Do You Have PRP Derangement Syndrome (PDS)?

Credit: Shutterstock
I’ve documented through the years that while some forward-thinking orthopedic surgeons have embraced using PRP, many have an irrational disdain for it. This is such a bizarre juxtaposition of the evidence that I call this PDS (PRP Derangement Syndrome). Today we’ll review a recent study that proves this point. Let’s dig in.
What is PRP?
PRP stands for platelet-rich plasma and if you want a quick refresher as to what this is, see my video below:
Orthopedic Surgeons and PRP
The good news is that we’ve seen an increasing number of orthopedic surgeons begin to embrace using PRP. While most of these providers do this poorly with very little injection expertise (and a handful of orthopedists have learned how to do it well), it’s a start toward the wider acceptance of this type of basic regenerative medicine treatment. However, despite this progress toward eliminating disease, we still see evidence out there of some serious cases of PDS.
This Week’s PDS Piece from the Journal of Arthroplasty
Arthroplasty means joint replacement and in a very real way, PRP competes with joint replacement surgery. For patients with early to mid-stage arthritis, some of whom at an early age are now being declared knee replacement candidates, the research shows that PRP works very well. Hence, if you’re a joint replacement surgeon, you may not be happy about patients coming into the office to ask about PRP. If that unhappiness has developed into an irrational rage, you may have developed PDS.
How do we know PDS exists? Easy to find evidence exists in the orthopedic research journals. In fact, a PDS article was just published this week.
This new article is entitled, “Google Trends Analysis Shows Increasing Public Interest in Platelet-Rich Plasma Injections for Hip and Knee Osteoarthritis” (1). Basically, it looks like several joint replacement surgeons used a student to search various terms associated with knee osteoarthritis and PRP. They then used some simple stats to show that there was “a significant rise in Google queries related to platelet-rich plasma injections for osteoarthritis of the hip and knee since 2009“. That’s groovy, but it’s this statement in the abstract that was concerning, “One biologic therapy with mixed clinical and basic science evidence for treating osteoarthritis is platelet-rich plasma injections into the affected joint.” Why is this clear evidence the authors had PDS? Let’s dig in.
The Research on PRP Used to Treat Knee Arthritis
So is it true that the research on the use of PRP for knee arthritis is “mixed”? That statement means that we don’t have good evidence this stuff works. Since this is a journal for joint replacement surgeons, why don’t we start by looking at the research that supports knee replacement?
To date, we have one randomized controlled trial of knee replacement versus conservative care (physical therapy) (2). That’s it. There is no study comparing knee replacement to medications, saline placebo, or steroid injection. For a procedure that is responsible for 600,000 invasive surgeries a year (US only) and loads of morbidity, that’s just pitiful.
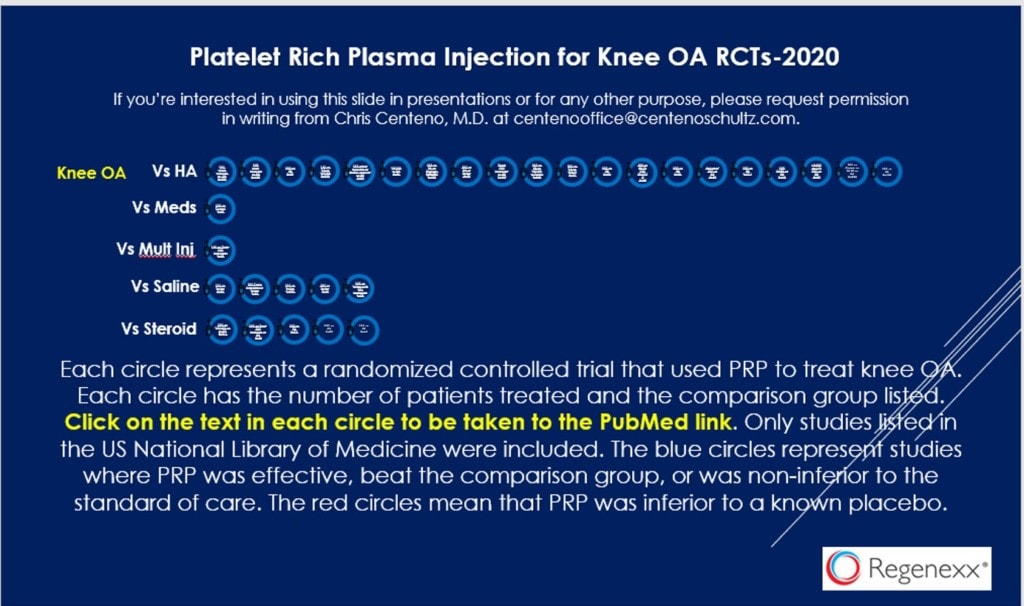
To see the PRP literature on knee arthritis, see my infographic above. Click on that image to get the PDF with links at each icon representing a study. Click like your life depends on it as actually taking the time to look at this document may be the beginning of your PDS treatment journey.
So how many PRP studies are there that show superiority over hyaluronic acid, the stuff that many of these surgeons with PDS use in their practices every day? TWENTY. Yep, that’s 19 more than support using knee replacement as a treatment. How many PRP studies showing superiority over placebo injections? FIVE. Given that there is no knee replacement study against a placebo, that’s 5 more than for knee replacement. How many RCTs show that PRP is better than steroid injections, which are used day in and out by surgeons with PDS? FIVE. Right now, we have 32 RCTs that show that PRP works for knee arthritis. Hence, the surgeons who wrote this article clearly have a severe case of PDS.
Heterogeneity
One of the signs that an orthopedic surgeon has PDS is when they claim that there are just too many different types of PRP being used, hence, we need more research. This is a PDS symptom called “heterogeneity”.
However, there are a few issues with this argument that demonstrate clear signs of PDS. First, with almost three dozen RCTs on PRP, this becomes less of an issue as there are only a few main types being used in these studies, so we’re likely to have several RCTs on each type. In addition, remember that there is only one RCT on knee replacement despite dozens of very different knee replacement prostheses being on the market. How’s that for heterogeneity? Meaning to support all of the knee replacement devices, we would need in total, hundreds of RCTs showing that knee replacement works.
Do You Have PDS?
If you’re an orthopedic surgeon you may want to take my quick quiz to see if you suffer from PDS:
- Do you think that the surgeries you perform have better level 1 evidence than PRP?
- Do you get uncontrollably angry when a patient comes into the office asking about PRP and wanting to delay or cancel their planned surgical procedure?
- Do you believe that PRP is a worldwide conspiracy?
If you answered “Yes” to any of the above, you may need to see a colleague about getting treated for PDS.
The upshot? If you think you have PDS, please seek treatment now! Delaying diagnosis and treatment of a serious illness is never a good thing.
___________________________________
References:
(1) Cohen S, et al. Google Trends Analysis Shows Increasing Public Interest in Platelet-Rich Plasma Injections for Hip and Knee Osteoarthritis. Journal of Arthroplasty. June 03, 2021 DOI:https://doi.org/10.1016/j.arth.2021.05.040
(1) Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, Rasmussen S. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med. 2015 Oct 22;373(17):1597-606. doi: 10.1056/NEJMoa1505467

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.