Atypical Trigeminal Neuralgia?
Since we have non-surgical treatments for trigeminal neuralgia that don’t involve brain surgery, we often see patients with this condition. However, our medical care system is often like a dog with a bone sometimes and creates and then holds onto a diagnosis even when it no longer makes sense. Today I’ll review the case of a patient who was diagnosed with atypical trigeminal neuralgia who really doesn’t have that diagnosis. Let’s dive in.
What Is Trigeminal Neuralgia?
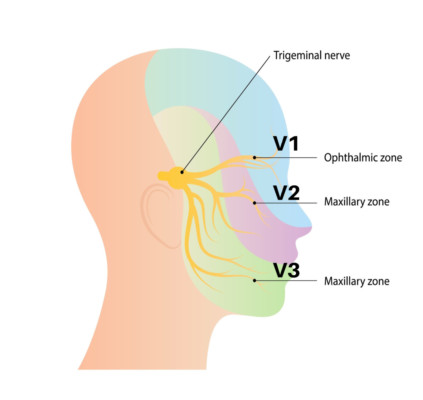
Trigeminal neuralgia is caused by the 5th cranial nerve which supplies sensation to the face. It breaks into three parts as shown above which are V1 in the forehead, V2 at the cheek, and V3 at the jaw. Patients often experience disabling nerve pain, often shocking or tingling. These nerve areas are hypersensitive. Meaning even a mild brushing or stimulation of the face can be painful. Other names for this condition include:
- Tic Douloureux
- Fothergill Disease
- TN (Abbreviation)
- Trifacial Neuralgia
Classifying Trigeminal Neuralgia
Trigeminal neuralgia is broken into two types: type 1 and type 2. Type 1 is “classical” as described above. Type 2 is atypical trigeminal neuralgia. This has been described as a wastebasket term for facial pain that doesn’t look like trigeminal neuralgia. I’ll explore today why this atypical trigeminal neuralgia box is a real disservice for many patients and often ends up being a diagnosis that doesn’t help them find an effective treatment.
Treatment for Trigeminal Neuralgia
The problem with modern trigeminal neuralgia treatment is that it’s either medications or brain surgery. There is no in-between. Before we dive into this section, realize that these are treatments for TN1 (type 1) and not for atypical trigeminal neuralgia (type 2 or TN2). Let’s review.
Medications are focused on nerve pain. These can include old standbys like Neurontin (Gabapentin) or Tegretol (Carbamazepine) or newer much more nerve-focused drugs like Lyrica (Pregabalin).
Surgical therapy often includes Microvascular decompression (MVD). This is where an incision is made behind the ear, a small hole is drilled in the skull, and, under an operating microscope, the trigeminal nerve is visualized. If there is something near the nerve like a blood vessel, that is moved and a cushion placed by the nerve.
Other treatments include RFA (Radiofrequency Ablation). This is where a probe is placed close to the nerve and the tip heats up, destroying the nerve. There is also a gamma knife therapy (stereotactic radiosurgery), whereby the area is irradiated to try to accomplish a similar goal to RFA.
Is there a way to avoid brain surgery or destroying the nerve? Our focus is to precisely inject platelet growth factors around the trigeminal nerve using sophisticated image guidance. These include growth factors that may have the ability to help the nerve heal.
Atypical Trigeminal Neuralgia
Not as much is known about atypical trigeminal neuralgia as Type 1 classical disease (1). For type 1, the prevalence is 0.1-0.2 per thousand people (a rare problem) with a female-to-male ratio of about 3:2 (impacting more women than men) (2). For atypical trigeminal neuralgia, the issue is that there is massive overlap with other problems that impact the face and head. This is a shortlist of other problems that cause similar facial pain symptoms:
- TMJ-Temporomandibular Joint-The jaw joint can cause point pain just below and in front of the ear. However, once the masseter muscle becomes painful due to chronic bruxism (teeth grinding), the pain can easily fill the V2 and V3 areas.
- CCI-Craniocervical Instability -This is where the ligaments that hold the head on are damaged or are loose leading to the excessive motion of the head on the upper neck. This is more common in patients who have been in a car crash or who have had other head trauma or who have loose ligaments (EDS or Ehlers-Danlos Syndrome). This can also irritate the trigeminal nerve leading to facial pain. It can also cause TMJ.
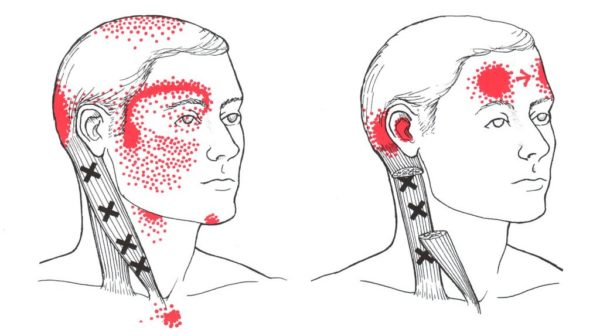
- Trigger Points in Facial or Neck Muscles-These are chronic spots in muscles that are tight and weak and refer pain to other areas. Above is the referral pattern for trigger points in the sternocleidomastoid muscle. Note that the pattern on the left matches V1 and V2 pain.
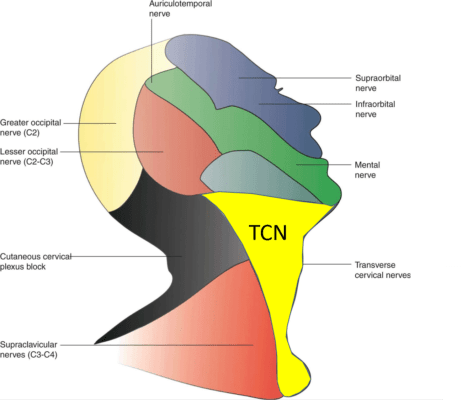
- TCN-Transverse Cervical Nerve-(aka superficial cervical plexus)-This is the nerve complex that lives under the SCM. It supplies the skin below V3 (above in bright yellow marked TCN), so problems here can often be called atypical trigeminal neuralgia.
Next, we’ll explore how a patient diagnosed with atypical trigeminal neuralgia really had something else.
Diagnosis or Misdiagnosis?
I’d like to share a patient story that may help some atypical trigeminal neuralgia patients get clarity on their diagnosis. This is a patient I evaluated in the clinic this past week. Let’s dive in.
The patient had a multi-year history of right facial pain in the V2/V3 area. She was told that she had atypical trigeminal neuralgia. I suspect that’s because she didn’t have many of the nerve symptoms so common with the diagnosis and had occipital headache pain as well. All of this began with a dental procedure where her head and neck were hyper-extended for a prolonged period.
On exam, interestingly, the patient has no side-to-side sensation difference in the V2 area. That was odd because trigeminal neuralgia is a nerve hypersensitivity issue, which means that by definition her side-to-side or same side sensation should have been different. That was the first strike against this being atypical trigeminal neuralgia.
On further examination, her right TMJ joint was tender and only that joint. That was another problem, as you would expect a whole nerve territory like V2 or V3 to be tender in an atypical trigeminal neuralgia patient and not just her jaw joint. That was the second strike.
When I checked her neck, the diagnosis of atypical trigeminal neuralgia fell apart. She had a side-to-side sensation change in the C2 dermatome, which meant there was an upper neck nerve problem. She was also tender in the upper neck facet joints C0-C2, which was also indicative of an upper neck problem. The final straw was realizing that she was hypermobile. All of this combined meant that she was more likely to have craniocervical instability (CCI) due to Ehlers Danlos than primary atypical trigeminal neuralgia. While her facial pain could be due to trigeminal neuralgia, that’s more likely to be secondary to the CCI. It’s also possible that her facial pain is just due to TMJ, which is also common in CCI patients.
Why this misdiagnosis? Because the type of physicians who would diagnose trigeminal neuralgia just don’t have much experience in either TMJ or CCI diagnosis. Hence, rather than looking further to see what was really wrong, it was easier to put this patient into the “atypical” box.
The upshot? Trigeminal neuralgia can be awful. However, what can be equally awful is a misdiagnosis. Hence, if you get put into that atypical trigeminal neuralgia box, it’s time to look deeper!
________________________________
(1) Weiss, A.L., Ehrhardt, K.P. & Tolba, R. Atypical Facial Pain: a Comprehensive, Evidence-Based Review. Curr Pain Headache Rep 21, 8 (2017). https://doi.org/10.1007/s11916-017-0609-9
(2) Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurol Sci. 2005 May;26 Suppl 2:s65-7. doi: 10.1007/s10072-005-0410-0. PMID: 15926023.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.