Big Procedures, Big Problems. Little Procedures, Little Problems

Credit: Shutterstock
I’ll never forget my brother-in-law’s comments when our kids were young. Having older kids at the time, he told us, “Little kids, little problems. Big kids, big problems”. Today I’ll modify his advice to “Big procedures, big problems. Little procedures, little problems”. Let’s dig in.
The Trend Towards Minimally Invasive Care
Minimally invasive in medicine has been a serious trend since the early 90s. This means that common surgical procedures have been getting smaller and smaller. For example, the open-heart surgery that was common when I was in medical school in the 1980s was CABG (Coronary Artery Bypass Graft). However, by the early 2000s, that surgery began to be replaced with coronary artery stenting, which could be performed through a catheter inserted in an artery.
This trend is based on a simple notion. If you reduce the tissue trauma needed to get the job done, you reduce the possible side effects from the procedure. For example, open heart surgery requires the doctor to literally saw through the sternum and the phrase “crack the chest” comes from the sound of broken ribs as you spread the sternum open to allow visualization of the heart. Compare that to floating a catheter into an artery in the groin and deploying a stent via x-ray guidance and there’s just no comparison in all the bad stuff that can happen.
The Rise of Interventional Orthobiologics
This week I interviewed a bright young physician for our Interventional Orthobiologics fellowship at our practice in Colorado. In this program, we’re educating the next generation of physician leaders in what we call Interventional Orthobiologics. He asked how we started all of this, way back when. What he meant, is how did we end up leaders in the movement to convert patients from invasive orthopedic surgeries to image-guided injections of orthobiologics? The core answer is simple, frustration with the status quo. So this morning I’ll give you two good examples of what sparked that frustration with the insanity of modern orthopedic surgery.
Case #1-The Dumb Synovectomy
One of the silliest procedures devised by my orthopedic colleagues is a surgery called a Synovectomy. I just saw this patient in the office this week. He has always had pain at the patellar tendon and an ultrasound exam showed that the tendon is beaten up. He also has some swelling in the joint. In the world of Interventional Orthobiologics, this is easily remedied by high-dose PRP injections into the tendon and joint using precise ultrasound guidance. However, a local surgeon decided that what he really needed was to remove the synovial lining of the knee joint (Synovectomy). Why is this a problem? Because that lining holds about half of all of the natural stem cells in a joint.
Did this work? Of course not. His pain didn’t change and it was easy to show him on ultrasound that the patellar tendon (which is exactly where he hurts) is the problem and is in need of help. However, now he has a new problem caused by the surgery, which is scarring between the patellar tendon and the joint fat pad.
Hence, what could have been done with a small procedure with small possible side effects was instead done incorrectly by a huge surgery that caused more problems than it fixed. It’s this frustration that caused our practice to begin creating this new field. Just like yesterday, way back in 2005 when we started it, I said to myself, “Enough”.
Case #2-Manufacturing a Quadraplegic
My second example is very sad, but really illustrates the concept of big procedures, big problems. This is the case of a patient undergoing an upper cervical Fusion that was sent to me by a colleague. I’ve seen many examples through the years where the screws used to hold the bones together in this surgery often go astray. For example, I’ve found them in the C0-C1 joint and other places they were never intended to be. However, this one is so awful, it’s better to show you the films:
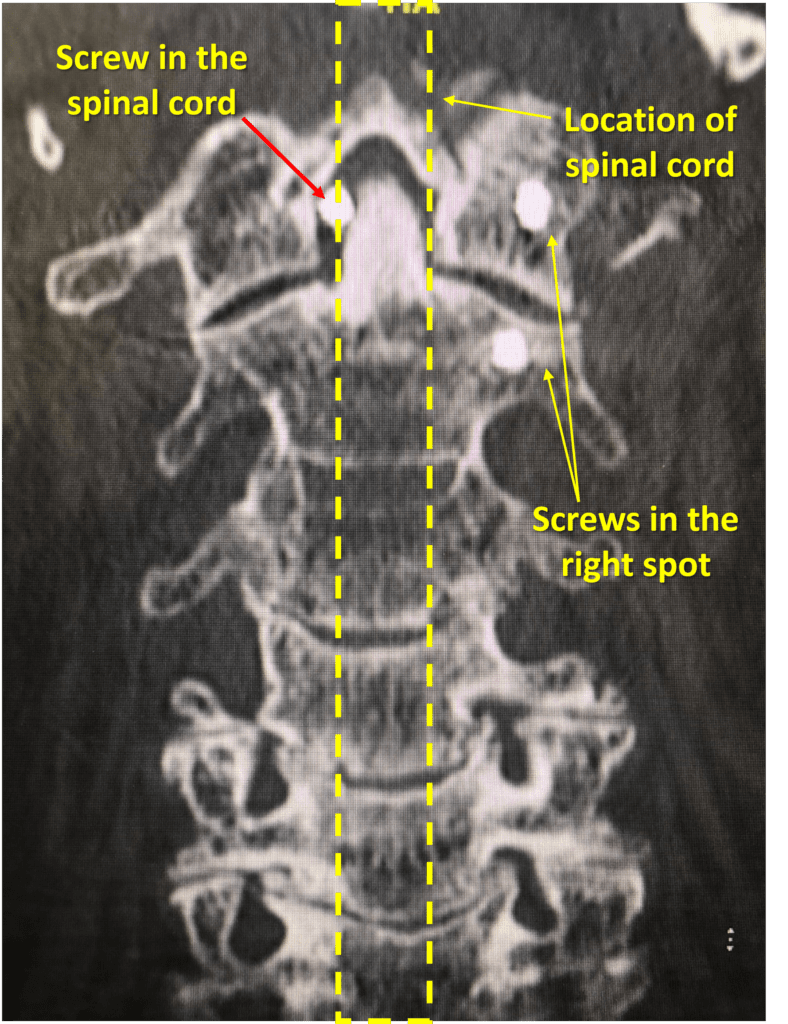
Here we see the CT scan of a patient that was undergoing Fusion surgery of the upper neck for Cranial Cervical Instability (CCI). The screws that hold the fusion hardware on the right side of the screen went into the right spot. The screw in the upper left of the screen did not. That screw ended up not in the bone, but in the space between the Dens of C2 and the Atlas. The problem? The dashed lines represent where the spinal cord travels, so that screw likely damaged the spinal cord. How do we know for sure? The patient woke up from the surgery a quadriplegic.
Given that this is not my patient, I don’t know if we could have helped this patient with precise injections. I do know that we could have easily injected these joints at C0-C1 and C1-C2 with orthobiologics or we could have tried other less invasive procedures to help various areas like ligaments or nerves. Would that have worked? Unsure, however, these less invasive regenerative procedures certainly should have been tried before taking on the risk of an upper neck Fusion surgery.
No Procedure Is Without Risk
All procedures, whether big or small have risks. However, as I have repeatedly said through the years, we should try to use less invasive procedures with smaller risks before using bigger procedures with bigger risks. Hence, I hope these two examples help patients understand why my frustration way back in 2005 forced our practice to begin looking for a better way. In addition, in 2021, I am not the only person involved in birthing this new medical specialty called International Orthobiologics. At least a dozen others are now involved in improving these procedures and concepts. I am happy to say that a good chunk of those physicians are our former fellows.
The upshot? Big procedures, big problems. Little procedures, little problems. That’s a mantra you should say to yourself every time you’re offered an invasive surgery. Is there another less invasive option? Oftentimes finding those options require the patient to do some homework, but they’re out there!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
