SI Joint Fusion Complications? Why Are We Doing this to Patients?
One of the biggest issues I see is how easily interventional pain physicians have been lured in by quasi-spine surgeries that they know are bad for their patients. A case in point is SI fusion. Let’s dig into SI joint fusion complications through a case posted on LinkedIn.
What Is the SI Joint?
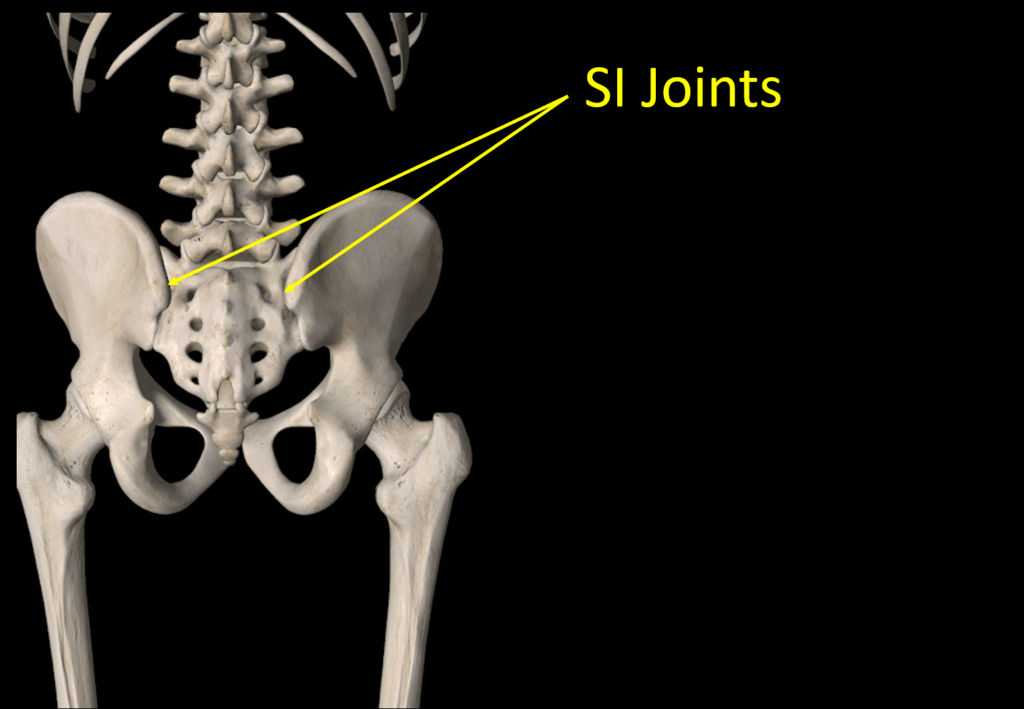
The acronym SI stands for “sacroiliac”. The SI joint lives between the pelvis and hip as shown above. It’s a joint like any other in your body. Its main function is as a force transfer between your legs and spine.
SI Joint Ligaments and Instability
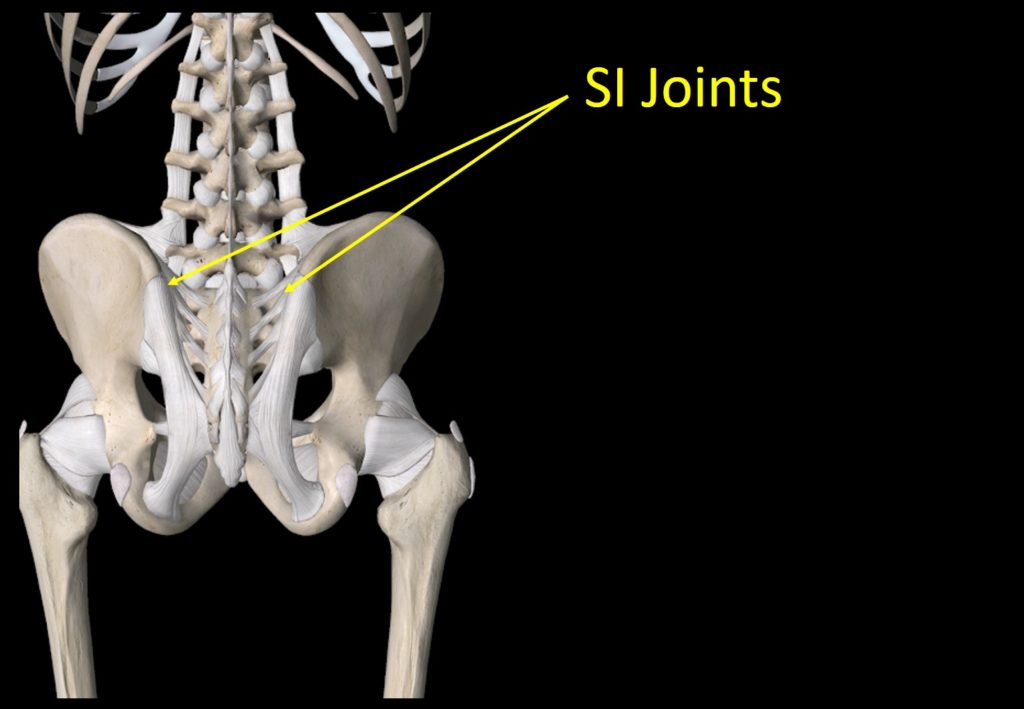
The SI ligaments are shown above in white. This is a robust complex of ligaments that help to transfer that force as described above. The ligaments can get damaged by things like car crash trauma, falls on the butt, or other injuries. When they do, the joint becomes unstable, meaning it moves too much. This can cause local pain in the SI joint area as well as radiating pain down the leg. Some patients also report that their leg gives out.
What Is SI Fusion?
If the SI joint is unstable, some interventional pain physicians and surgeons are now advocating that the patient should have their joint fused. This means an invasive procedure where the joint is bolted together so it doesn’t move. This procedure used to be pretty popular in the 90s but was abandoned due to SI joint fusion complications. Recently it has had a resurgence as companies line up to make screws and hardware.
Why the Resurgence?
If SI fusion was big in the 90s and fell out of favor due to poor results and complications, why is it back? These newer systems allow a doctor to place a screw through the joint without surgery. IMHO the real reason the idea is back is money. Meaning a screw that’s made for tens of dollars in some low-wage country can be resold for $1,000+ when placed through an SI joint here in the U.S.
What Are SI Joint Fusion Complications?
These are the main SI Joint fusion complications:
- Adjacent Segment Disease
- Misplaced screws
- Fracture of the bone
- Infection
The SI joint was built to move. It absorbs shock and moves slightly this way and that, acting as the main force coupling between your leg and spine. If we fuse that joint, the forces then increase on the hip and the spine. Meaning that the patient will be more likely to develop hip and L5-S1 spinal problems. This concept is called ASD or Adjacent Segment Disease. See my video below for more information on ASD:
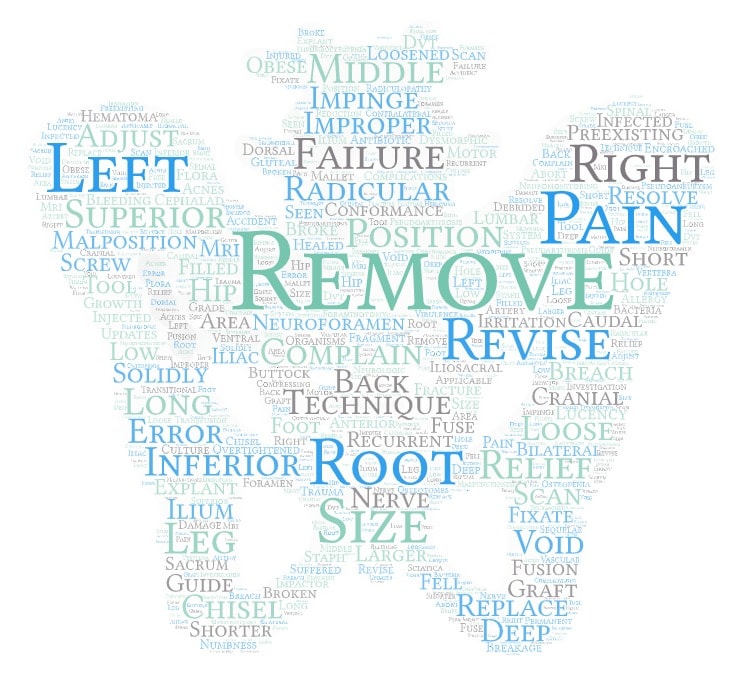
Misplaced screws are also an issue. For example, I recently pulled the FDA complications reporting database for one of the more common SI Joint fusion devices and found many reports of these screws being placed through the sacral spinal nerves. If that happens, the patient may lose bowel or bladder control. Here’s a word cloud of those SI joint fusion complications:
On fracture of the bone, we’ll cover that one below. Infection is always a possible problem with any surgery that implants something into the body. Another issue is that this is a one-way street procedure. Meaning, once you put a screw through the SI joint, it destroys the joint. There is no way to back that screw out and have the joint function normally if this doesn’t work.
The Most Recent SI Fusion Complications
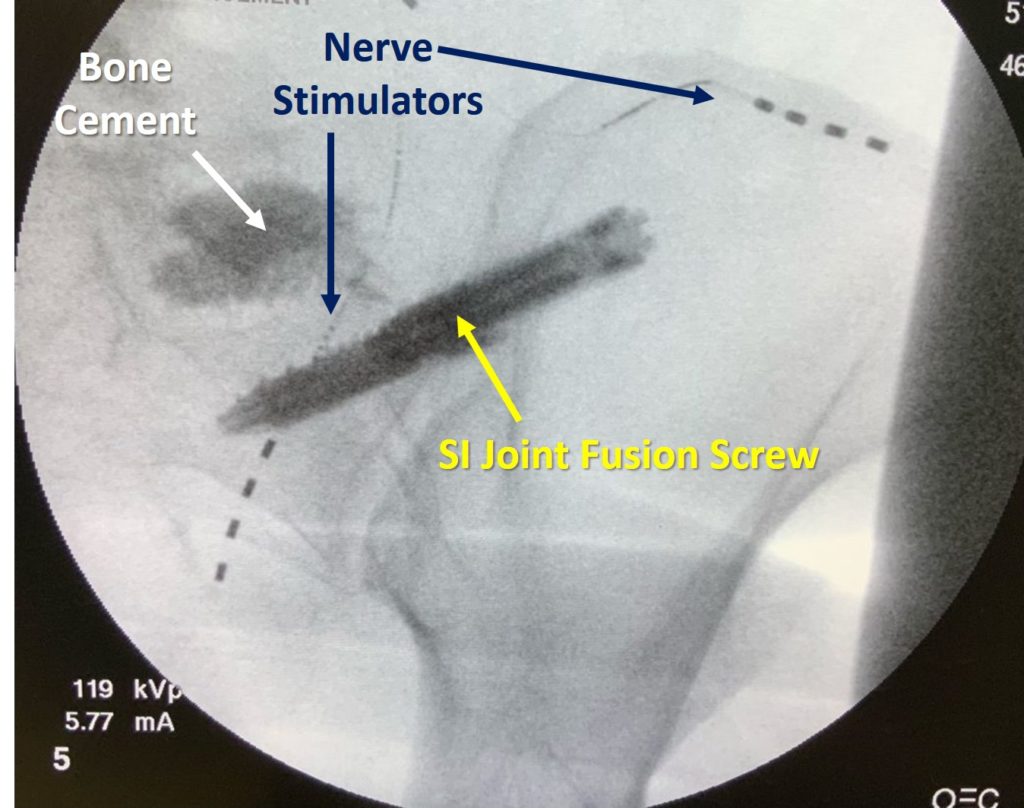
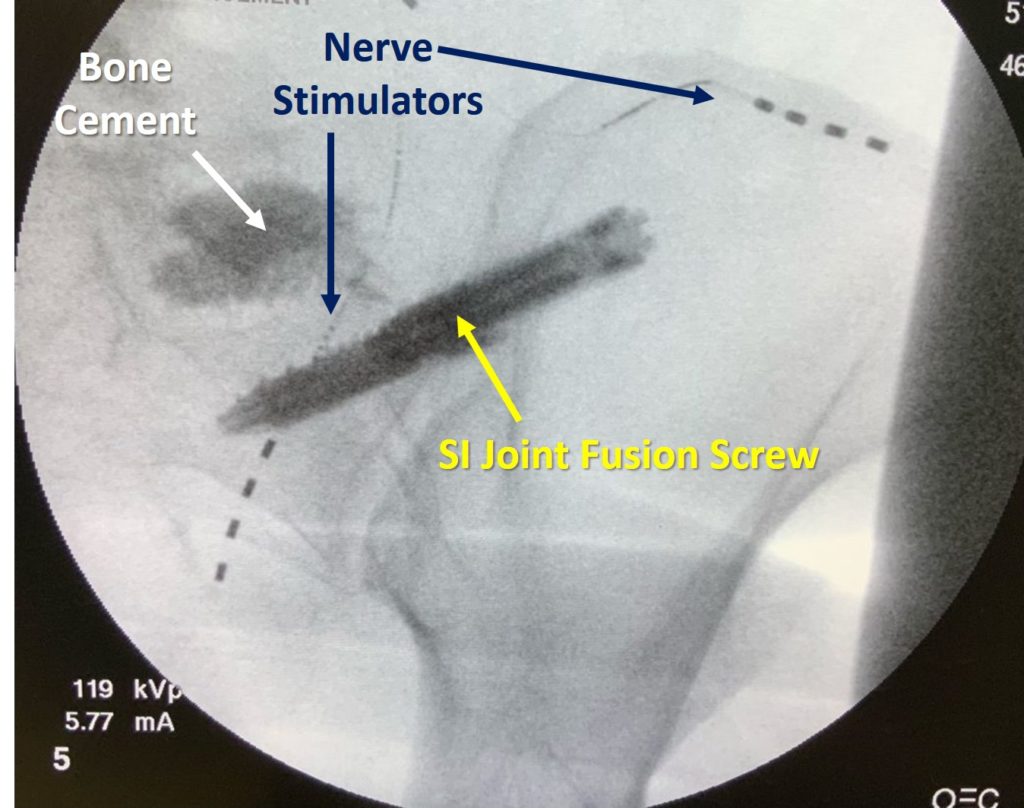
The SI joint x-ray above represents one patient’s story of SI joint fusion complications. This is a 56-year-old patient who had an SI joint fusion screw placed (Sacrix), which is shown above in yellow. That screw then caused a fracture in the sacrum, so the second procedure was bone cement, which was injected into the fracture area (white). The patient was then left with chronic pain, so that then caused the need for the third procedure, which was a nerve stimulator being placed (Navy blue points to the leads).
So what began as an SI fusion caused three procedures. Realize that the nerve stimulator is not a permanent fix, those leads will have to be replaced at some point. All that does is block the chronic pain caused by the SI joint fusion. So this patient replaced one chronic problem with now several others.
Why Are We Doing This to Patients?
How can we eliminate SI joint fusion complications? Based on my direct experience treating hundreds of SI joint instability patients, there are MANY options that don’t involve surgery. Image-guided prolotherapy works in many patients. These are injections to cause a brief inflammatory healing and tightening response in the damaged ligaments. Precise image-guided orthobiologic injections can be even more effective. To learn more about common orthobiolo0gic injectates, see my video below:
So how many patients out of 100, in my direct experience, will fail these much more elegant therapies that induce healing? Only a handful. However, how many patients who get SI fusion are trying these very effective injections? Not many. So why are doctors banging screws through and destroying SI joints before injecting SI joints with things that can heal ligaments? Money. Some insurance companies cover SI joint fusion and the healing injections are usually not covered.
Don’t physicians have a moral responsibility to push patients toward the least invasive care that’s likely to work? Even if that’s not covered by insurance? Yes, but regrettably many physicians are allowing patients to skip less invasive care that might cure their issue.
The upshot? Si Joint fusion is an incredibly invasive way to fix SI joint instability that can usually be fixed with much less invasive injections. So why are we doing this to patients?
If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.