Exploring Slipped Disc: Common Causes, Symptoms, And Treatment Options

Medically Reviewed By:
A slipped disc is a common spinal condition that can affect daily life, potentially causing discomfort and restricting movement. It may impact people across different age groups, often due to lifestyle factors, physical strain, or preexisting medical conditions. Understanding key aspects of this condition may help individuals recognize early signs and seek appropriate medical care.
People can take proactive steps to support spine health by exploring the causes, symptoms, and treatment options available for a slipped disc.
What Is A Slipped Disc?
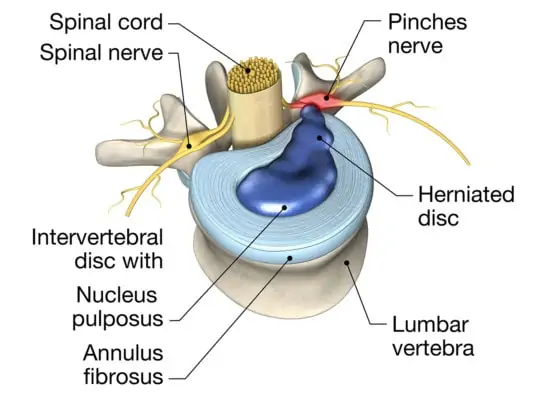
While the term “slipped disc” may suggest that the disc—a cushion-like structure that sits between the vertebrae—has moved entirely out of place, this is not quite accurate. A slipped disc typically refers to a herniated disc, meaning the inner gel-like substance, called the nucleus pulposus, may push through a tear in the tough outer layer known as the annulus fibrosus.
By contrast, a bulging disc is a condition where the disc fibers weaken and stretch, but the outer layer remains intact, which may cause the gel to create a bulge rather than breaking through.
Both herniated and bulging discs can occur anywhere along the spine, from the cervical (neck) discs to the lumbar (lower back) discs. Although a herniated disc may require closer attention due to the break in the outer layer, in most cases, both conditions may often be managed with conservative care options, reducing reliance on steroids or surgery.
Common Signs And Symptoms To Watch For
A slipped disc may present with various symptoms, affecting mobility and comfort. Identifying these signs early can help individuals seek timely care.
- Numbness Or Tingling – A slipped disc may compress nearby nerves, which could lead to tingling or numbness in the affected area.
- Limited Range Of Motion In The Back – Stiffness or discomfort may make it difficult to bend, twist, or move the back freely.
- Muscle Weakness – Compressed nerves may contribute to muscle weakness, making it harder to lift or hold objects.
- Back Pain When Getting Up From A Chair: Pain when rising from a seated position may be due to muscle stiffness, joint degeneration, or spinal issues. It can cause discomfort in the lower back, often easing with movement but recurring with prolonged sitting. Read More About Back Pain When Getting Up From A Chair.
Causes And Risk Factors Of Disc Problems
Disc issues can arise from various factors that affect the spine’s structure and function. Recognizing underlying causes and risk factors may help individuals explore ways to manage or prevent disc-related conditions, which may support spinal health over time.
Age-Related Degeneration
As the body ages, spinal discs naturally lose moisture and elasticity, making them more prone to wear and tear. This degeneration can lead to cracks or herniations in the discs, which may contribute to a higher likelihood of a slipped disc or other disc-related issues. The gradual breakdown of disc integrity is often associated with back pain and reduced spinal flexibility in older adults.
Repetitive Strain
Repetitive strain occurs when the spine endures continuous stress from activities like heavy lifting, bending, or twisting. Over time, this pressure may weaken the discs, making them more vulnerable to slipping or bulging. Jobs or activities involving repeated movements, particularly those that stress the back, may increase the likelihood of disc issues due to gradual wear and tear.
Injury
Sudden impacts or trauma, such as falls, car accidents, or sports injuries, can damage spinal discs, causing them to slip or rupture. These injuries may place immediate pressure on surrounding nerves, leading to sharp pain, restricted movement, and other symptoms. Even minor injuries, if left untreated, could contribute to long-term disc issues.
Genetics
Genetics may play a role in the likelihood of developing disc problems. Individuals with a family history of spinal conditions could be at higher risk for issues like slipped discs. Genetic factors may influence the strength and flexibility of spinal discs, making some people more prone to degeneration or injury, even with minimal strain or pressure on the spine.
Obesity
Excess body weight can contribute to additional strain on the spine, potentially increasing stress on discs. Obesity can also contribute to inflammation, which may worsen symptoms such as pain and stiffness, further impacting mobility and overall spinal health.
Sedentary Lifestyle
A lack of physical activity can weaken the muscles that support the spine, making the spinal discs more prone to injury and degeneration. Prolonged sitting or inactivity, especially when posture is compromised, will put additional pressure on the discs, especially in the lower back, potentially increasing the risk of a slipped disc. Regular exercise is essential for maintaining the flexibility and strength needed for a healthy spine.
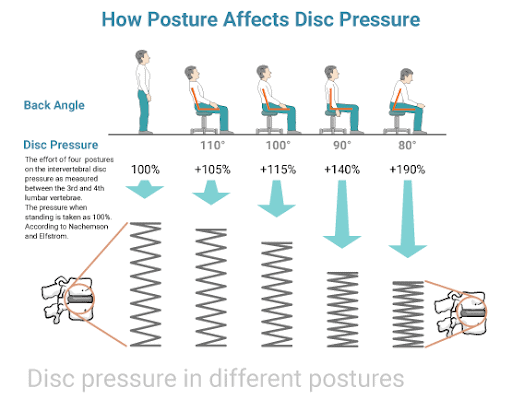
Poor Posture
Poor posture, such as slouching, can place uneven pressure on the spine and discs. Over time, this stress may weaken the discs, making them more susceptible to slipping or bulging. Maintaining good posture may help distribute weight evenly across the spine, reducing strain and potentially lowering the likelihood of disc-related issues.
Diagnosing A Bulging Or Slipped Disc
Accurate diagnosis is essential for understanding the extent of a disc injury and determining the most appropriate treatment options. Physicians may use several methods to diagnose a bulging or slipped disc:
- Physical Examination: A physician may assess symptoms, evaluate posture, and check for muscle weakness, reflex changes, and possible signs of nerve compression.
- Neurological Examination: Assessing sensation, reflexes, and muscle strength may help pinpoint areas affected by nerve compression or irritation.
- Imaging Tests: Advanced imaging techniques provide detailed views of the spine’s structure, which may help identify disc issues and assess nerve involvement. Common imaging methods include:
- MRI (Magnetic Resonance Imaging): The most common and detailed imaging technique for visualizing soft tissues, including spinal discs, to evaluate nerve involvement.
- CT Scan (Computed Tomography): Provides detailed cross-sectional images of the spine, which may help detect disc bulges or herniations when an MRI is not suitable.
- X-ray: Although it does not directly visualize spinal discs, an X-ray can help rule out other causes of back pain, such as fractures or spinal alignment issues.
- Discography: In select cases, a contrast dye is injected into the disc to determine if it is the source of pain. This test is used less frequently.
- Electrodiagnostic Testing: Tests such as electromyography (EMG) and nerve conduction studies can assess nerve function and help identify nerve damage or compression related to disc issues.
These diagnostic methods provide valuable insights into the nature of the disc issue, helping physicians develop a customized treatment plan.
Treatment Options For Disc Problems
Depending on the severity of symptoms, managing disc injuries often involves a combination of non-invasive and targeted treatments. These options may help reduce pain, improve mobility, and support recovery.
- Rest and activity modification: Reducing strain on the back by avoiding activities that worsen symptoms may support recovery.
- Hot therapy: Heat therapy may help relax tense muscles.
- Physical therapy: Exercises and stretches guided by a therapist can strengthen back muscles and improve flexibility.
- Alternative therapies: A variety of complementary approaches may be used alongside conventional treatments, though their effectiveness varies and is not always supported by clinical research:
- Acupuncture: Thin needles are used to stimulate specific points, which may help reduce pain and promote relaxation.
- Massage therapy: Massage therapy may help release muscle tension and improve circulation, which could contribute to pain relief.
- Yoga: Gentle stretches and poses may enhance flexibility and strengthen the core, which may help support the spine.
- Chiropractic care: Spinal adjustments aim to improve alignment, which may help reduce pressure on discs and nerves.
- Surgical options: Procedures like discectomy, laminectomy, or spinal fusion may be considered for severe or unresponsive cases.
Why You Should Avoid Surgery And Steroids For Herniated Or Bulging Discs
Herniated or bulging discs can compress and irritate surrounding nerves, causing pain in the back or anywhere along the affected nerve pathway, such as the leg or knee. Surgery typically involves removing disc tissue to alleviate this pressure; however, regardless of the method—coblation, laser, scalpel, or any other surgical device—surgery for a disc issue may carry potential risks, including disc weakening and long-term instability.
With surgery, the back wall of the thick annular covering is removed, potentially weakening that area of the disc, which could lead to further issues over time. This can cause future problems, especially because discs don’t heal well on their own, unlike most other tissues.
Another concern with surgery is the disruption of blood supply to the affected disc area, which may result in further complications and long-term problems with that disc. Laser surgery may be recommended; however, whether laser or scalpel, any procedure that involves removing parts of the disc can still weaken the disc.
Epidural steroid injections should also be avoided for slipped discs and other disc issues, as their effectiveness diminishes over time, and they are associated with potential side effects, such as increased risks of spinal fractures, cartilage loss, and adrenal issues.
For individuals exploring alternatives to surgery and epidural steroids, physicians in the licensed Regenexx network offer non-surgical options for addressing herniated or bulging discs. These proprietary methods focus on promoting the body’s natural repair processes and may be considered as part of a personalized care plan.
The Regenexx Approach For Disc Issues
While steroids and surgery are commonly recommended, they may not offer the best long-term solutions for a slipped disc or other spinal issues. Steroids can lead to complications, such as spinal fractures, cartilage damage, and adrenal issues. Similarly, surgery, which involves controlled tissue removal, may introduce new complications and long-term spine instability.
Physicians in the licensed Regenexx network offer interventional orthobiologics which may support the body’s natural repair abilities for certain disc-related conditions.
Consult with a physician in the licensed Regenexx network to learn more about your non-surgical options. The Regenexx approach offers an alternative to surgery and may reduce the need for prescription drugs, such as opioids.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
