Masking, COVID, and a New Cochrane Study

Our pandemic response was a dismal failure. No single issue shows that more than the idea that wearing a mask would decrease the spread of this disease. Now a new Cochrane analysis shows us how futile this was and also highlights how our public health leaders failed to follow the science.
Masking Pre-COVID
For anyone following the science of masking, multiple world governments had looked at the issue of masking up populations to reduce the spread of respiratory viruses way before the pandemic. They all had concluded that this was a fool’s errand. Meaning that the science didn’t support that it helped reduce the spread of common respiratory viruses. Why?
Any healthcare worker that has had to wear a surgical mask and glasses can tell you why asking an entire population to mask will never work. That’s because there are serious amounts of unfiltered airflow that escape above and below the mask. High-quality N-95 masks are different, but they’re also very uncomfortable and have to be fit to your face and tested. Meaning that no US hospital that requires N-95s allows a person to just throw on a mask without testing its seal. KN-95 masks share both problems is that they also have airflow around teh seal even worse than just throwing on an American-made 3M N-95.
Understanding the Levels of Medical Evidence
There are various levels of research quality in medical evidence with multiple grading scales (16). Below I have listed the levels 1-10 for convenience:
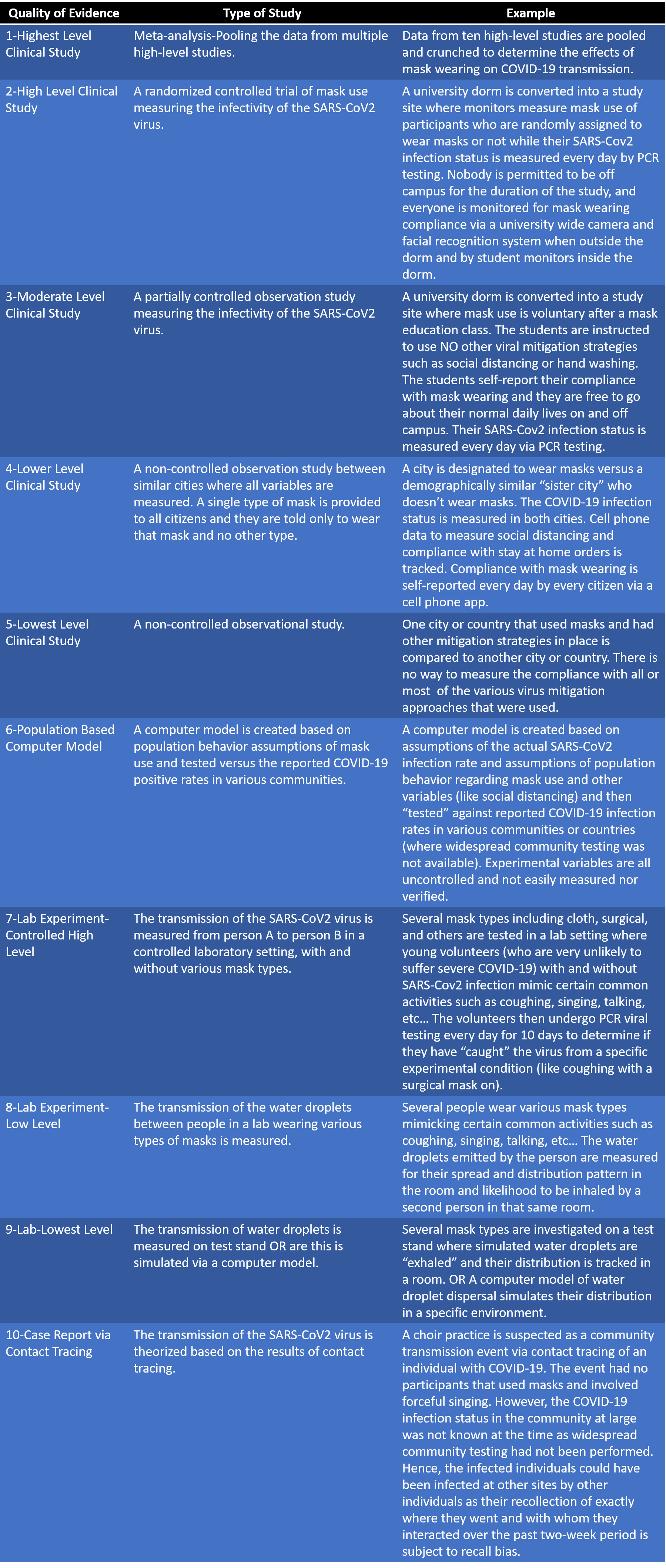
Studies that meet the level 1 or 2 bar are considered authoritative.
Here is the quality of the respiratory mask studies that I graphed as of the beginning of the 2020 pandemic when we were instructed to mask (2-14):
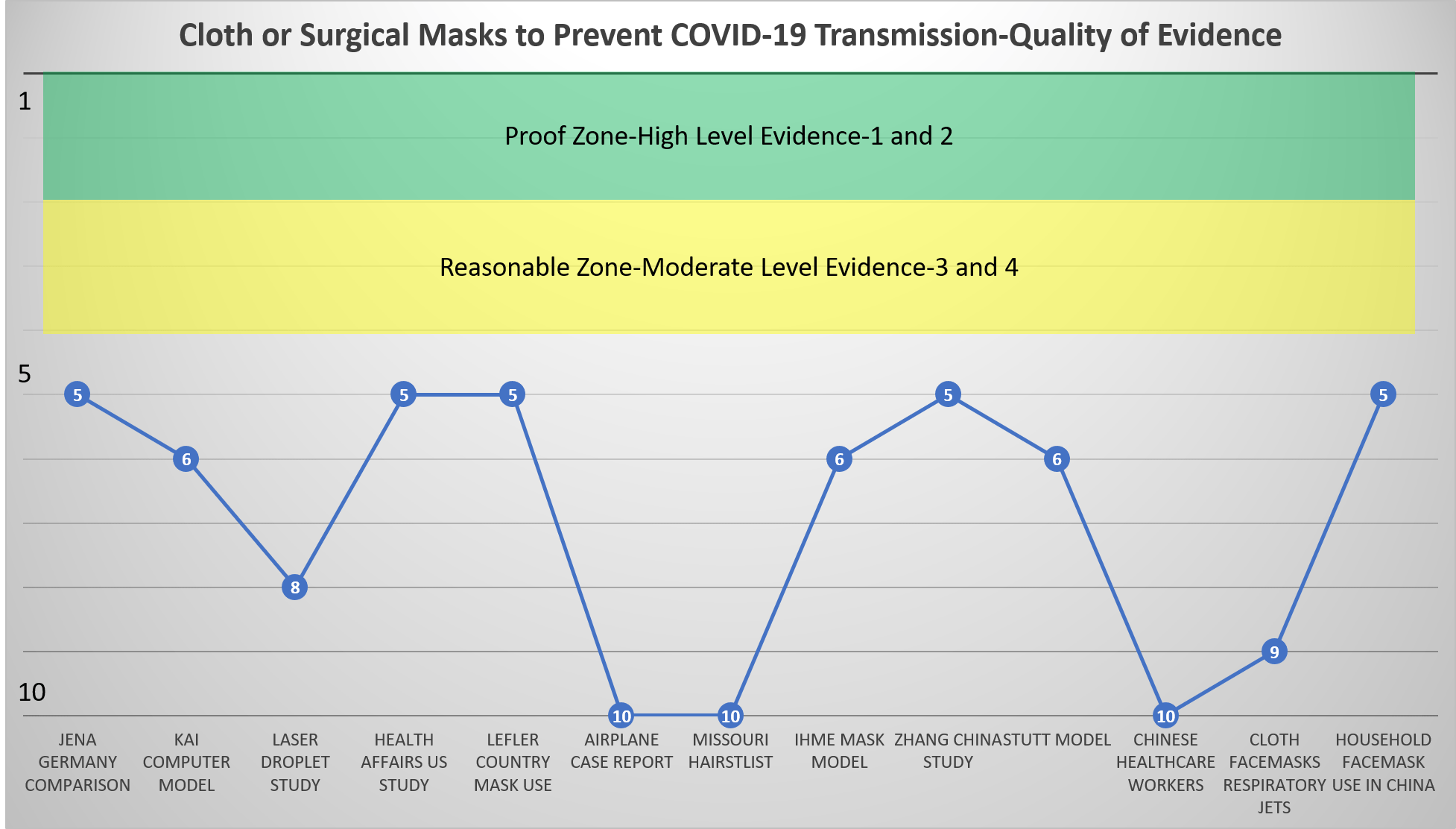
As you can see, despite being told to mask, there was little strong data back then to suggest that masking a population would help reduce the spread of a respiratory virus.
The New Cochrane Study
Cochrane studies are usually the highest level of evidence we have available or “Level 1” as shown above. This research group just looked at all of the masking studies we had for both reducing the spread of respiratory viruses and the SARS-Cov2 virus (1). They pulled apart the data from multiple studies and pooled it, which is called a meta-analysis. What did they find?
This is from their page:
“Medical or surgical masks
Ten studies took place in the community, and two studies in healthcare workers. Compared with wearing no mask in the community studies only, wearing a mask may make little to no difference in how many people caught a flu-like illness/COVID-like illness (9 studies; 276,917 people); and probably makes little or no difference in how many people have flu/COVID confirmed by a laboratory test (6 studies; 13,919 people). Unwanted effects were rarely reported; discomfort was mentioned.
N95/P2 respirators
Four studies were in healthcare workers, and one small study was in the community. Compared with wearing medical or surgical masks, wearing N95/P2 respirators probably makes little to no difference in how many people have confirmed flu (5 studies; 8407 people); and may make little to no difference in how many people catch a flu-like illness (5 studies; 8407 people), or respiratory illness (3 studies; 7799 people). Unwanted effects were not well-reported; discomfort was mentioned.
Hand hygiene
Following a hand hygiene programme may reduce the number of people who catch a respiratory or flu-like illness, or have confirmed flu, compared with people not following such a programme (19 studies; 71,210 people), although this effect was not confirmed as statistically significant reduction when ILI and laboratory-confirmed ILI were analysed separately. Few studies measured unwanted effects; skin irritation in people using hand sanitiser was mentioned.”
Basically, wearing that surgical mask or N-95 mask to Whole Foods doesn’t help protect you from getting COVID-19, but washing your hands frequently probably works.
How Did Public Health Officials Get this One So Wrong?
We knew very clearly before the pandemic that masking a population made no sense. No high-quality data was published during the pandemic that moved that needle. So why did our public health officials not follow the science? Remember I said a long time ago that after the pandemic was over there would be research looking at how we did as a society.
It’s now very clear that everyone got on the mask train without credible evidence (15). Heck, that was clear back in 2020. So why did this happen? Public health officials weren’t following the science, but instead an ideology.
The upshot? The science now clearly shows, as it did in 2020, that masking an entire population doesn’t help reduce the spread of a respiratory virus or reduce anyone’s risk of getting COVID-19. So let’s put a stake in the heart of this myth and throw the masks away. Do continue to wash your hands frequently.
_____________________________________________________________________________
References:
(1) Jefferson T, Dooley L, Ferroni E, Al-Ansary LA, van Driel ML, Bawazeer GA, Jones MA, Hoffmann TC, Clark J, Beller EM, Glasziou PP, Conly JM. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews 2023, Issue 1. Art. No.: CD006207. DOI: 10.1002/14651858.CD006207.pub6.
(2) Jena Germany Comparison: IZA Institute of Labor Economics. Face Masks Considerably Reduce COVID-19 Cases in Germany: A Synthetic Control Method Approach. IZA DP No. 13319, June 2020
(3) Kai Computer Model: Kai et al. Universal Masking is Urgent in the COVID-19 Pandemic: SEIR and Agent Based Models, Empirical Validation,
Policy Recommendations. Arxiv {Pre-print Server]. https://arxiv.org/pdf/2004.13553.pdf
(4) LASER Droplet Study-Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. N Engl J Med. 2020;382(21):2061-2063. doi:10.1056/NEJMc2007800
(5) Health Affairs US Study-Lyu W, Welby G. Community Use Of Face Masks And COVID-19: Evidence From A Natural Experiment Of State Mandates In The US. Health Affairs. https://doi.org/10.1377/hlthaff.2020.00818
(6) Lefler Country Mask Use-Leffler, Christopher & Ing, Edsel & Lykins, Joseph & Hogan, Matthew & McKeown, Craig & Grzybowski, Andrzej. (2020). Association of country-wide coronavirus mortality with demographics, testing, lockdowns, and public wearing of masks (Update June 15, 2020). https://www.researchgate.net/publication/342198360_Association_of_country-wide_coronavirus_mortality_with_demographics_testing_lockdowns_and_public_wearing_of_masks_Update_June_15_2020 Accessed 7/11/20.
(7) Airplane Case Report-Schwartz K, et al. Lack of COVID-19 transmission on an international flight. CMAJ April 14, 2020 192 (15) E410; DOI: https://doi.org/10.1503/cmaj.75015
(8) Missouri Hairstylist-Washington Post. The Outbreak that Didn’t Happen: Masks Credited with Preventing Coronavirus Spread Inside a Missouri Hair Salon. https://www.washingtonpost.com/business/2020/06/17/masks-salons-missouri/ Accessed 7/11/20.
(9) IHME Mask Model-University of Washington. The Institute for Health Metrics and Evaluation. New IHME COVID-19 Model Projects Nearly 180,000 US Deaths. http://www.healthdata.org/news-release/new-ihme-covid-19-model-projects-nearly-180000-us-deaths. Accessed 7/11/20.
(10) Zhang China Study-Renyi Zhang, Yixin Li, Annie L. Zhang, Yuan Wang, Mario J. Molina. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences, 2020; 202009637 DOI: 10.1073/pnas.2009637117
(11) Stutt Model-Stutt R, et al. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’ in managing the COVID-19 pandemic. Proceedings of the Royal Society A. 10 June 2020https://doi.org/10.1098/rspa.2020.0376
(12) Chinese Healthcare Workers-Ng K, Poon BH, Kiat Puar TH, et al. COVID-19 and the Risk to Health Care Workers: A Case Report. Ann Intern Med. 2020;172(11):766-767. doi:10.7326/L20-0175
(13) Cloth Facemasks Respiratory Jets-Verma S, Dhanak M, Frankenfield J. Visualizing the effectiveness of face masks in obstructing respiratory jets. Phys Fluids (1994). 2020;32(6):061708. doi:10.1063/5.0016018
(14) Household Facemask Use in China-Wang Y, Tian H, Zhang L, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, ChinaBMJ Global Health 2020;5:e002794.
(15) University of California San Francisco. Still Confused About Masks? Here’s the Science Behind How Face Masks Prevent Coronavirus. https://www.ucsf.edu/news/2020/06/417906/still-confused-about-masks-heres-science-behind-how-face-masks-prevent. Accessed 7/11/20.
(16) The University of Oxford. Oxford Centre for Evidence-based Medicine – Levels of Evidence (March 2009). https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ Accessed 7/11/20.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
