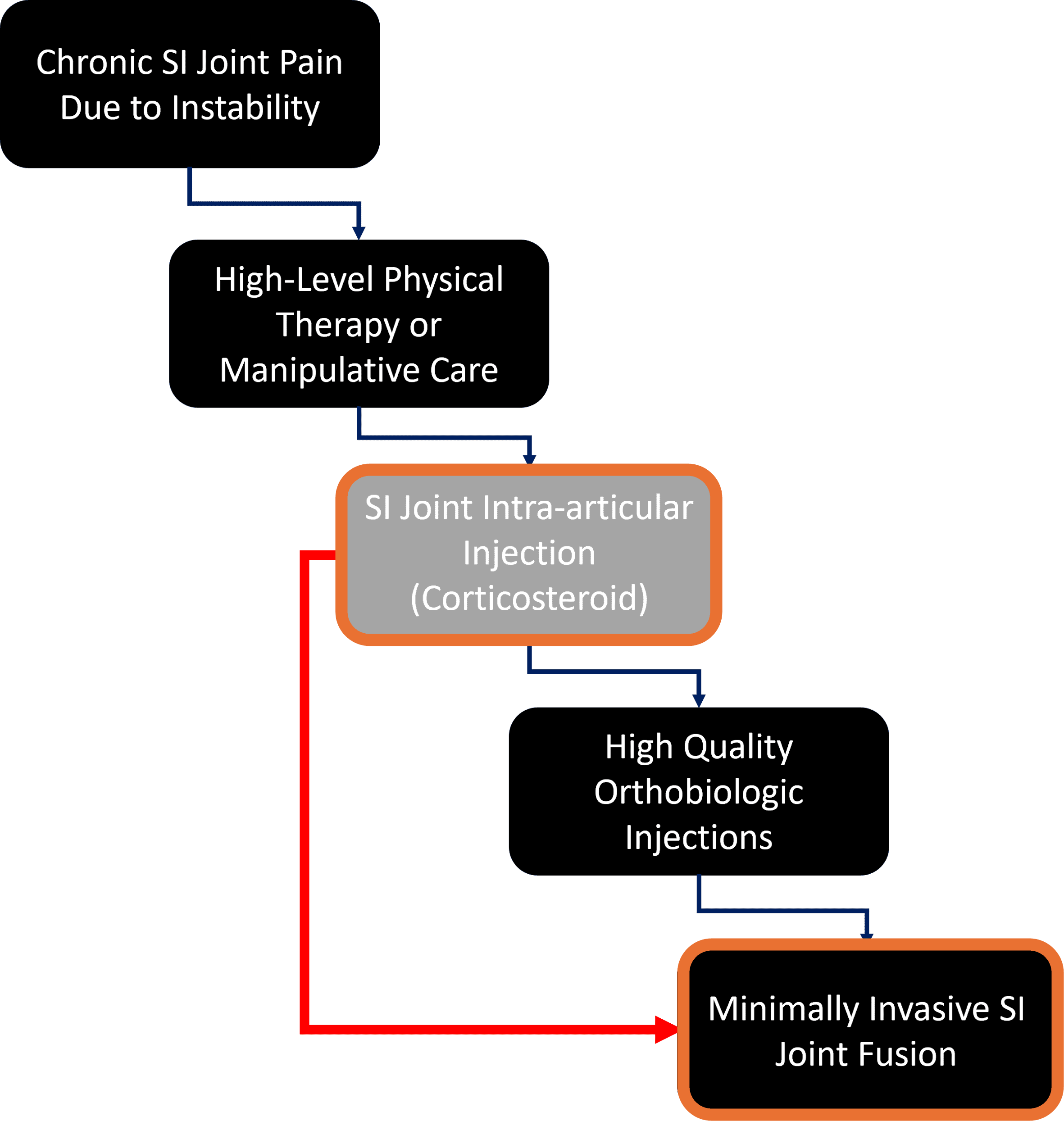
Above is what’s actually happening to insurers and employers who are footing these bills. The patients aren’t being offered orthobiologics, so in general, all 25 out of our initial 100 are getting SI fusion. Why? Because insurers won’t cover orthobiologics, and providers don’t want to go through the hassle of charging the patient, even if it means their patients will get more invasive care with more complications.
Why SI Fusion is Emblematic of Cost Containment Failures
So, who is SI fusion good for? The patients? No, because far simpler and less invasive procedures can usually solve 95% of the SI instability cases out there. The complication rates of those procedures are almost zero and cost much less. The insurance company or employer? No, because SI fusion, when you consider the cost of the procedure, the screws, anesthesia, facility fees, complication costs, and other expenses, is far more expensive.
However, SI fusion benefits:
- IPM physicians, through increased reimbursement for the procedure and facility fee
- Hospitals by moving patients from simple outpatient office procedures to more expensive hospital-owned ASC procedures
- Device manufacturers who get to sell a $50 screw for thousands of dollars
Hence, it’s not hard to see why SI fusion is exploding nationally and why it’s emblematic of why cost containment fails. Bundling the costs of SI fusion won’t solve the main issue of patients being moved from less costly office-based injections to invasive surgeries. Capitation also won’t solve this problem because health plans don’t traditionally cover the better solutions for this problem.
Common Sense Healthcare
How does Regenexx solve this problem? By extending orthobiologics coverage to self-funded health plans, Regenexx fills this gap by covering the less invasive solutions for these patients. In addition, we ensure that the right patients get these treatments through prior authorization and physician training certification. Regenexx also sets the protocols and injectates for these orthobiologic procedures.
In other words, Regenexx substitutes less invasive care that can solve the problem with less cost and complications.
The Lessons of SI Joint Fusion for Health Plans Trying to Control Costs
What can a healthcare plan or cost-containment company learn from SI fusion? First, in a world where medicine continually reinvents itself to bypass all cost-containment measures, bundling and capitation will never work. Both can be easily circumvented with new procedures, devices, and drugs. The only cost solution that will work is to look at the cost/outcome of procedure A versus procedure B. All too often in healthcare, there are clear winners when these comparisons are made.
Even in situations where insurers can chose A as being more cost-effective than B, they have another problem-provider buy-in. Providers often do what makes them the most money. In the case of Regenexx, we can take providers performing these less-invasive SI instability procedures and allow them to get reimbursed by a self-funded plan, aligning incentives between the provider and employer. The providers win because of high insurance reimbursement for a procedure that saves the employer money.
The upshot? SI Joint Fusion shows why cost containment often fails. Providers, hospitals, and drug and device companies will always find ways to circumvent or reinvent. However, aligning incentives for providers to deliver less invasive, high-quality care does work.
______________________________________________________
- Schoell, K., et al., Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J. 2016 Nov;16(11):1324-1332. doi: 10.1016/j.spinee.2016.06.016.
- Maruenda JI, Barrios C, Garibo F, Maruenda B. Adjacent segment degeneration and revision surgery after circumferential lumbar fusion: outcomes throughout 15 years of follow-up. Eur Spine J. 2016 May;25(5):1550-1557. doi: 10.1007/s00586-016-4469-5. Epub 2016 Mar 8. PMID: 26957098.
- Saavedra-Pozo FM, Deusdara RA, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014;14(1):78–83.
- Zhong ZM1 Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clin Neurol Neurosurg. 2017 May;156:29-34.
- Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101.
- Chen AS, Solberg J, Smith C, Chi M, Lowder R, Christolias G, Singh JR. Intraarticular Platelet Rich Plasma vs Corticosteroid Injections for Sacroiliac Joint Pain-a Double Blinded, Randomized Clinical Trial. Pain Med. 2021 Nov 24:pnab332. doi: 10.1093/pm/pnab332. Epub ahead of print. PMID: 34850180.
- Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017 Jul;17(6):782-791. doi: 10.1111/papr.12526. Epub 2016 Dec 1. PMID: 27677100.
- Kim WM, Lee HG, Jeong CW, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010 Dec;16(12):1285-90. doi: 10.1089/acm.2010.0031. PMID: 21138388.
- Polly DW, Swofford J, Whang PG, Frank CJ, Glaser JA, Limoni RP, Cher DJ, Wine KD, Sembrano JN; INSITE Study Group. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg. 2016 Aug 23;10:28. doi: 10.14444/3028. PMID: 27652199; PMCID: PMC5027818.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.