Chiari Malformation Treatment – Do You Need Surgery?
I often see patients after surgical Chiari malformation treatment. Many actually have craniocervical instability causing their problems, but mistakenly get Chiari surgery and don’t do well. In fact, I just spoke to one of these patients this week on a Telemedicine consult. I tried to explain to her that this is a procedure with significant collateral damage, so I thought it was time for a blog on the topic.
What Is Chiari Malformation?
Chiari malformation occurs when the brain pushes down through the hole in the base of the skull called the foramen magnum. This can cause pressure on the back of the brain (cerebellum) and/or the brain stem. This can lead to a host of symptoms:
- Neck pain
- Balance problems, dizziness, or vomiting
- Muscle weakness or numbness
- Difficulty swallowing or speaking.
vomiting - Ringing or buzzing in the ears (tinnitus)
The biggest concern is that these symptoms overlap with many other problems. For example, patients with upper neck facet joint injuries get neck pain, balance issues, and other symptoms. Patients who have craniocervical instability (CCI) often have all of the above symptoms. Hence, having an MRI suggestive of a Chiari malformation and these symptoms does NOT mean the next step is invasive surgery.
Types of Chiari Malformation
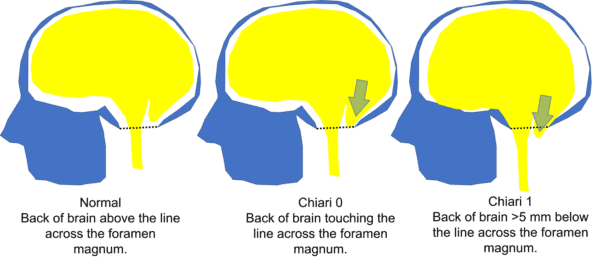
Where the rubber meets the Chiari road is which type of malformation is present. The least severe is actually not listed in the above pictures because it’s more controversial, which is often called Chiari 0 or cerebellar ectopia. Few physicians would argue that if you have a portion of your brain that has herniated downwards than you may have a very real need for Chiari malformation treatment through surgical decompression (Chiari 1 or 2 as shown above). However, all too often these days, patients get operated on for Chiari 0 without a frank lower brain herniation, which is the focus of this blog.
Chiari 0 or CTE (Cerebellar Ectopia)
First, Chiari 0, or Cerebellar Tonsillar Ectopia (CTE), is when the back of the brain (cerebellum) isn’t really herniating down through the bottom hole in the skull. Instead, it’s “on the line” of pushing down and out of the skull or has done so just slightly. All of this is much less severe than Chiari 1, which means that surgery for Chiari 0 is very controversial. For example, we don’t have a huge body of research that shows that this MRI finding is associated with symptoms (2).
My colleagues and I performed a research study many years ago which looked at how many cerebellar ectopia or Chiari 0 patients could be found on upright MRI imaging after car crashes (1). We found that about 1 in 5 patients with chronic pain after a car crash had this issue. The question was whether this was causing their symptoms, or an upper neck injury, as many of these patients also had evidence of CCI. Meaning that the ligaments that held their head on had been injured and that the Chiari 0 was being caused by that ligament injury.
Surgery for Chiari 0
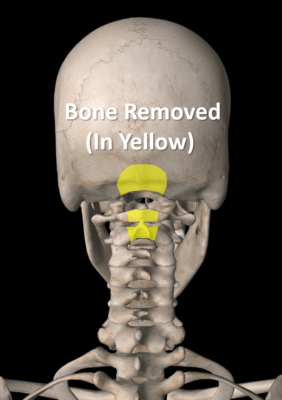
Chiari malformation treatment often involves surgery. The goal is to remove bone and “decompress” the area of the brain with pressure. That means opening the skin, retracting back the muscles, and then removing the bone shown here in yellow. This is often the back of the skull and the back of the c1 and/or C2 vertebrae (if needed). The skull bone removal procedure is called a posterior fossa decompression.
Complications from this procedures are substantial (3). They include more than 1 in 10 of the patients having a dural leak. This means that the doctor cuts through the covering of the brain and spinal cord (the dura) which is the sac containing cerebrospinal fluid in which the brain floats. The dura is then sewn back up and leaks, often requiring another surgery. Other common complications include 9% who get an infection of the brain (meningitis), infected wounds at 7%, and damaged nerves in 5%. About 3% of the patients die from the surgery.
What Is the Collateral Damage?
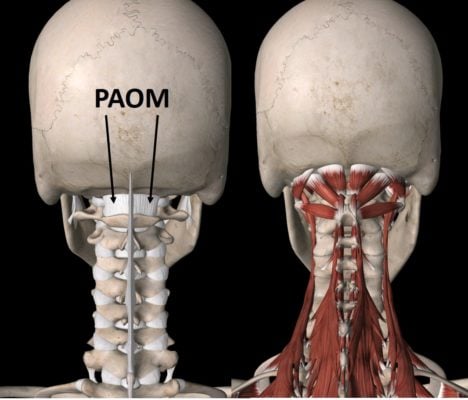
However, a much bigger deal with this surgery, even beyond the very serious complications that could happen, is the collateral damage. To understand that, we need to review the critical anatomy in this area. In the image shown here, note that the PAOM is a ligament in the back of the neck that helps to keep the skull stable on the neck as you look down. Then note the myriad of muscles in the upper neck at the base of the skull. They’re responsible for maintaining your head stability on your neck. Both this ligament and many of these muscles are destroyed when a posterior fossa decompression surgery is performed. Why is this a big deal?
Permanent Bobblehead
This ligament and these muscles at the back of the upper neck and skull are critical for stabilizing your head on your neck. Think of the head as a bowling ball at the end of a stick (your neck). Without an important piece of duct tape (the PAOM ligament) or the muscles that actively balance the bowling ball on the stick, you can become a permanent bobblehead. Hence, outside of huge fusion surgery to bolt all of this together, there is no way to fix the collateral damage done by this aggressive surgical Chiari malformation treatment.
My Patient
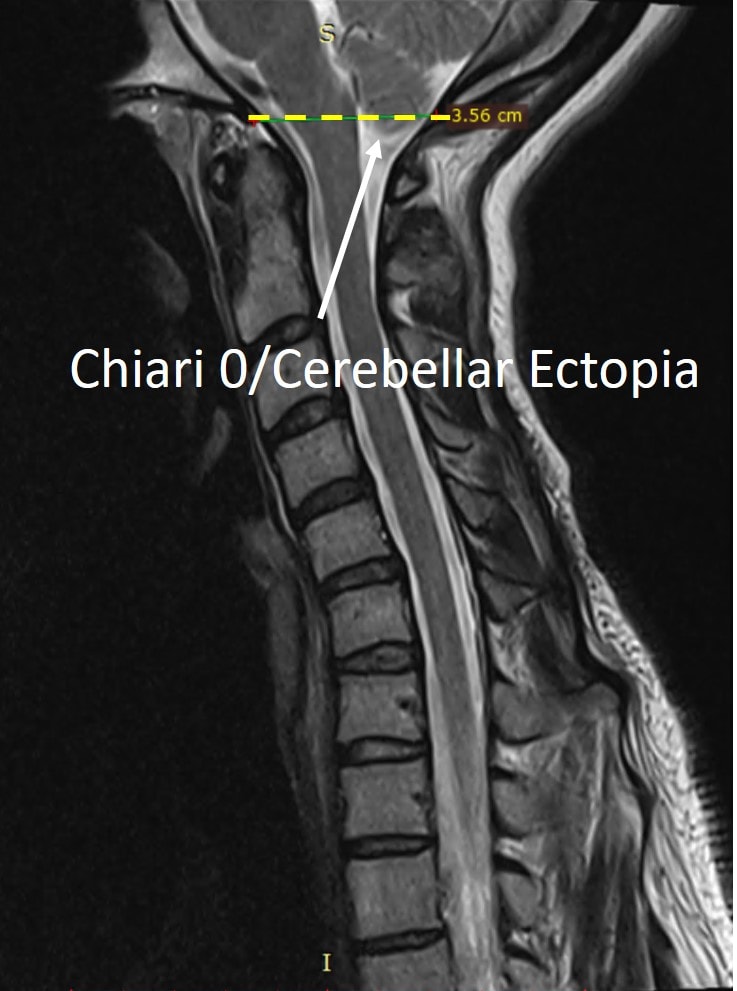
This is my patient’s MRI to the left. It shows a Chiari 0 or cerebellar ectopia, meaning that she doesn’t have a Chiari 1 with a good chunk of her lower brain having herniated through the bottom of the skull and into the spinal canal. Instead, the surgeon believed that pressure on the lower part of the brain (the cerebellar tonsils) was causing her symptoms. She therefore, underwent a posterior fossa decompression at great personal risk. This didn’t help any of her symptoms which primarily include balance problems, neck pain, and brain fog. She was then later diagnosed with craniocervical instability (CCI) by a neurosurgeon in Spain who wants to now fuse C0-C2 (the skull to her upper neck bones) and her lower neck to boot. She wisely said no and began to explore other options.
Ultimately, she’s likely a candidate for a much less invasive PICL procedure to help tighten down upper neck ligaments damaged while she was playing volleyball many years ago. However, I had to tell her that since the PAOM ligament and many upper neck muscles are no longer there because of the surgical Chiari malformation treatment she has already had, our less invasive injection procedure may fail. So while I have hopes that I can help her and the PICL procedure is less invasive than the planned fusion, because of the collateral damage from surgery, it could be too late. For information on the PICL procedure to help tighten damaged upper neck ligaments without invasive surgery, see below:
The upshot? I wanted to get this blog out to discourage other CCI patients from persuing surgical Chiari malformation treatment. This is a big surgery with big complications, but more importantly, the collateral damage that the procedure causes can be epically bad, and can limit less invasive treatment options. So please think twice before getting this procedure!
_____________________
References:
(1) Freeman MD, Rosa S, Harshfield D, Smith F, Bennett R, Centeno CJ, Kornel E, Nystrom A, Heffez D, Kohles SS. A case-control study of cerebellar tonsillar ectopia (Chiari) and head/neck trauma (whiplash). Brain Inj. 2010;24(7-8):988-94. doi: 10.3109/02699052.2010.490512.
(2) Furuya K, Sano K, Segawa H, Ide K, Yoneyama H. Symptomatic tonsillar ectopia. J Neurol Neurosurg Psychiatry. 1998;64(2):221–226. doi:10.1136/jnnp.64.2.221
(3) Dubey A, Sung WS, Shaya M, Patwardhan R, Willis B, Smith D, Nanda A. Complications of posterior cranial fossa surgery–an institutional experience of 500 patients. Surg Neurol. 2009 Oct;72(4):369-75. doi: 10.1016/j.surneu.2009.04.001. Epub 2009 Jul 14.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
