Carpal Tunnel Surgery Recovery
Carpal tunnel surgery recovery is critical to understand BEFORE you sign up for the surgery. Understanding the recovery timeline is all about knowing how the procedure is performed and whether you’re a candidate for newer, less invasive, and regenerative options. So let’s dig in.
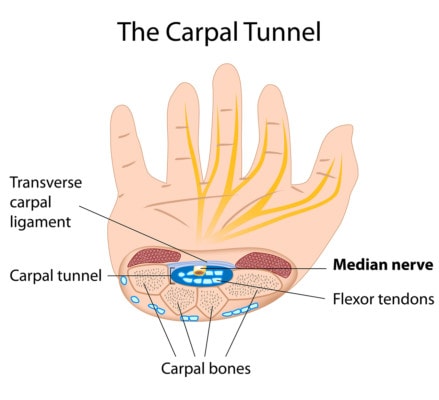
What Is the Carpal Tunnel?
Alila Medical Media/Shuttertock
There’s an area in your wrist where it meets the hand called the carpal tunnel. Tendons go though this area which gets tightest at the transverse carpal ligament which serves as the “roof” of the tunnel. The median nerve also goes through here and when it gets compressed or irritated, this can cause carpal tunnel syndrome. About 4% of adults will get this problem at some point (1).
What Is Carpal Tunnel Surgery?
Carpal tunnel surgery usually involves cutting the roof of the carpal tunnel which is made up of the transverse carpal ligament. There are many different ways this can be accomplished including using open surgery, endoscopically, or using ultrasound and a cutting device. There are also newer solutions such as nerve hydrodissection which don’t involve cutting the ligament but attempt to free up scar tissue around the nerve and reduce the swelling. How the procedure is done usually determines the carpal tunnel surgery recovery time.
Should I Have Carpal Tunnel Surgery?
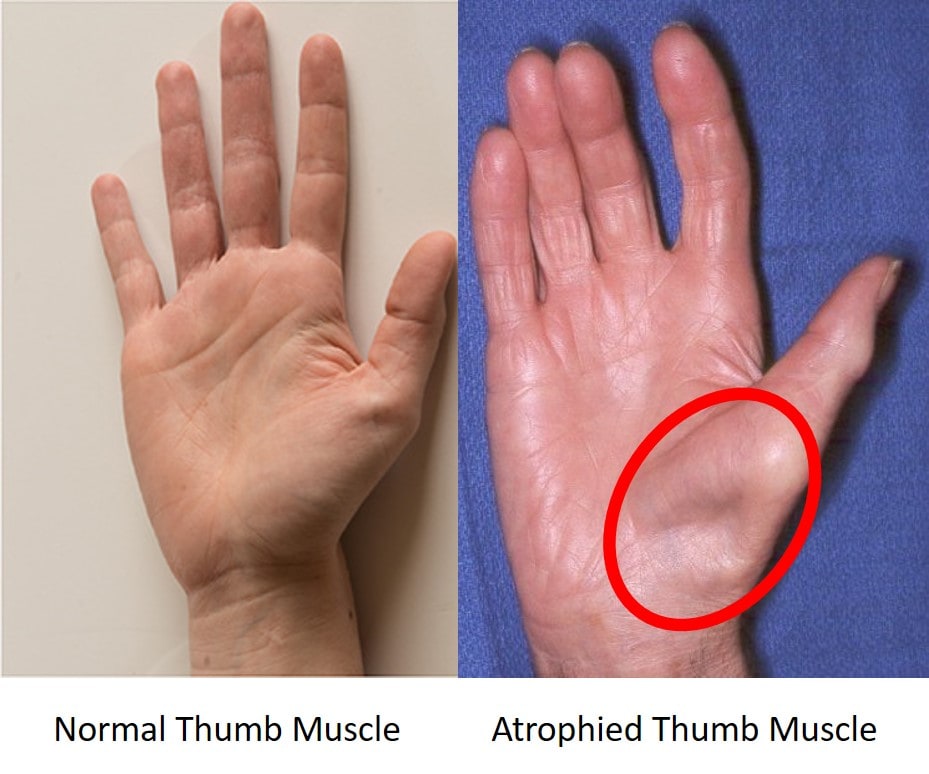
Who absolutely needs carpal tunnel surgery? Basically, if you have wasting of the muscle at the base of the thumb, then you likely need surgery. This means that the APB (Abductor Pollicis Brevis) muscle has gotten smaller than your other side. This problem is caused by the median nerve irritation in the carpal tunnel killing off muscle fibers.
If you just have numbness in the thumb and index finger with or without cramping in the thumb area, you likely don’t need surgery. Physical therapy may help. If that doesn’t work, then a newer technique called nerve hydrodissection may be helpful. See my video below for what that ultrasound-guided procedure looks like.
What Are Different Types of Carpal Tunnel Procedures?
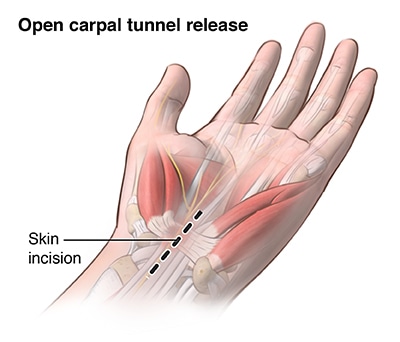
Open Surgery
In this procedure, the surgeon makes a traditional incision over the wrist. The transverse carpal ligament is then cut and the incision is closed. There are a few advantages, but one of them is not invasiveness, as this is the procedure with the most tissue damage.
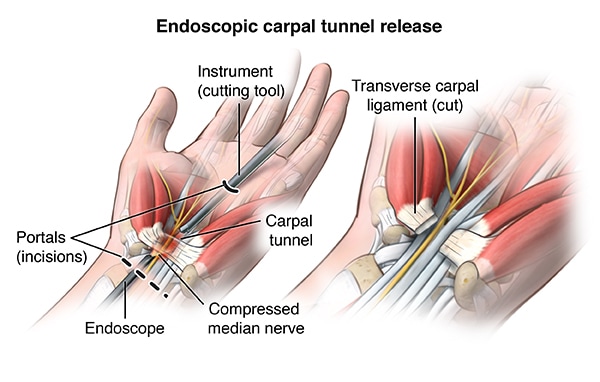
Endoscopic Surgery
In this procedure, the surgeon uses an endoscope to look at the nerve, tendons, and ligament (2). The ligament is cut through that small hole using instruments. The advantage is that there is less tissue damage. The disadvantage is that this is still surgery.
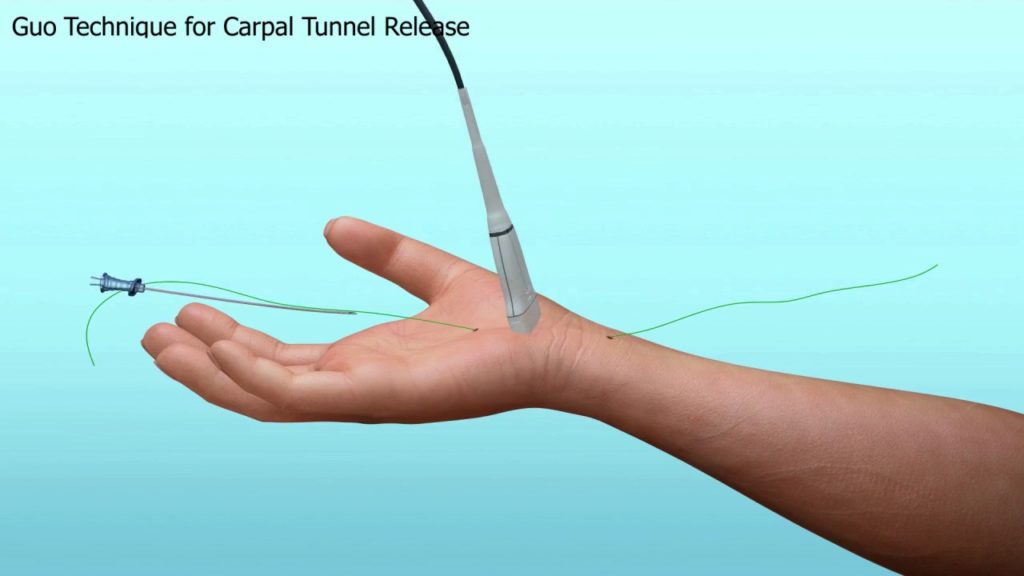
Ultrasound-guided Release
Here the doctor uses an ultrasound machine to see the ligament, tendon, and nerves and uses a specialized device to cut the ligament (5). This is less invasive than endoscopic carpal tunnel release. There are many different devices and tools used.
Nerve Hydrodissection Without Cutting the Ligament
This procedure is different than the other three, in that the transverse carpal ligament is not cut. Why? Cutting the ligament can cause wrist instability (too much movement in the carpal bones) (4). This problem can lead to long-term pain and arthritis in the wrist.
Here the doctor uses ultrasound guidance to image the nerve and tendons and inject either steroid or platelet based growth factors around the nerve (9). The goal is to break up scar tissue and free up the nerve while also reducing swelling in the surrounding tendons. This is the least invasive of the procedures discussed here.
What Can I Expect after Carpal Tunnel Surgery and Recovery?
Carpal tunnel surgery recovery times and pain and disability after surgery are linked to the invasiveness of the procedure. More invasive means more recovery time while less invasive generally means a quicker recovery. Let’s review some facts based on what’s published.
The average time to return to normal daily activities was 16 days for endoscopic release patients whereas it took 20 days to return to normal activities in open surgery patients.
1-Month
Open surgery – A head to head trial showed that 45% of patients had relief by 3 days. 55% of patients with open surgery were better in one month.
Endoscopic Surgery – 57% of patients had early relief while 63% had complete relief of symptoms after one month (3).
6-Months
66% of patients who had open surgery and 77% of patients with endoscopic release showed complete relief by 6-months.
For ultrasound-guided release, data at different time points isn’t available, but functional scores showed that recovery times were similar to endoscopic release (6). In addition, there was no residual scar pain which was reported in about half of patients undergoing an open procedure (7)
Given that nerve hydrodissection without cutting the ligament isn’t surgical and instead is a highly precise injection, it’s expected that return to activities, work, and recovery would be the fastest of all of these procedures, but the recovery timeline data is still being reported for this newer technique.
How Long Are You Out of Work after Carpal Tunnel Surgery?
Time off from work varies by procedure. Return to work was reported at 30 days for open surgery and 15 days for endoscopic. (8)
What Are the Side Effects of Having Carpal Tunnel Surgery?
Side effects include (10):
- Infection
- Nerve damage
- Instability in the wrist bones due to cutting a critical ligament
- Failure of the procedure to relieve symptoms
- Pain at the surgical site scar
One large study looking at many trials concluded that there is a greater risk of non-serious nerve injury (about 3X greater) with the endoscopic release versus open surgery, but less chance of scar pain and earlier return to work. (11).
The Newest Technique
We have been successfully using a Perc-Carpal Tunnel Orthobiologic Scar Release (Perc-CT SOR Procedure) for many years with excellent results. It’s similar to the ultrasound-guided carpal tunnel hydrodissection procedure described above, but instead of using the high-dose steroid which can hurt nerves and tendons (18,19), we use the patient’s own platelet-derived growth factors that can help nerves heal through cytokines like NGF, PDGF, and IG-1 (13, 17).
The use of the patient’s own platelets has been shown to be superior to steroid shots in the treatment of carpal tunnel syndrome (12, 16). PRP has also been shown to superior to using another commonly injected substance called D5W (14). Others have also found good results with this platelet based injection technique (15).
To see a video of what this looks like, see below:
Recovery time is minimal and patients have very little if any downtime.
The upshot? There are many options for surgery and each has a different carpal tunnel surgery recovery timeline. Hence, do your research and choose wisely!
___________________________________
References:
(1) Ibrahim I, Khan WS, Goddard N, Smitham P. Carpal tunnel syndrome: a review of the recent literature. Open Orthop J. 2012;6:69–76. doi: 10.2174/1874325001206010069
(2) Schmelzer RE, Della Rocca GJ, Caplin DA. Endoscopic carpal tunnel release: a review of 753 cases in 486 patients. Plast Reconstr Surg. 2006 Jan;117(1):177-85. https://www.ncbi.nlm.nih.gov/pubmed/16404264
(3) Malhotra R, Kiran EK, Dua A, Mallinath SG, Bhan S. Endoscopic versus open carpal tunnel release: A short-term comparative study. Indian J Orthop. 2007;41(1):57–61. doi: 10.4103/0019-5413.30527
(4) Vanhees M, Verstreken F, van Riet R. What does the transverse carpal ligament contribute to carpal stability?. J Wrist Surg. 2015;4(1):31–34. doi: 10.1055/s-0034-1398486
(5) Petrover D, Silvera J, De Baere T, Vigan M, Hakimé A. Percutaneous Ultrasound-Guided Carpal Tunnel Release: Study Upon Clinical Efficacy and Safety. Cardiovasc Intervent Radiol. 2017;40(4):568–575. doi: 10.1007/s00270-016-1545-5
(6) Petrover D, Silvera J, De Baere T, Vigan M, Hakimé A. Percutaneous Ultrasound-Guided Carpal Tunnel Release: Study Upon Clinical Efficacy and Safety. Cardiovasc Intervent Radiol. 2017;40(4):568–575. doi: 10.1007/s00270-016-1545-5
(7) Gong HS, Baek GH, Oh JH, Lee YH, Jeon SH, Chung MS. Factors affecting willingness to undergo carpal tunnel release. J Bone Joint Surg Am. 2009;91:2130–2136. doi: 10.2106/JBJS.H.01221.
(8) Jugovac, N. Burgić, V. Mićović, et al. Carpal tunnel release by limited palmar incision vs. traditional open technique: randomized controlled trial. Croat Med J, 43 (2002), pp. 33-36. https://www.ncbi.nlm.nih.gov/pubmed/11828556
(9) Guo K, McCool L, Wang H, Guo D, Guo D. The Modified Ultrasound-Guided Distal-to-Proximal Carpal Tunnel Injection With Median Nerve Hydrodissection: A Retrospective Safety Review of 827 Procedures. Hand (N Y). 2019 Jul 9:1558944719861715. doi: 10.1177/1558944719861715.
(10) Karl JW, Gancarczyk SM, Strauch RJ. Complications of Carpal Tunnel Release. Orthop Clin North Am. 2016 Apr;47(2):425-33. doi: 10.1016/j.ocl.2015.09.015.
(11) Sayegh ET, Strauch RJ. Open versus endoscopic carpal tunnel release: a meta-analysis of randomized controlled trials. Clin Orthop Relat Res. 2015;473(3):1120–1132. doi: 10.1007/s11999-014-3835-z
(12) Senna MK, Shaat RM, Ali AAA. Platelet-rich plasma in treatment of patients with idiopathic carpal tunnel syndrome. Clin Rheumatol. 2019 Aug 16. doi: 10.1007/s10067-019-04719-7.
(13) Sowa Y, Kishida T, Tomita K, Adachi T, Numajiri T, Mazda O. Involvement of PDGF-BB and IGF-1 in activation of human Schwann cells by platelet-rich plasma. Plast Reconstr Surg. 2019 Aug 27. doi: 10.1097/PRS.0000000000006266.
(14) Shen YP, Li TY, Chou YC, Ho TY, Ke MJ, Chen LC, Wu YT1. Comparison of perineural platelet-rich plasma and dextrose injections for moderate carpal tunnel syndrome: A prospective randomized, single-blind, head-to-head comparative trial. J Tissue Eng Regen Med. 2019 Jul 31. doi: 10.1002/term.2950.
(15) Güven SC, Özçakar L, Kaymak B, Kara M, Akıncı A. Short-term effectiveness of platelet-rich plasma in carpal tunnel syndrome: A controlled study. J Tissue Eng Regen Med. 2019 May;13(5):709-714. doi: 10.1002/term.2815.
(16) Uzun H, Bitik O, Uzun Ö, Ersoy US, Aktaş E. Platelet-rich plasma versus corticosteroid injections for carpal tunnel syndrome. J Plast Surg Hand Surg. 2017 Oct;51(5):301-305. doi: 10.1080/2000656X.2016.1260025.
(17) Sánchez M, Anitua E2, Delgado D, Sanchez P, Prado R, Orive G, Padilla S. Platelet-rich plasma, a source of autologous growth factors and biomimetic scaffold for peripheral nerve regeneration. Expert Opin Biol Ther. 2017 Feb;17(2):197-212. doi: 10.1080/14712598.2017.1259409.
(18) Halpern AA, Horowitz BG, Nagel DA. Tendon ruptures associated with corticosteroid therapy. West J Med. 1977;127(5):378–382. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1237870/
(19) Mackinnon SE, Hudson AR, Gentili F, Kline DG, Hunter D. Peripheral nerve injection injury with steroid agents. Plast Reconstr Surg. 1982 Mar;69(3):482-90. https://www.ncbi.nlm.nih.gov/pubmed/7063571

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.