Alternatives to Back Surgery for Herniated and Bulging Discs
There are quite a few alternatives to back surgery for patients with bulging or herniated discs. Back surgery, in general, is one of those procedures where everyone seems to know someone who had a bad experience. Newer techniques aim to try to heal the damage to the disc rather than cutting parts of it out. So let’s dig into this topic.
What is a Bulging or Herniated Disc?
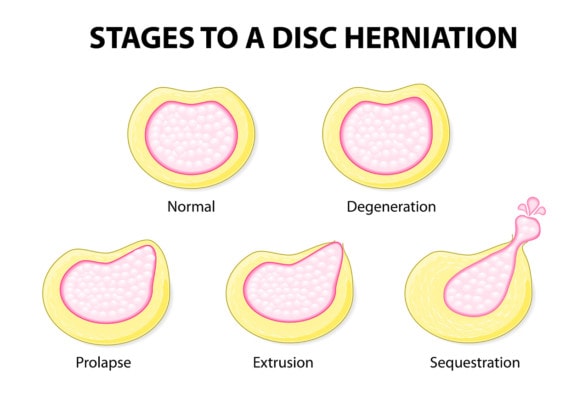
Designua/Shutterstock
The discs that live between your neck or back bones (vertebrae) are like shock absorbers and have a softer gel inside (nucleus pulposis) with a hard fibrous outside (annulus fibrosis). A bulging disc is when the outer fibers that make up the sidewalls of the disc become damaged through trauma or wear and tear and the inner stuff causes the sidewall to pooch out or bulge. This is also called a disc protrusion or prolapse. When the softer gel actually escapes the disc, this is called a disc herniation, herniated disc, or extrusion. All of this bulging or herniation can irritate the nearby spinal nerve leading to sciatica (radiculopathy).
How Successful is Lower Back Surgery?
Some research shows that patients with sciatica (symptoms down the leg) get better quicker, but after a year, there is little difference between patients who got surgery versus those who opted to do nothing (1-3). Meaning back surgery can help get rid of nerve pain faster, but if the patient waits, the pain will likely go away on its own over time.
What Kind of Surgery is Done for a Bulging Disc?
There are a number of different types of back surgery for disc bulges and herniations. All accomplish the same thing, which is cutting out the disc material (either the herniated inner part or the bulging sidewall) which is called Discectomy. The procedures basically differ in invasiveness. The traditional surgery (also called Open Discectomy) goes through the low back muscles and has many different problems, including killing off the important spinal stabilizing muscles (4). A number of smaller surgical approaches have since been developed which include minimally invasive endoscopic procedures that work through smaller windows to get at the disc. The two procedures work about the same as far as outcomes and complications, but the minimally invasive procedure has a quicker recovery time (5).
What Percentage of Back Surgeries Fail?
One of the reasons patients seek alternatives to back surgery is that the failure rate of spinal surgery ranged from 10 to 50% (6-10). This means the patients were classified as having continued low back or leg pain or new disabling symptoms after the surgery which is called Failed Back Surgery Syndrome. These failure rates are very high for surgery, which is why back surgery has gained a negative public perception (11).
What Happens if a Bulging Disc goes Untreated?
The simplest alternative to back surgery is skipping surgery. For herniated discs, most patients (75%) who don’t get the surgery will show an improvement in the disc herniation size on MRI and have complete resolution of their pain over 1-2 years (12). Another 15% will have partial regression of the disc and get partial relief, leaving only 10% with long-term pain and no change in the size of the herniation. For disc bulges, the opposite is generally true with resolution in only about 10% over time (13).
New Non-surgical Treatments for Disc Herniation and Bulges
A mainstay of alternatives to back surgery, introduced in the 1990s, is the use of epidural steroid injections. In this procedure, the doctor injects high dose steroids between the nerve and the disc by using x-ray guidance. These generally work in many patients (14). Having said that, the steroid and anesthetics used can be toxic to local nerves and disc cells (15-17).
Two new alternatives to back surgery have emerged using autologous orthobiologics, or the patient’s own platelets or stem cells. The first is an Orthobiologic Epidural which differs from an epidural steroid injection in the following ways:
- Growth factors are used which are obtained from the patient’s own blood platelets that have been shown to be beneficial to nerve health (19,20).
- A nanogram dose of steroid which is tissue friendly is used instead of the 1,000,000 times higher dose currently used in epidural steroid injections
- The anesthetic used is tissue friendly (ropivacaine instead of toxic bupivacaine) (24)
Our clinic published on a large case series of patients treated with these Orthobiologic Epidurals with excellent results (18). Many of these patients avoided surgery, hence for them, an Orthobiologic Epidural fit into the category of alternatives to back surgery.
Another new treatment for disc bulges is called Percutaneous Spinal Annuloplasty and takes a different approach as well. Instead of cutting out chunks of disc material that can weaken the sidewall and set the patient up for re-herniation (21), the goal is to get the tears in the disc to heal through an injection of the patient’s own stem cells. We have published several papers on the effectiveness of this procedure to reduce disc bulge sizes and symptoms without surgery (22,23), making this also fit into the alternatives to back surgery category.
The upshot? There are several new alternatives to back surgery that have a different approach. Namely to use your body’s platelets or stem cells to try to heal the damage rather than cut important structures out.
_____________________________________________________________
References:
(1) Lurie JD, Tosteson TD, Tosteson AN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial [published correction appears in Spine (Phila Pa 1976). 2015 Jan;40(1):E59]. Spine (Phila Pa 1976). 2014;39(1):3–16. doi: 10.1097/BRS.0000000000000088
(2) Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008;336(7657):1355–1358. doi: 10.1136/bmj.a143
(3) Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983 Mar;8(2):131-40. https://www.ncbi.nlm.nih.gov/pubmed/6857385
(4) Kotil K, Tunckale T, Tatar Z, Koldas M, Kural A, Bilge T. Serum creatine phosphokinase activity and histological changes in the multifidus muscle: a prospective randomized controlled comparative study of discectomy with or without retraction. J Neurosurg Spine. 2007 Feb;6(2):121-5. https://www.ncbi.nlm.nih.gov/pubmed/17330578
(5) Harrington JF, French P. Open versus minimally invasive lumbar microdiscectomy: comparison of operative times, length of hospital stay, narcotic use and complications. Minim Invasive Neurosurg. 2008 Feb;51(1):30-5. doi: 10.1055/s-2007-1004543.
(6) Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013 Feb;7(1):56-9. doi: 10.1177/2049463713479096.
(7) Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979–987. Published 2016 Nov 7. doi: 10.2147/JPR.S92776
(8) Clancy C, Quinn A, Wilson F. The aetiologies of failed back surgery syndrome: a systematic review. J Back Musculoskelet Rehabil. 2017;30(3):395–402 https://www.ncbi.nlm.nih.gov/pubmed/27689601
(9) Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine (Phila Pa 1976). 2007;32(19):2119–2126. https://www.ncbi.nlm.nih.gov/pubmed/17762814
(10) Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Chronic opioid therapy after lumbar fusion surgery for degenerative disc disease in a workers’ compensation setting. Spine (Phila Pa 1976). 2015;40(22):1775–1784 https://www.ncbi.nlm.nih.gov/pubmed/26192725
(11) “Doctors getting rich with fusion surgery debunked by studies:” Bloomberg, Dec 30 2010. Accessed 10/12/19. https://www.bloomberg.com/news/articles/2010-12-30/highest-paid-u-s-doctors-get-rich-with-fusion-surgery-debunked-by-studies
(12) Kesikburun B, Eksioglu E, Turan A, Adiguzel E, Kesikburun S, Cakci A. Spontaneous regression of extruded lumbar disc herniation: Correlation with clinical outcome. Pak J Med Sci. 2019;35(4):974–980. doi: 10.12669/pjms.35.4.346
(13) Keskil S, Ayberk G, Evliyaoğlu C, Kizartici T, Yücel E, Anbarci H. Spontaneous resolution of “protruded” lumbar discs. Minim Invasive Neurosurg. 2004 Aug;47(4):226-9. https://www.ncbi.nlm.nih.gov/pubmed/15346319
(14) Manchikanti L, Knezevic NN, Boswell MV1, Kaye AD, Hirsch JA. Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis. Pain Physician. 2016 Mar;19(3):E365-410. https://www.ncbi.nlm.nih.gov/pubmed/27008296
(15) Mather LE, Copeland SE, Ladd LA. Acute toxicity of local anesthetics: underlying pharmacokinetic and pharmacodynamic concepts. Reg Anesth Pain Med. 2005 Nov-Dec;30(6):553-66. https://www.ncbi.nlm.nih.gov/pubmed/16326341
(16) Mackinnon SE, Hudson AR, Gentili F, Kline DG, Hunter D. Peripheral nerve injection injury with steroid agents. Plast Reconstr Surg. 1982 Mar;69(3):482-90. https://www.ncbi.nlm.nih.gov/pubmed/7063571
(17) Eder C, Pinsger A, Schildboeck S, Falkner E, Becker P, Ogon M. Influence of intradiscal medication on nucleus pulposus cells. Spine J. 2013 Nov;13(11):1556-62. doi: 10.1016/j.spinee.2013.03.021
(18) Centeno C, Markle J, Dodson E, et al. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017;4(1):38. Published 2017 Nov 25. doi: 10.1186/s40634-017-0113-5
(19) Sowa Y, Kishida T, Tomita K, Adachi T, Numajiri T, Mazda O. Involvement of PDGF-BB and IGF-1 in activation of human Schwann cells by platelet-rich plasma. Plast Reconstr Surg. 2019 Aug 27. doi: 10.1097/PRS.0000000000006266.
(20) Sánchez M, Anitua E2, Delgado D, Sanchez P, Prado R, Orive G, Padilla S. Platelet-rich plasma, a source of autologous growth factors and biomimetic scaffold for peripheral nerve regeneration. Expert Opin Biol Ther. 2017 Feb;17(2):197-212. doi: 10.1080/14712598.2017.1259409.
(21) Shin BJ. Risk factors for recurrent lumbar disc herniations. Asian Spine J. 2014;8(2):211–215. doi: 10.4184/asj.2014.8.2.211
(22) Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016;14(1):253. Published 2016 Sep 1. doi: 10.1186/s12967-016-1015-5
(23) Centeno C, Markle J, Dodson E, et al. Treatment of lumbar degenerative disc disease-associated radicular pain with culture-expanded autologous mesenchymal stem cells: a pilot study on safety and efficacy. J Transl Med. 2017;15(1):197. Published 2017 Sep 22. doi: 10.1186/s12967-017-1300-y
(24) Dregalla RC, Lyons NF, Reischling PD, Centeno CJ. Amide-type local anesthetics and human mesenchymal stem cells: clinical implications for stem cell therapy. Stem Cells Transl Med. 2014;3(3):365–374. doi: 10.5966/sctm.2013-0058

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
