Is ACL Surgery a Second Hit to the Joint Cartilage?
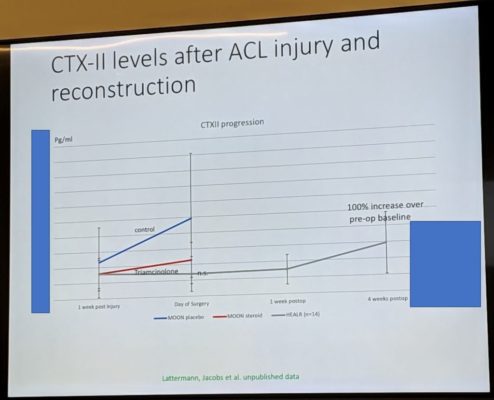
I’ve blogged before on the idea that we now have high-level evidence that suggests ACL surgery itself is harming the joint. While at the Havemeyer Symposium (think tank) at CSU, one of the physician-scientists presented an interesting slide that supports this idea. Let me explain.
The Prior Research
As I have reported previously, data from the ACL randomized controlled trial known as KANON demonstrated that early ACL surgery was correlated with cartilage loss. Meaning, if the patient waited to see if they needed the surgery (2/3rds didn’t need it), then the cartilage loss was less in that group. This study strongly suggested that it was the surgery causing the cartilage loss. Is there more evidence that shows that this is the case?
The Havemeyer Symposium
I’m spending 3 days with a number of scientific thought leaders in orthobiologics who are trading research information. One of those physician-scientists, Christian Latterman, M.D. from Harvard showed the above slide. He is a thought leader in the use of biomarkers in the knee to predict which patients will have more problems and how best to mitigate that risk.
What is a Knee Biomarker?
The synovial fluid in the knee has lots of chemicals in it. You can measure these and some of them may tell us which joints are degenerating or arthritic or healthy. These are called synovial fluid biomarkers.
What is Shown in the Slide?
First, since this is unpublished data, I redacted the slide a bit. What it shows is the CTXII levels in the synovial fluid of knees with ACL tears. The level of this biomarker is directly related to the level of cartilage injury, meaning, the higher the levels, the more cartilage injury in the knee. Right after the injury, injecting steroids helped the cartilage degeneration from the injury itself, but the ACL surgery marks another elevation in this cartilage injury marker. This maxes out at about 4 weeks.
This slide fits with the idea that the ACL surgery itself is harming the cartilage a second time. Why? Likely because we’re drilling holes in cartilage and bones to seat the tendon graft to replace the ACL.
Steroid Can Help Cartilage?
We have quite a bit of data that shows that steroid can hurt cartilage. First, what’s shown here is likely due to a short term down-regulation of an inflammatory cycle that was harming cartilage. What’s not shown nor measured here is whether that steroid shot might harm cartilage cells at some later point. We do know from one randomized controlled trial that repeated steroid shots can reduce cartilage thickness.
Having said all of that, a steroid shot in the knee may or may not be useful in certain circumstances and quite harmful in others. All of that has yet to be studied. So we have more research to do.
Non-surgical ACL Treatment
We have been treating ceratin ACL tears with a precise injection of bone marrow concentrate for years and documenting MRI changes consistent with the healing of the ligament. Watch the video below on how that procedure works:
In conclusion, big surgeries like ACL repair may harm the cartilage a second time. The cartilage gets a hit first at the time of injury and then a second time when we try to fix the ACL damage. This data would obviously argue for ACL repair techniques that don’t harm the joint.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
