Can a Ligament Grow Back? Getting an Athlete’s ACL to Heal
On this page:
- What is the ACL and can it grow back?
- Can ACL tears be treated without surgery?
- An athlete’s ACL story
We began treating ACL tears using x-ray guidance and high-dose bone marrow concentrate back in 2011 before anyone else was performing that procedure and frankly before anyone else was doing much of anything with bone marrow concentrate.
Early on I had to answer the question for myself, “Can the ACL grow back?” Meaning that despite orthopedic surgeons often claiming that the ACL can’t grow back, would we see the opposite if we injected substances to promote healing? This morning’s example is a patient who I didn’t think we could help, but who eventually responded. He has taught me a thing or two about what’s possible and how to sequence these procedures.
What Is the ACL? Can the ACL Grow Back?
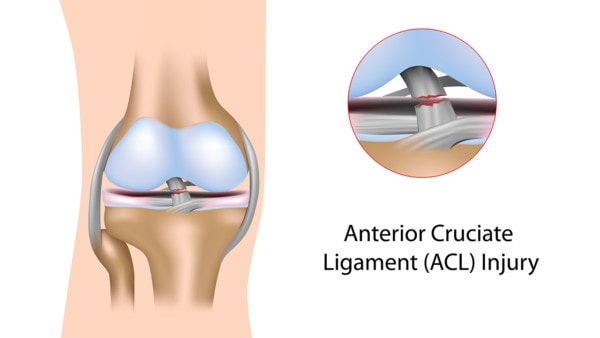
Alila Medical Media/Shutterstock
The ACL (Anterior Cruciate Ligament) is a tough complex of ligament bands that live in the middle of the knee. They keep the leg bone from moving forward and rotating on the thigh bone. The urban myth for decades has been that a torn ACL can’t grow back. Where did that come from? As far back as the 1930s the idea was hatched that a completely torn ligament couldn’t heal on its own (1). In the 80s, there were attempts to sew the two torn ends back arthroscopically, but this often failed (2).
Then in 2012, shortly after we embarked on our work, a research paper looked at complete ACL tear patients who had surgeries delayed by using follow-up MRIs. The researchers demonstrated that some complete tears did successfully heal on their own (3).
However, this study suffered from a big problem that scientists call selection bias. Meaning that the patients who were more likely to be OK with delaying surgery (which made up the study subjects here) were also those who were more likely to be feeling better without the need for surgery.
However, this was about the same time that surgeons began experimenting with poking holes in the knee bones during surgery to release bone marrow to prompt ACL healing, so the idea that the ACL could heal with help caught on (4). The idea here was that the bone marrow contained stem cells which could produce new ligament tissue or help the existing tissue heal (5). While this is a surgical approach, could this be accomplished with only an injection?
Can the ACL grow back through an injection of the patient’s own healing substances like platelet-rich plasma (PRP) or bone marrow concentrate? We have published on cases of healed ACL ligaments (many of which were completely torn) after we precisely injected bone marrow concentrate using precise fluoroscopy guidance (6,7). This is a non-surgical walk-in/walk-out procedure that uses sophisticated imaging guidance to place cells in the torn parts of the ligament.
We were surprised that these patients, many of whom were surgical candidates, had post-injection MRIs showing ACL regrowth and went back to full activity. They also had a lower retear rate than if they had surgery. Others have also published on injecting PRP into partial ACL tears (not surgical candidates) with excellent results (8).
How Is this Non-Surgical Procedure Performed?
The procedure we created to get complete ACL tears to heal on their own was not easy to perfect. It took years of trial and error to dial in a reliable injection procedure. We tried both ultrasound and fluoroscopy (real-time x-ray) and the latter proved to be the better technology.
This procedure is now taught through the Interventional Orthopedics Foundation. To see what the Perc-ACLR injection procedure (Percutaneous ACL Repair) looks like, watch my video below:
An Athlete’s ACL Story
If we really want to answer the question “Can the ACL grow back?” with a practical example, this recent patient result surprised even me. He was a star in high school who tore his ACL doing what he loved and his parents decided to try the Perc-ACLR procedure instead of surgery. His initial MRI didn’t look great, so I had my doubts but told his folks that I would know more once I injected radiographic contrast into the ACL using fluoroscopy.
Why? This can give a good read on how many fibers remain intact. After the first injection, I wasn’t that optimistic, but we proceeded with the Perc-ACLR procedure using bone marrow concentrate. Then, because of my concerns, I saw him back a few more times for PRP booster shots performed the same way. By the last injection, the flow of the contrast in the ligament plus his MRIs weren’t looking like I wanted, so I told his parents to consider surgery to replace the ligament.
However, recently I learned that since the patient was feeling better and better and fully functional at an elite level, his parents decided to forego the surgery and stayed the course. His mom sent me a recent radiologist’s report which stated that despite the complete ACL tear that we started with the read was now an ACL sprain without an ACL rupture. I got the films and this is what I saw:

I have outlined the ACL in the faint yellow dashed lines. The ligament on the left is a blown-out mess, what would be called a complete ACL tear requiring surgical replacement of the ligament. The next picture shows some consolidation of the ligament (darker is better on these images).
The third image is what I saw when I told him that he needed surgery. This is a ligament that’s trying to heal, but not quite making it. The fourth image to the right is the one readout by the radiologist as an ACL sprain. Suffice it to say that this ligament went from a mess of damaged fibers late last year to the MRI appearance of a normal ACL with a sprain by this summer.
He, his college, and his parents need to decide what to do next. I told his folks that I would like to repeat a bone marrow concentrate Perc-ACLR procedure or if that didn’t work with his schedule, to have him play with a brace and get a PRP booster now to promote more healing over the season.
So can the ACL grow back? We’ve seen excellent results on post-injection MRIs that support that concept. In addition, these results fit with how these patients respond physically in that most return to full sporting activities. This has provided more evidence that the ligament can grow back.
So in my opinion, for most of these patients, the ACL healing procedure doesn’t require surgery, but instead a precise injection of the patient’s own concentrated bone marrow.
__________________________________________________
References
(1) Wittek A. Replacement of the cruciate ligament with patellar tendon. Schweiz Med Wochenschr. 1935;65:103–104.
(2) Sandberg R, Balkfors B, Nilsson B, Westlin N. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg Am. 1987;69:1120–1126.
(3) Costa-Paz M, Ayerza MA, Tanoira I, Astoul J, Muscolo DL. Spontaneous healing in complete ACL ruptures: a clinical and MRI study. Clin Orthop Relat Res. 2012;470(4):979-985. doi:10.1007/s11999-011-1933-8
(4) Vavken P, Murray MM. The potential for primary repair of the ACL. Sports Med Arthrosc Rev. 2011;19(1):44-49. doi:10.1097/JSA.0b013e3182095e5d
(5) Malahias MA, Chytas D, Nakamura K, Raoulis V, Yokota M, Nikolaou VS. A Narrative Review of Four Different New Techniques in Primary Anterior Cruciate Ligament Repair: “Back to the Future” or Another Trend?. Sports Med Open. 2018;4(1):37. Published 2018 Aug 9. doi:10.1186/s40798-018-0145-0
(6) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437-447. Published 2015 Jul 31. doi:10.2147/JPR.S86244
(7) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. Published 2018 Sep 3. doi:10.1186/s12967-018-1623-3
(8) Koch M, Mayr F, Achenbach L, et al. Partial Anterior Cruciate Ligament Ruptures: Advantages by Intraligament Autologous Conditioned Plasma Injection and Healing Response Technique-Midterm Outcome Evaluation. Biomed Res Int. 2018;2018:3204869. Published 2018 Jul 25. doi:10.1155/2018/3204869

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
