Bone Marrow Lesions: Causes, Symptoms And Treatment Options

Medically Reviewed By:
Joint pain can affect daily activities and may indicate underlying structural concerns. One condition that may be identified through medical imaging is a bone marrow lesion (BML). These lesions can develop due to various causes and are frequently associated with joint-related conditions.
Understanding the causes, symptoms, and available treatment options for BML is crucial for addressing discomfort and maintaining joint health. The following guide explores the common causes, symptoms, and treatment approaches for BMLs to help individuals manage their joint health.
What Is A Bone Marrow Lesion?
Joints, such as the knee, consist of multiple structures that work together, including bone, cartilage, ligaments, and synovial fluid. These tissues interact by exchanging cells and biochemical signals. When cartilage is damaged, it may also affect the underlying bone, and vice versa.
Changes within the bone that can be detected through MRI imaging are sometimes referred to as “bone marrow edema” or “bone marrow lesions.” On water-sensitive MRI sequences (such as T2 or Fat Sat), a BML appears as a bright area, while other sequences may show it as a darker region.
In some cases, a BML may be an early indication that the cartilage in that area is compromised. If left alone, the cartilage often degrades at that spot, and the BML may result in the death of the bone, also known as a bone cyst. If a BML is identified on a knee MRI, early intervention with platelet-rich plasma treatments or bone marrow concentrate injections is recommended, followed by a repeat MRI.
Different Categories Of Bone Conditions
BMLs can be categorized based on their severity and underlying causes. Understanding these classifications helps guide treatment and management decisions. Below are the primary categories commonly used to classify BMLs.
Category I
Category I BMLs are often linked to early-stage joint changes. These lesions may develop due to minor trauma or increased stress on the bone and are commonly observed in individuals with mild osteoarthritis or those recovering from minor joint injuries. Early intervention at this stage may help support joint function over time.
Category II
Category II lesions are moderate in severity and often associated with more advanced joint changes. These lesions may indicate increased bone stress or inflammation, which can occur in individuals with moderate to severe osteoarthritis or after repeated joint injuries. Individuals with Category II lesions may experience increased joint pain and discomfort, requiring more focused treatment to address both the lesion and the underlying condition.
Category III
Category III BMLs represent the most severe cases and are usually associated with advanced joint degeneration or major injuries. These lesions often occur with severe osteoarthritis, significant trauma, or conditions that affect bone integrity.
Addressing Category III lesions typically involves more intensive interventions, potentially including surgical options or interventional orthopedics, which could include procedures using Regenexx lab processes to support joint function.
Why Are Knee Bone Marrow Lesions A Big Deal?
Untreated knee BMLs can significantly impact joint health and long-term mobility. These lesions are often early indicators of underlying joint problems, such as osteoarthritis or injury-related stress. If left unaddressed, they may contribute to progressive joint deterioration over time.
BMLs in the knee may be associated with pain, swelling, and inflammation, restricting movement and negatively affecting quality of life. Over time, ongoing stress on the knee joint can worsen cartilage damage, which in some cases can lead to changes in joint mechanics, possibly requiring surgical interventions, such as knee replacement.
Persistent knee pain from BMLs can also limit physical activity, further weakening the muscles around the joint, reducing stability, and increasing the risk of future injuries.
Treating knee BMLs early is crucial for preventing these long-term issues, improving pain management, and preserving mobility. Physicians in the licensed Regenexx network may recommend treatment approaches that include procedures using Regenexx injectates to help reduce pain and improve function.
Exploring Joint Pain And Other Indicators Of Lesions In The Bone Marrow
Joint pain is the most common symptom associated with BMLs, signaling that something may be wrong within the bone or surrounding joint structures. However, pain is often accompanied by other symptoms that further impact joint health and mobility, including:
- Stiffness – Individuals with BMLs may experience stiffness in the affected joint, especially following periods of inactivity. This can make it difficult to move the joint freely and may worsen throughout the day.
- Swelling – Inflammation often accompanies BMLs, leading to visible swelling around the joint. This swelling can cause discomfort, restrict movement, and increase pressure within the joint.
- Limited range of motion: As the lesion progresses, individuals may notice a reduced range of motion in the affected joint, limiting their ability to perform everyday tasks.
Medical Conditions That Present With Bone Marrow Abnormalities
BMLs are often linked to various medical conditions that impact joint and bone health. These conditions can range from degenerative and inflammatory diseases to infections and trauma. Understanding these associated conditions is essential for diagnosing and treating BMLs.
Degenerative Arthritis
Degenerative arthritis, commonly known as osteoarthritis, is a leading cause of BMLs. As the cartilage in the joint wears away, increased stress is placed on the bones, leading to lesions that contribute to joint pain and mobility issues.
Inflammatory Arthritis
Inflammatory arthritis occurs when the immune system attacks the joints, causing inflammation and damage to the bone and surrounding tissues, including bone marrow.
- Rheumatoid arthritis (RA): This autoimmune disease leads to chronic inflammation, potentially resulting in bone marrow abnormalities and contributing to joint pain and deformity over time.
- Ankylosing spondylitis: Primarily affecting the spine, this form of arthritis can cause inflammation that spreads to other joints, potentially leading to BMLs.
- Psoriatic arthritis: Associated with psoriasis, this condition leads to inflammation in the joints, causing damage to both bone and cartilage, potentially resulting in BMLs.
Metabolic Arthritis
Metabolic conditions, like gout, can also lead to BMLs due to the accumulation of crystals in the joints, causing inflammation and bone damage.
- Gout: Caused by a buildup of uric acid crystals in the joints, gout leads to acute pain, swelling, and bone abnormalities over time.
Bone And Joint Infections
Infections in the bone or joint can cause significant bone marrow abnormalities as the body responds to the infection with inflammation, causing damage to bone tissue.
- Osteomyelitis: A bone infection that causes bone marrow inflammation, potentially leading to long-term damage if untreated.
- Septic arthritis: A joint infection that can cause severe inflammation and damage to both the joint and the surrounding bone marrow.
Cancer/Tumors
Certain cancers, such as bone cancer or tumors that metastasize to the bone, can cause BMLs. These lesions are often visible during imaging studies conducted as part of cancer diagnosis and monitoring.
Trauma
Traumatic injuries, such as fractures or bone bruises, are common causes of BMLs. These lesions result from the direct impact of stress on the bone and are often seen in athletes or individuals engaged in high physical activity.
- Stress fractures: Small cracks in the bone, often caused by overuse, can lead to bone marrow abnormalities.
- Compression fractures: Typically seen in the spine, these fractures occur when the bone is compressed, resulting in BMLs.
- Insufficiency fractures: Stress fractures occur when weakened bones are subjected to normal stress, causing abnormalities in the bone marrow.
- Bone bruises: Trauma to the bone can result in bruising, leading to lesions that may be painful and slow to heal.
- Anterior cruciate ligament (ACL) tears: An ACL tear is a partial or complete rupture of the anterior cruciate ligament in the knee, often caused by sudden twists or high-impact movements. It may lead to pain, swelling, instability, difficulty bearing weight, or changing direction.
- Knee osteoarthritis: Knee osteoarthritis occurs when the cartilage in the knee joint wears down over time, leading to pain, stiffness, swelling, and reduced mobility. Symptoms may worsen with activity, potentially affecting daily movements such as walking or climbing stairs.
Diagnostic Methods For Detecting Bone Irregularities
Detecting BMLs and other bone abnormalities involves multiple diagnostic steps. The following methods are commonly used:
- Physical examination: A physician evaluates the joint or bone through a physical exam, assessing range of motion, swelling, tenderness, pain, and joint stability. This helps guide further testing.
- MRI (magnetic resonance imaging): MRI is highly useful for detecting BMLs and soft tissue issues, providing detailed images that reveal early signs of bone damage, inflammation, and marrow abnormalities.
- X-rays: While less sensitive to BML, X-rays assess bone structure and can detect fractures, bone spurs, or joint degeneration.
- CT (computed tomography) scans: CT scans offer cross-sectional images of the bone, which help identify complex fractures or tumors. Though less effective than MRI for detecting marrow lesions, they provide valuable insights into other bone issues.
- Bone scan: This test detects areas of high bone activity, useful for identifying stress fractures or infections that might not be visible with other imaging methods.
- Ultrasound: Primarily used to examine soft tissues, ultrasound can help rule out other potential causes of joint pain, although it is not typically used for diagnosing BMLs.
Conventional Treatment Options
Treating BMLs usually involves a combination of non-surgical and surgical approaches to reduce pain, improve mobility, and prevent further joint damage.
- Painkillers or pain relievers: Anti-inflammatory drugs and pain relievers are commonly prescribed to manage pain and reduce swelling associated with BMLs.
- Physical therapy: Physical therapy strengthens the joint, enhances flexibility, and improves stability, which often relieves pain and improves mobility in individuals with BMLs.
- Core decompression surgery: This surgical procedure relieves pressure on the bone, improves blood flow, and promotes healing by removing a portion of the bone near the lesion.
The Regenexx Approach To Knee Bone Conditions
Physicians within the licensed Regenexx network specialize in interventional orthobiologics, offering treatment options such as bone marrow concentrate injections to treat knee bone conditions. The Regenexx approach uses interventional orthobiologics to support the body’s natural repair process and joint health.
Each procedure is customized to the individual’s specific needs and guided by imaging for precise application. Supported by extensive research, the Regenexx approach offers an alternative to surgery and prescription medications like opioids.
Case Study: A BML Patient Story
A high school basketball player sustained a hard fall on his right knee in 2017, leading to swelling and pain during activity. Rest, ice, NSAIDs, and physical therapy provided no improvement. An MRI revealed subchondral edema, osteochondritis dissecans, and a cartilage lesion on the lateral femoral condyle.
Despite these treatments, multiple MRIs showed that the area did not heal, and the patient’s pain worsened during physical activity. Dr. Markle, a physician in the licensed Regenexx network in Colorado, performed a precise bone marrow concentrate injection, guided by X-ray, targeting the BML and joint.
Before and after images (shown below) indicate healing in the affected area, with the patient experiencing improved physical recovery.
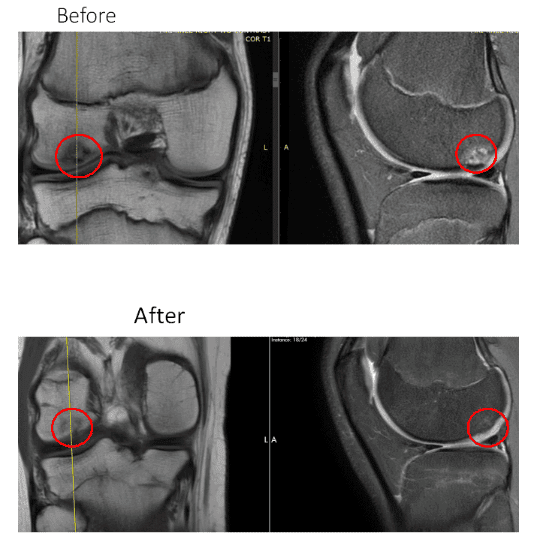
In the two before images shown above, the red circles highlights a dead area in the cartilage or an advanced BML. In the after image, taken a few months post-procedure, the same area within the red circles no longer shows signs of dead bone. Instead, there is substantial healing in the bone, as indicated by the fill-in on the left coronal image and reduced white signal on the right sagittal image. The patient also experienced physical recovery.
The takeaway? BMLs are critical to understand if you suffer from chronic knee pain. Physicians in the licensed Regenexx network have been treating BMLs with advanced, targeted injections of patients’ own bone marrow concentrate into the affected areas for over a decade. These lesions can contribute to further cartilage damage if unaddressed.
Take The Next Step In Supporting Knee Function
Taking control of your knee health is an important step toward maintaining mobility and function. Physicians in the licensed Regenexx network offer interventional orthopedic procedures using Regenexx lab processes, designed to support the body’s natural repair processes and promote joint function.
These non-surgical procedures using Regenexx lab processes may help reduce discomfort and support knee health. If you are exploring options for managing knee discomfort or considering alternatives to surgery, consult with a physician in the licensed Regenexx network to determine whether a non-surgical approach may be right for you.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
