ACL Surgery Is Not Cost Effective in New Study

Credit: Shutterstock
As I have written before, ACL surgery is a sacred cow of modern surgical sports medicine. It is the single procedure that most defines the whole field. Despite that, the recent research on the procedure hasn’t been favorable. Now a recent study adds to that by showing that the way we use the procedure in the U.S. isn’t cost-effective. Let’s dig in.
ACL Reconstruction 101
The idea behind this surgery is that the ACL, which is a major stabilizer of the knee joint, becomes torn and the patient is unable to return to sports. The surgeon then uses a tendon as a graft, removes the existing ligament, and drills holes in the femur and tibia to anchor the tendon graft. Hence a tendon now serves the function of the old ACL.
The Problems with ACLR
Despite this being a VERY popular surgery in the U.S. and elsewhere, it has some serious problems that have been identified by researchers:
- The new ligament has no position sensors (proprioception) and as a result, athletic prowess suffers (1,2,5)
- The re-tear rate of the new graft is high (3)
- The most common single bundle graft is at best a poor substitute for the original equipment which has two bundles (4)
- The surgery does nothing to prevent arthritis, which is one reason many patients chose surgery (7,10).
- 2/3rds of athletes never get back to their previous level of play (6)
- The surgery event itself is so traumatic that it’s a second hit to the cartilage (8).
- There is more cartilage loss in operated knees when compared to people who chose not to get the surgery (9)
The New Research
With all of these problems, the big question is whether ACL surgery is cost-effective. If you were to ask the average orthopedic surgeon, the conclusion that ACL surgery the way it’s performed in the U.S. is worth the money is as evident as the sky is blue. However, what if we look at it through the lens of a QALY study?
QALY means Quality Adjusted Life Year. This measures the quality of the number of years a patient has left to live. To be worth it, that quality of life has to improve with the surgery versus without. In addition, to be cost-effective, the number of dollars it takes to move that needle in the direction of a better quality of life has to be lower than not performing the surgery or the other treatment being compared.
The US versus Scandinavian ACL Approach
Our Scandinavian colleagues have been researching how best to use ACL surgery. Their research has shown that waiting to see which patients declare themselves over about a year as absolutely not being able to function without surgery is the best way to use this surgery. In that approach, these few patients are the only ones who get operated. This is VERY different than the US approach, which is often 6-12 weeks of physical therapy, and if that doesn’t work, the patient usually gets ACL reconstruction surgery. Existing research already shows that this Scandinavian approach works well (9).
The New Study
Researchers in the Netherlands looked at the QALY metrics of 167 patients with ACL tears with 85 being randomized to early ACL surgery (the US approach) and 82 to physical therapy. In the physical therapy group, the researchers used the Scandanavian protocol
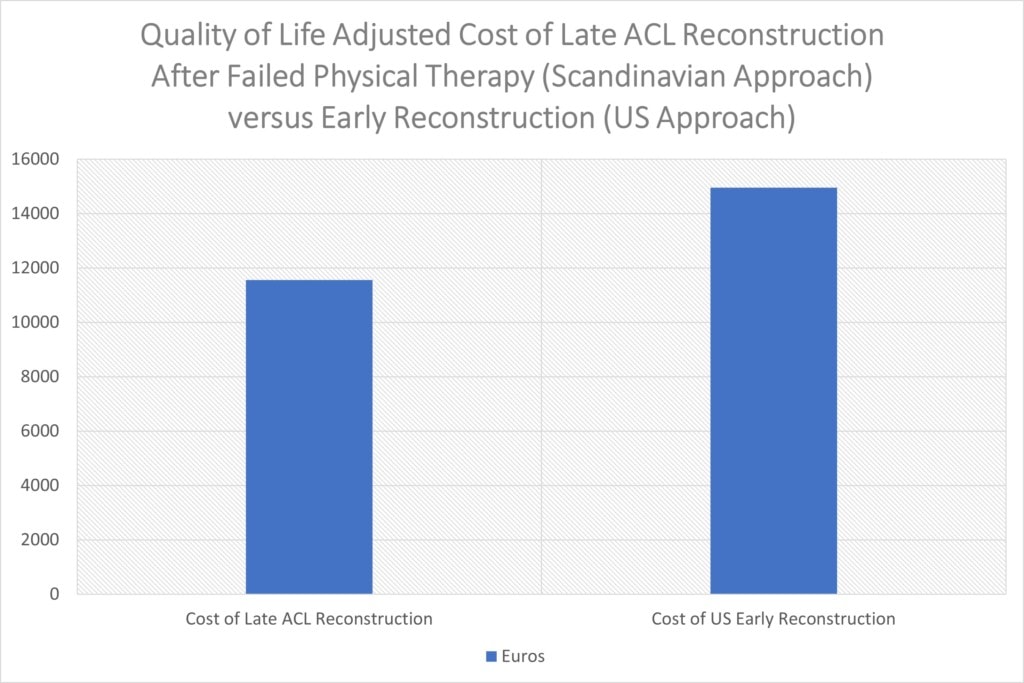
The total costs factoring in quality of life gains in Euros for the US (early reconstruction) approach was 14,951 and for the Scandanavian approach was 11,558. While the early reconstruction group had a slightly better quality of life, their costs were also much higher. Also, remember that this study was only two years of follow-up, so as some of the above issues come into play, like more arthritis in the ACL surgery group, the cost-effectiveness of the surgery side will likely get worse over time.
Will This Study Change Anything?
This paper is likely to create quite a stir because as I have said, this surgery has become a sacred cow in modern sports medicine. To get a sense of how bad that has become, I suggested a randomized study comparing our Perc-ACL injection to heal ACL tears without surgery to surgical ACL reconstruction and was turned down by a university professor that didn’t want to proceed. The reason given was that it would be “unethical” not to operate on every patient who failed a few weeks of PT. That was despite the existing Scandinavian studies at the time showing that the U.S. approach was not better than waiting a whole year to see which patients really needed surgery. Now that decision looks even crazier than it was two years ago.
The upshot? Our US approach to ACL reconstruction is less cost-effective than the Scandinavian approach. Will this study change anything? Probably not, as the ACL money machine is working hard to protect itself.
_______________________________________
References:
(1) Patterson MR, Delahunt E. A diagonal landing task to assess dynamic postural stability in ACL reconstructed females. Knee. 2013 Dec;20(6):532-6. doi: 10.1016/j.knee.2013.07.008. Epub 2013 Aug 18. PMID: 23962647.
(2) Bączkowicz D, Skomudek A. Assessment of neuromuscular control in patients after anterior cruciate ligament reconstruction. Ortop Traumatol Rehabil. 2013 Jun 28;15(3):205-14. doi: 10.5604/15093492.1058410. PMID: 23897997.
(3) Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013 Aug;41(8):1808-12. doi: 10.1177/0363546513493896. Epub 2013 Jun 28. PMID: 23813800.
(4) Song EK, Seon JK, Yim JH, Woo SH, Seo HY, Lee KB. Progression of osteoarthritis after double- and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2013 Oct;41(10):2340-6. doi: 10.1177/0363546513498998. Epub 2013 Aug 19. PMID: 23959965.
(5) Nyland J, Klein S, Caborn DN. Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthroscopy. 2010 Sep;26(9):1212-25. doi: 10.1016/j.arthro.2010.01.003. Epub 2010 Jun 16. PMID: 20810079.
(6) Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011 Mar;39(3):538-43. doi: 10.1177/0363546510384798. Epub 2010 Nov 23. PMID: 21098818.
(7) Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049-1057. doi:10.1177/0363546514526139
(8) Hunt ER, Jacobs CA, Conley CE, Ireland ML, Johnson DL, Lattermann C. Anterior cruciate ligament reconstruction reinitiates an inflammatory and chondrodegenerative process in the knee joint. J Orthop Res. 2021 Jun;39(6):1281-1288. doi: 10.1002/jor.24783. Epub 2020 Jun 29. PMID: 32558951.
(9) Culvenor AG, Eckstein F, Wirth W, Lohmander LS, Frobell R. Loss of patellofemoral cartilage thickness over 5 years following ACL injury depends on the initial treatment strategy: results from the KANON trial. Br J Sports Med. 2019 Sep;53(18):1168-1173. doi: 10.1136/bjsports-2018-100167. Epub 2019 Feb 8. PMID: 30737199.
(10) Wirth W, Eckstein F, Culvenor AG, Hudelmaier MI, Stefan Lohmander L, Frobell RB. Early anterior cruciate ligament reconstruction does not affect 5 year change in knee cartilage thickness: secondary analysis of a randomized clinical trial. Osteoarthritis Cartilage. 2021 Apr;29(4):518-526. doi: 10.1016/j.joca.2021.01.004. Epub 2021 Feb 4. PMID: 33549723.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
