Can the Fox Guard the Henhouse? Why Putting Surgeons In Charge of Reducing Surgical Rates is a Bad Idea

Credit: Shutterstock
My mother loved her homespun idioms. One of those was that you could never put the fox in charge of the henhouse. This week a Regenexx corporate salesperson was trying to explain to a corporate client why putting a famous orthopedic clinic in charge of using interventional orthobiologics to reduce surgeries was a bad idea. So let’s explore that and look at why my mother’s sayings were usually prophetic.
Molasses in January
My mother loved to turn a phrase. In addition to the fox and the henhouse, another one was “Slow as molasses in January” (usually referring to how her kids were moving to get something done). Growing up in South Florida and never having actually seen any molasses, while I knew the concept, it wasn’t until later in life when I moved to Colorado and actually saw molasses that I truly understood. That’s why the fox and the henhouse stuck in my head when I got a call from one of our corporate salespeople.
Regenexx Corporate Program
The goal of our corporate program is to take patients who are usually considered surgical candidates and move them to interventional orthobiologics. For example, an ACL tear that’s complete, but non-retracted would get a Perc-ACL procedure using their own bone marrow concentrate under precise fluoroscopic guidance rather than an ACL Reconstruction surgery. Or a patient who was told they needed a low back fusion would get a platelet-based DDD injection procedure instead of that surgery. As with any disruptive technology, there are winners and losers.
If you’re a surgical practice, the money is made by performing surgeries. In fact, in most orthopedic surgery practices about 90% of the total revenue is generated that way. Add in ownership of out-patient surgery centers and payments from the medical device manufacturers who make surgical tools and implants and even a small decrease in the number of surgical cases being scheduled can cause massive financial problems.
Based on our almost two-decade experience with using interventional orthobiologics, about half or more of current elective orthopedic surgery patients could be successfully moved to these non-surgical procedures and avoid the knife. Even if we take a conservative one-third of current surgical cases getting placed into this non-surgical bin, that would cause massive financial disruption for the average orthopedic surgery practice as that means fewer surgeries, partially empty expensive ambulatory surgery centers (ASCs), and far fewer device payments from manufacturers.
In addition, since 99% of orthopedic surgeons have no training in these complex interventional procedures that use x-ray and ultrasound guidance, it means hiring physicians who understand how these are done and letting go of surgeons due to declining surgery rates. That in and of itself will upset the surgical applecart (another one of my mother’s sayings).
Why Can’t We Put the Fox in Charge of the Henhouse?
A corporate client recently told one of our salespeople that he had a famous orthopedic sports medicine clinic close by, so why couldn’t they just use that site to get interventional orthobiologics? After all, this is one of the most famous places in the west where many athletes get their surgeries performed. In addition, the clinic claimed they could do these interventional procedures! Let’s explore why this constitutes putting the fox in charge of the henhouse and is a very bad idea.
As discussed above, what incentive does this orthopedic surgery practice have to move patients from the surgical to the non-surgical column? For example, every patient that is moved away from surgery gets rid of a surgical fee and an ASC payment, as these interventional procedures are performed in sophisticated office-based procedure rooms and not in a surgery center. In addition, the orthopedic surgery clinic has no in-office fluoroscopy or specialized procedure rooms and no physicians who understand how to perform these procedures, so any procedures they decide to perform will be done poorly at great expense in the hospital ambulatory surgery center joint venture.
Ultimately, what will happen is that the orthopedic surgeons at this famous sports medicine practice will begin to add the cost of these interventional procedures to their surgeries. Few surgeries will ever get replaced as there is zero incentive to perform these non-surgical procedures at a level of sophistication that can replace surgery. Making this exercise cost plus rather than cost minus.
No Utilization Management
Regenexx has two decades of experience in interventional orthobiologics and runs the world’s largest registry tracking patient outcomes for these procedures. Hence, based on that data and what’s been published, we know when an interventional orthobiologics procedure will help replace surgery and what doesn’t work. As a result, all procedures must be approved by our utilization management system as being likely to save the employer money by avoiding surgery. The orthopedic clinic has no such ability or data and wouldn’t know which procedures are likely to replace surgery and which are likely to fail. This free for all will add cost to the employer’s health plan.
Experts in Interventional Orthobiologics?
Given that this was a famous orthopedic sports medicine clinic, they claimed to the employer that they knew what they were doing with these non-surgical procedures. To test that claim, I looked at the total number of patients that the clinic had published in medical journals who had received these procedures versus that number for Regenexx:
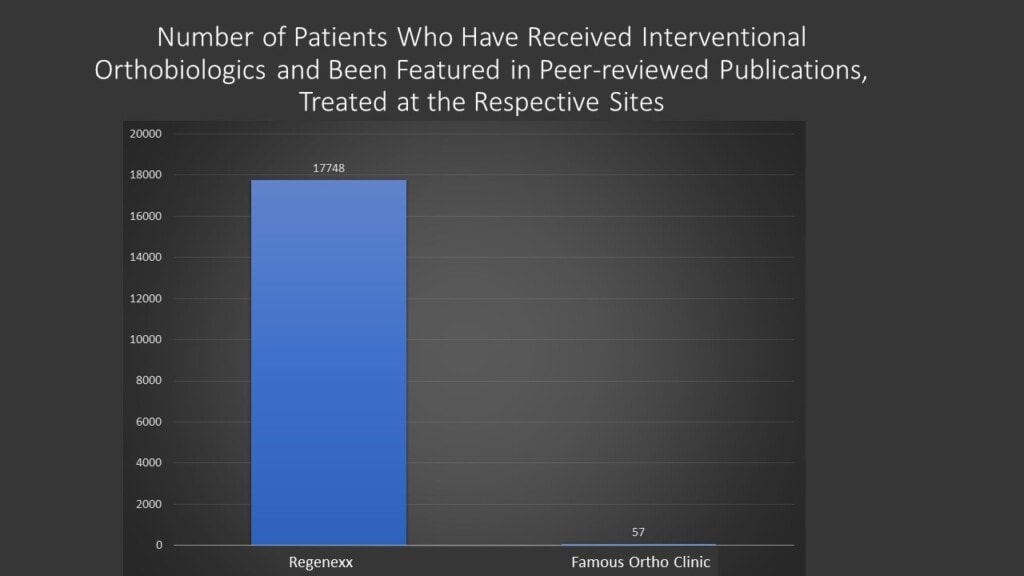
That 57 patients on the famous ortho clinic side is actually an overestimate as they were involved in a few PRP studies that were done at a few sites with all of those patients likely not being treated at that clinic. As you can see from the comparison, even with that over-estimate, the Regenexx side shows world-class expertise in interventional orthobiologics versus a clinic that doesn’t know which end is up.
A New Trend?
The competition in the orthopedic surgery market in many cities is fierce. Why? Obamacare forced rapid and massive consolidation of many clinical practices with orthopedic surgery groups being forced to partner with local hospitals. For example in our market, we have the University of Colorado battling two main hospital groups, each with an orthopedic surgery group that wants a piece of that profitable market. This often leads to irrational decision-making. For example, all three of these Denver-based groups have opened sites in the sparsely populated mountains that are separate from their Denver offices. That has prompted local orthopedic surgery groups there to open more mountain offices in more tiny communities to fend off the “Denver invasion”. All of that activity increases pressure on these groups to maximize revenues despite declining surgery reimbursement rates. Hence, it’s not surprising that all of these groups, not only here, but nationally, would love to convince employers that they can use interventional orthobiologics to replace surgeries. Or said another way, “Trust me, as the fox I can guard the henhouse and I promise not to eat too many chickens.”
The upshot? As usual, my mother was right. you can’t have the fox guard the henhouse and expect that to work out well. Orthopedic surgery practices can never be responsible for overseeing their own disruption. In many ways, that would be like believing that taxi companies can oversee a ride-sharing app like Uber. Entrenched industries always protect the status quo.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
