Valgus Knee: Causes, Symptoms, And Treatment Options

Medically Reviewed By:
Valgus knee, commonly known as “knock-knee,” can lead to arthritis on the outer knee. Although invasive surgery is often recommended, it may not always be necessary.
This article explores the valgus knee condition and how non-surgical approaches, including the Regenexx approach, can support physicians in helping to manage knee health.
What Is a Valgus Knee?
A valgus knee occurs when the knee joint angles inward instead of aligning straight. In severe cases, the knees may touch when standing.
Valgus knee is most common in children, typically affecting those aged 3 to 6. In most cases, the condition corrects itself naturally by age 7. However, in rare instances, it may persist into adolescence or develop later in life due to underlying diseases or conditions.
Prior surgery, such as removing the lateral meniscus after a tear, is a common cause of valgus deformity in adults. The meniscus removal can cause the knee’s outer compartment to collapse, as the meniscus acts as a natural spacer. Additionally, untreated medial collateral ligament sprains or tears can allow the inner knee bones to spread apart.

Normal Knees Vs. Knock Knees
The image below compares normal knee alignment, knock knees (valgus knees), and bow legs (varus knees). In a healthy, normal alignment, the legs remain straight, allowing the body’s weight to be evenly distributed across the knee joint, ensuring proper function and minimizing wear.
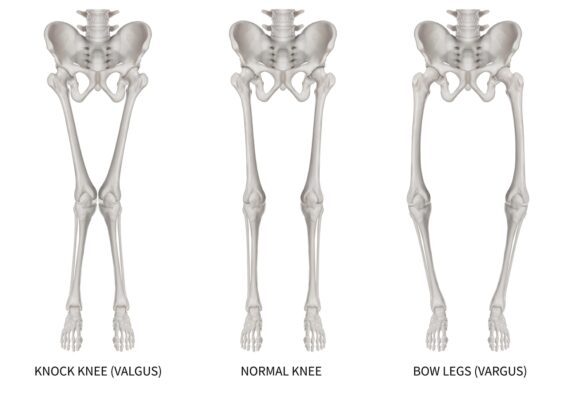
In knock knees, the inward angle of the knees causes them to touch, even while the ankles stay apart. This misalignment can lead to additional stress on the outer knee. Conversely, bow legs display the opposite alignment, with knees that angle outward, creating a gap between them.
This visual helps illustrate the differences in knee alignment, making it easier to understand how these conditions can affect joint stability and overall mobility.
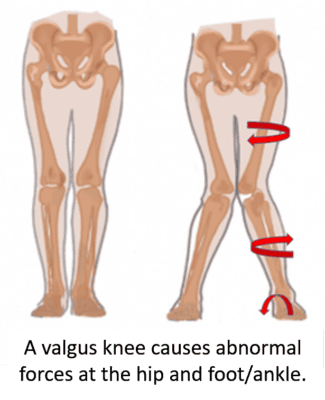
How Does The Valgus Knee Affect The Kinetic Chain?
The valgus knee affects the kinetic chain by disrupting the alignment and function of the entire leg. This misalignment causes problems in the knee’s lateral compartment and the joints above and below it.
For instance, a valgus knee often leads to internal hip rotation, placing additional stress on the iliotibial band (ITB) and other hip structures. It also impacts the foot, causing excessive pronation, which places abnormal forces on the ankle.
Since the knee is a key link in the kinetic chain, any misalignment or dysfunction can interfere with the leg’s ability to efficiently transfer forces from the hip to the ground. When the knee is compromised, the entire kinetic chain is affected, leading to biomechanical imbalances and issues in surrounding joints and muscles.
Different Grades Of Leg Misalignment
As with any condition, valgus knee has varying levels of severity. The valgus angle typically measures the degree of misalignment, with more severe cases exhibiting an angle greater than 20 degrees from straight. The condition is also classified based on whether the collateral ligaments, which provide stability to the knee, are tight or loose.
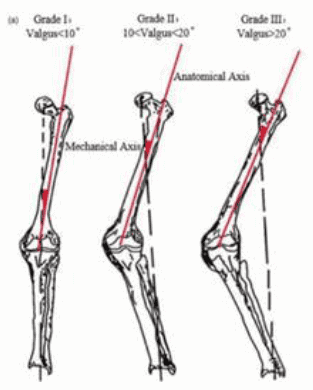
- Grade 1: This grade involves a mechanical axis deviation of less than 10 degrees. It is considered mild and is usually correctable without surgery. In Grade 1 cases, the medial collateral ligament (MCL) remains intact, providing stability to the knee.
- Grade 2: This grade indicates a more moderate range between 10 and 20 degrees. While the MCL is still functional, it may be elongated, suggesting that the knee is beginning to lose some stability.
- Grade 3: This grade involves a deviation greater than 20 degrees. In these severe cases, the medial stabilizing ligaments are typically non-functional, often requiring a constrained knee implant to restore stability.
Causes And Risk Factors Of Valgus Knee Formation
Valgus knee can result from various factors, such as long-term muscle weakness, particularly in the hips. Weak gluteus maximus muscles can cause the knee to collapse inward under stress, increasing the risk of ACL injuries, especially in girls, as it places stress on the ACL and other ligaments.
Over time, this inward pressure can also lead to lateral knee arthritis due to excess pressure on the outer knee compartment.
Natural Growth In Infants And Toddlers
Knock knees are a common part of normal development in infants and toddlers. The condition usually corrects itself by age 7, as the bones grow and align properly.
Genetic Factors And Family History
Genetics can play a role in the development of valgus knees. If a family member has experienced the condition, there is a higher likelihood that others in the family may develop it.
Bone Development Disorders
Certain bone development disorders, such as Blount’s disease and rickets, can lead to improper bone alignment, resulting in a valgus knee.
Leg Injuries Or Trauma
Severe leg injuries, particularly fractures or trauma to the knee joint, can cause misalignment, leading to the formation of knock knees.
Overweight Or Obesity
Carrying excess weight can strain the knee joint, increasing the risk of developing valgus knee, particularly in individuals predisposed to joint misalignment.
Vitamin D Deficiency (Rickets)
A lack of vitamin D can lead to rickets, a condition that weakens the bones and causes improper growth and alignment. Rickets can be a significant risk factor for developing valgus knee in children.
Bone Infection (Osteomyelitis)
Osteomyelitis, a bone infection, can weaken the structure of the bones and lead to misalignment, including knock knees. While less common, this can be a contributing factor in some cases.
Recognizing The Symptoms And Signs Of Knock Knees
Knock knees can present a range of physical symptoms, from subtle misalignments to more pronounced discomfort. Recognizing these signs early can help in seeking appropriate treatment and prevent further complications.
- Knee Misalignment: One of the most obvious signs is the inward angle of the knees. The knees may touch or come close together, while the ankles remain apart when standing.
- Abnormal Walking Patterns: Knock knees can cause a distinct gait in which the knees may rub together during walking.
- Discomfort or Pain: Discomfort or pain can develop due to the uneven distribution of weight and increased pressure on the outer knee.
- Knee Instability: Many patients report that their knees feel weak or buckle unexpectedly, increasing the risk of falls or injuries.
- Decreased Hip Flexibility: The inward angling of the knees can also affect the hips, reducing hip flexibility.
- Difficulty Walking or Running: Due to the misalignment, walking, running, or jumping can become increasingly difficult, leading to arthritis in the outer knee due to extra stress on the joint.
- Side-of-Knee Pain: Pain on the side of the knee may result from ligament injuries, iliotibial (IT) band syndrome, or meniscus issues. Accompanying symptoms can include tenderness, swelling, and discomfort, often worsening with movement or prolonged activity. Read More About Side-Of-Knee Pain.
Diagnosis
Physicians assess leg alignment and the space between the ankles while a patient is standing. X-rays measure the degree of misalignment and check for bone abnormalities. In more severe cases, additional imaging, like MRI (magnetic resonance imaging), may be used to examine ligaments and cartilage.
The physician will use these findings to recommend the best treatment approach based on the severity of the condition.
Conventional Treatment Options
Several conventional treatment options are available to manage knock knees, depending on the severity of the condition and the patient’s overall health.
- Weight Management: Weight management is crucial in reducing the load on the knees, potentially slowing the progression of the valgus knee and alleviating symptoms like pain.
- Physical Therapy (PT): PT focuses on strengthening the muscles around the knees and hips to improve alignment and reduce joint stress, helping improve stability and correct mild misalignments.
- Splinting or Bracing: This is often used in growing children, to realign the legs as they develop gradually, providing external support to help correct the knee angle and prevent further progression.
- Foot Orthotics: Custom shoe inserts are often recommended to help redistribute weight more evenly across the feet and legs.
- Guided Growth Surgery: This surgery involves placing a small metal plate on one side of the growth plate to guide bone growth and gradually correct knee alignment. It is critical to consult a physician about side effects, which may include pain at the surgical site, risk of infection, plate or screw irritation, and potential need for additional surgery.
- Osteotomy: In more severe cases, an osteotomy may be performed, in which a wedge of bone is removed or added to realign the knee. Risks may include pain, infection, blood clots, difficulty with bone healing, and potential for arthritis development.
- Knee Replacement Surgery: For adults with severe arthritis or deformity, this procedure replaces the damaged joint with an artificial one to restore function and relieve pain. However, some risks can include infection, blood clots, joint stiffness or limited mobility, implant loosening, and nerve damage.
The Regenexx Approach To Knee Function Support
The Regenexx approach offers a less invasive alternative for knee pain. Procedures using Regenexx injectates help harness the body’s natural healing ability. Using interventional biologics, the Regenexx approach offers patients an alternative to surgery and reduces the need for prescription drugs.
Pilar’s Story
Pilar is a middle-aged woman with a right-sided valgus knee who needed Celebrex just to function. She had the typical lateral compartment arthritis and was having difficulty climbing stairs and walking for any length of time. Her MRI is below:
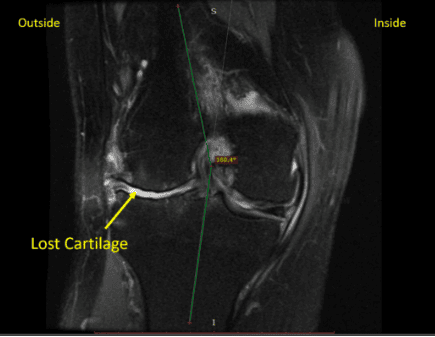
The blue line shows the knee angle as it should be, and the red line shows the actual angle, so she’s about 20 degrees off neutral. There is lost cartilage on the outside of the knee. This is severe medial compartment arthritis, which would normally require a knee replacement.
On exam, her MCL (the ligament on the inside of the knee) and ACL (a key ligament within the knee) were loose, causing instability. A physician in the Regenexx network extracted bone marrow concentrate containing stem cells from her hip, concentrated that fraction of cells in the lab, and then re-injected that using X-ray and ultrasound guidance into the following structures:
- ACL
- MCL
- Medial patellofemoral fascia
- Lateral compartment
About four months after the procedure, she reports 80% relief without invasive orthopedic surgery like a knee replacement. Her MCL and ACL ligaments are tighter, so the knee is more stable. Her hip pain has also decreased, likely because the improved valgus knee now puts less pressure on the outside of the hip.
The upshot? For some patients, this approach may provide an alternative to knee replacement surgery.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.
References
(1) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 2017;317(19):1967-1975. doi:10.1001/jama.2017.5283
(2) Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis [published correction appears in N Engl J Med. 2013 Aug 15;369(7):683]. N Engl J Med. 2013;368(18):1675-1684. doi:10.1056/NEJMoa1301408
(3) Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-2524. doi:10.1056/NEJMoa1305189
(4) Sihvonen R, Englund M, Turkiewicz A, Järvinen TL; Finnish Degenerative Meniscal Lesion Study Group. Mechanical Symptoms and Arthroscopic Partial Meniscectomy in Patients With Degenerative Meniscus Tear: A Secondary Analysis of a Randomized Trial. Ann Intern Med. 2016;164(7):449-455. doi:10.7326/M15-0899
(5) Nikolopoulos D, Michos I, Safos G, Safos P. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop. 2015;6(6):469-482. Published 2015 Jul 18. doi:10.5312/wjo.v6.i6.469
(6) Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: is “valgus collapse” a sex-specific mechanism?. Br J Sports Med. 2009;43(5):328-335. doi:10.1136/bjsm.2009.059139

Medically Reviewed By:
