Can PRP Help Rheumatoid Arthritis Patients?
I have been very cautious in recommending orthobiologics to patients with rheumatoid arthritis (RA). However, recently I found high-quality data on using PRP in these patients. So what does that say? Does PRP help patients with RA?
What is RA and How is It Different than OA?
Rheumatoid arthritis (RA) is an inflammatory disease where the immune system attacks the joints. Osteoarthritis (OA) is caused by many factors, but the key thread connecting them all is wear and tear. RA is also different in that it used to lead to very severe disabling disease that could be life-threatening if the disease attacked the upper neck. Now that disease-modifying drugs are available, severe RA cases can be controlled.
Why Was I Cautious About Recommending Orthobiologics in RA Patients?
RA patients often take powerful anti-inflammatory biologic drugs to reduce the joint destruction that happens due to this disease. The concern was that these drugs would interefere with the normal inflammatory process believed to be a part of how PRP works.
A Surprising PRP Study I Hadn’t Indexed
When I publish my PRP infographics and study reviews on PRP I tend to search the US Library of Medicine under PRP and various conditions like knee osteoarthritis or shoulder rotator cuff tear. That works well for getting studies about common issues identified. However, it also caused me to miss an important randomized controlled trial on RA and PRP.
A patient had asked a clinic staff member about whether there was research showing that PRP helped RA. I then quickly search PubMed for “PRP Rheumatoid Arthritis Randomized” and this new study popped up.
In this 2021 Randomized Controlled Trial, researchers took 60 rheumatoid arthritis patients who met ACR-EULAR criteria with low disease activity who were being treated with non-biologic DMARDs for 3 months. These patients had the following joints involved and injected:
- 24 wrists
- 10 elbows
- 12 ankles
They were injected with PRP once a month for 3 months. A similar group was randomized to receive Kenalog 40 mg. All patients in both groups continued to receive thier DMARD drugs.
The PRP that was used was leukocyte-poor, double spin, and just exceeded the 2X standard and based on the platelet content reported was low dose at approximately 2.5-3X on average.
How Did PRP Perform?
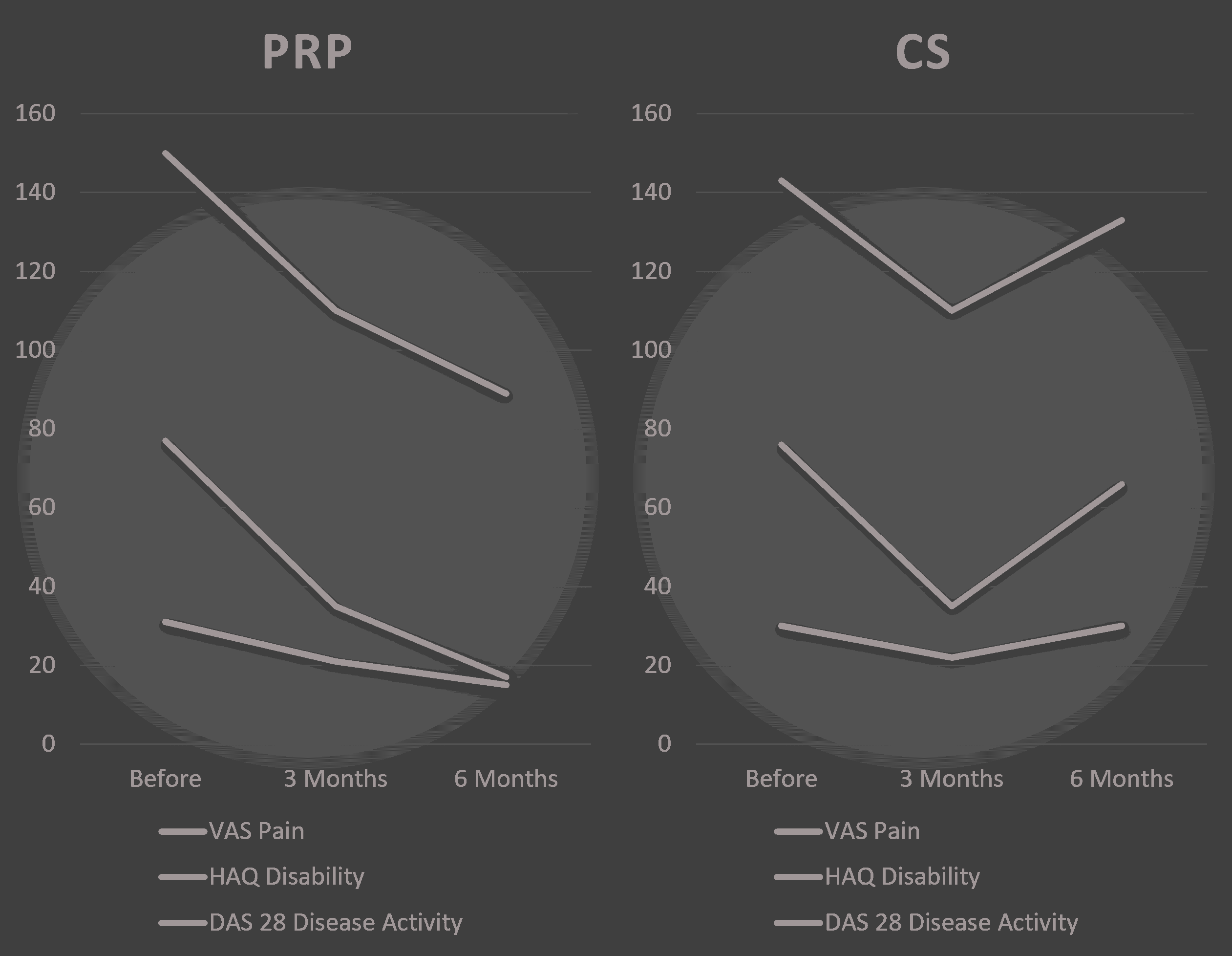
Above I took the three metrics reported and normalized them so they could all appear on the same graph. The VAS pain score is shown as 0-100, the HAQ disability score was multiplied by 100, and the DAS 28 disease activity score was multiplied by 10. As you can see, steroid injections (CVS) worked well at 3 months and then bounced back to about pre-injection baseline by 6 months. The PRP did much better at 6 months than at 3 months. These results mirror those reported by others in RCTs comparing PRP to CS injections.
Can PRP Drop Systemic Inflammatory Markers?
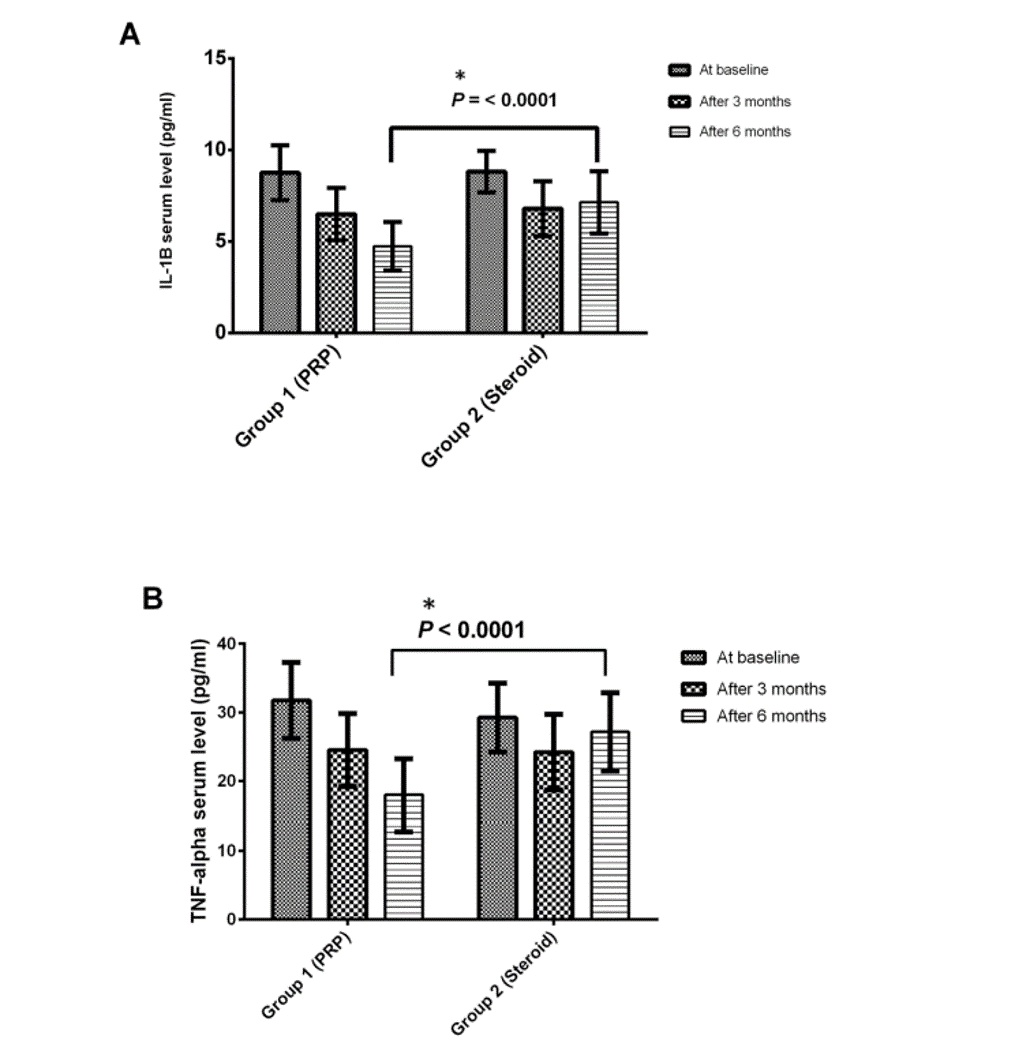
Proinflammatory markers are elevated in patients with rheumatoid arthritis, given that the disease impacts the whole body. These cytokines are one of the things believed to cause joint distruction. Hence, with multiple joints being injected, it was reasonable for the study authors to determine if PRP injected into the biggest problem joints was able to reduce these blood markers. What did they find?
PRP injections were more effective at lowering IL1-b and TNF-a blood levels than steroids. If you look at the measured levels above, IL1-b levels dropped about 40% by 6 months in the PRP group, well beyond the standard error range, while the CS patients had a negligible drop in that marker within that range. The decreases in TNF-a were even more impressive, with drops of about 50% for the PRP group compared to no significant decrease in the CS group.
What Could Be Accomplished with Higher Dose PRP?
While the PRP injections here were high-dose enough to classify as PRP (meaning that this wasn’t fake PRP under 2X concentration), they weren’t optimized. The age ranges in this study were from 39-62 years old with means from 47 to 55 years. That means that based on the in-vitro data, 15-20X concentrated PRP would likely perform better than the approximately 3X used.
This Study Is a Big Deal
The fact that we have high-level data now that PRP can both reduce pain and increase function in RA patients who are taking DMARD drugs is a very big deal. It’s an even bigger deal that the PRP again trounced the standard of care CS injections and reduced serum inflammatory cytokines. Why?
First, the thought has been that the anti-inflammatory DMARD drugs may be a non-starter for PRP in that they would block the needed acute inflammatory response. Second, we know that serum proinflammatory markers are directly linked to disease activity (2). Hence, if PRP lowers these markers, that may be a net positive gain for the patient. Third, we know CS injections destroy cartilage, so avoiding them in a disease that also destroys cartilage is a good thing (3).
The upshot? I now feel comfortable recommending PRP injections for RA patients. It will be interesting to see what kind of effects are possible once the doses are shited higher to compensate for the advanced age of most people with RA.
________________________________________
(1) Saif DS, Hegazy NN, Zahran ES. Evaluating the Efficacy of Intra-articular Injections of Platelet Rich Plasma (PRP) in Rheumatoid Arthritis Patients and its Impact on Inflammatory Cytokines, Disease Activity and Quality of Life. Curr Rheumatol Rev. 2021;17(2):232-241. doi: 10.2174/1573397116666201113090629. PMID: 33185167.
(2) Altomonte L, Zoli A, Mirone L, Scolieri P, Magaró M. Serum levels of interleukin-1b, tumour necrosis factor-a and interleukin-2 in rheumatoid arthritis. Correlation with disease activity. Clin Rheumatol. 1992 Jun;11(2):202-5. doi: 10.1007/BF02207957. PMID: 1617893.
(3) Wernecke C, Braun HJ, Dragoo JL. The Effect of Intra-articular Corticosteroids on Articular Cartilage: A Systematic Review. Orthop J Sports Med. 2015 Apr 27;3(5):2325967115581163. doi: 10.1177/2325967115581163. PMID: 26674652; PMCID: PMC4622344.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
