Carpal Tunnel Surgery Recovery: Does Cutting the Ligament Have Consequences?
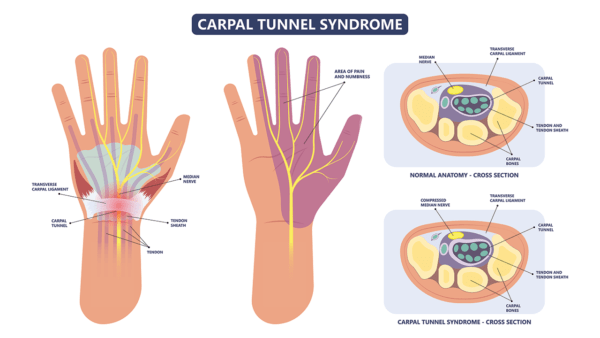
Carpal tunnel surgery has become a standard surgical treatment for carpal tunnel syndrome, a problem that occurs when the median nerve gets chronically pinched at the wrist. The surgery is simple, cut the ligament that normally covers the carpal tunnel to give the nerve more breathing room. However, does cutting the transverse carpal ligament (TCL) impact carpal tunnel surgery recovery? Does it have other long term consequences? Is the ligament there for a reason? Regrettably, taking the quick fix approach by cutting the ligament may have issues.
Rumruay/Shutterstock
The TCL makes up the roof of the space we call the carpal tunnel (see above). The median nerve lives in that tunnel. The ligament plays an important role is stabilizing all of those little bones (carpals) in the wrist. It also serves as an anchor for several important hand muscles (including the one on the meaty part of the thumb). It also acts like a pulley that helps the tendons that flex your fingers get better mechanical advantage. So what happens if we cut it during a carpal tunnel release surgery? Let’s see what the research literature says.
As early as the late 80s, it became clear that cutting the TCL made the carpal bones of the wrists more unstable. However, in this early study, the instability increase was noted to be only 7% (the paper doesn’t include a way to determine if this is a lot or a little). By the mid 90s, researchers noted that cutting the TCL shortened and weakened the hand muscles that anchored there. Several studies have noted that the tendons that flex your fingers move to a different location when the TCL is cut and this results in a bow stringing effect which is believed to be linked to wrist weakness. Other authors have linked this bow stringing to later development of trigger finger (see study 1, study 2). So to summarize, there is no free lunch with cutting the TCL, it has biomechanical consequences.
So while cutting the TCL has consequences, all types of carpal tunnel surgery whether they be minimally invasive, LASER, or traditional variants-cut the TCL. Is there a better way? We’ve been using nerve hydro-dissection with platelet lysate for years with very good results. This procedure uses sophisticated ultrasound imaging to inject growth factors from the patient’s own blood platelets around the median nerve. In our experience, this helps break up scar tissue around the nerve and reduces inflammation while improving blood flow. It also doesn’t involve cutting the TCL ligament or harming the biomechanics of the wrist. In addition, our Orthopedics 2.0 philosophy means that we also look for reasons why the carpal tunnel syndrome occurred in the first place. For example, we often find that irritated nerves in the neck have gone undiagnosed and are the root cause of why the nerve farther down in the wrist is running into problems.
The upshot? All types of surgical carpal tunnel approaches involve cutting the TCL ligament in the wrist. Cutting the TCL has consequences, so our approach to carpal tunnel doesn’t involve cutting the ligament, but rather trying to make the environment for the nerve healthier, releasing scar tissue through injection, and figuring out why the nerve is in trouble in the first place!
Note: The data for this literature review was supplied by Regenexx network provider Gerry Malanga, M.D. of New Jersey Sports Medicine.
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.